Abstract
Purpose and hypothesis
Shoulder lesions are common and a challenge to diagnose. They often result in significant disability for the patient and are an economic burden to society. From recent studies, an increasing incidence has been reported. The purpose of this study was to investigate and map the incidence of shoulder lesions in Denmark from 1996 to 2013 with focus on sex, age and geographical area.
Methods
The Danish National Patient Registry was searched retrospectively to find the number of shoulder lesions in Denmark during the period 1996–2013. Regional population data were retrieved from the services of Statistics Denmark. Incidence rates were analysed using Poisson regression models, and all analyses were done in R 3.2.2, and p values less than 0.05 were considered statistically significant.
Results
During the 18-year period, 244,519 patients with a DM 75 diagnosis were registered. Male-to-female ratio was 51:49, and median age was 51. Most frequent were rotator cuff syndrome with a mean incidence rate of 313.3 (confidence interval 241.8–384.8) per 105 person-years at risk (PYRS). A statistically significant increase in overall incidence rate from 149.4 per 105 PYRS in 1996 to 715.3 per 105 PYRS in 2013 was found (p < 0.01). Incidence was highest for men aged 51–70 (1085.1 per 105 PYRS in 2013). There was no significant difference in incidence between sexes. Rural areas had a 1.4-fold higher mean incidence rate than urban areas.
Conclusion
The incidence of shoulder lesions rapidly increased mainly due to an increase among people of working age (31–70 years). There were no significant differences in incidence between sexes. Rural areas had a 1.4-fold higher incidence rate than urban areas. As shoulder lesions impose a huge socioeconomic burden on society, not to mention a great distress to the patient, the present findings is highly relevant for political decision-making regarding preventive and health promoting initiatives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shoulder lesions are common and potentially debilitating. They constitute a high societal cost and occupational burden for workers [17]. The lesions are challenging to diagnose with a lack of clearly defined diagnostic criteria just as there is little overall evidence to guide treatment [21, 27].
The incidence of shoulder complaints in general practice varies and has been reported to be 9.5–14.2/1000 patients/year with rotator cuff-related disease being the most frequent [15, 29]. Shoulder problems account for 2.4% of all general practitioner consultations in the UK [8], and 4.5 million visit to the physicians annually in the USA [17]. It seems that the trend is raising, but little is known on the subject and most studies lack information on impact of sex, age and geographical variation, just as the course of treatment and treatment efficacy is unclear [1, 28].
Shoulder lesions include the diagnoses: adhesive capsulitis (i.e. “frozen shoulder”), rotator cuff syndrome, impingement, bursitis, bicipital tendonitis and calcific tendonitis, all belonging to the WHO ICD-10 category DM75. It is estimated that 65–70% of all shoulder lesions are due to rotator cuff disease [23] which has been regarded as a continuum that range from inflammation and impingement to full-thickness tears [12]. It will for the rest of the paper be called rotator cuff syndrome. There have been described intrinsic and extrinsic mechanisms of development [22], and age is a significant risk factor [6]. The cause of bicipital tendonitis is most often a secondary process related to continuing shoulder inflammation [10]. Calcifying tendonitis of the shoulder is usually a self-limiting disease, and the relationship between pain, calcific deposit and rotator cuff tears has not yet been fully understood [3, 25]. Adhesive capsulitis is a painful disease with a clinical presentation in three or four overlapping phases [13, 18] with a total duration of months to several years. It can be either primary (idiopathic) or secondary to, for example, trauma, surgery, rotator cuff syndrome or diabetes. Majority of patients are female, aged from 40 to 60 years [13, 19].
The purpose of this study was to investigate and map the incidence of degenerative rotator cuff-related shoulder lesions in Denmark from 1996 to 2013 with focus on sex, age, geographical area and type of hospital.
The hypothesis is that incidence is increasing and that mapping the incidence will aid political decision makers to identify areas of further investigation as a first step in preventive matters. To our knowledge, no previous study has examined all lesions comparative. We report national data from an 18-year period.
Materials and methods
The study was conducted as a retrospective registry study. National population data were compiled by extracts from the Danish National Patient Registry and services of Statistics Denmark.
Data acquisition
In Denmark, when patients seek medical care in the hospitals (both emergency room/walk-in consultation/hospitalized and whether in private or public hospital), they are registered with their unique person identifier, the social security number. At the end of treatment, a diagnosis is given. Danish legislation imposes hospitals to report data from all patient contacts to the Danish National Patient Register. From 1994, registration has been performed using the ICD-10 classification system.
The Danish National Patient Register was searched from 1 January 1996 to 31 December 2013. For patients registered under the ICD-10 code for shoulder lesions (DM 75), the following information was extracted: sex, age, municipality and type of hospital (public or private). National population data concerning sex, age and geographical population density were retained from the services of Statistics Denmark from 1996 to 2013 [26].
Included diagnose codes
Data were sorted according to the hierarchy of the ICD-10 coding system. The shoulder lesions were examined in the following groups: DM 75.0 (frozen shoulder), DM 75.1-DM 75.5 (rotator cuff syndrome: tear, tendinitis, impingement and bursitis) and finally DM 75.8–DM 75.9 (other/unspecified lesions). If a patient had both a specific diagnosis (i.e. DM 75.0–DM 75.5) and an unspecific diagnosis (DM 75, DM 75.8 or DM 75.9), only the specific diagnosis was included in the analyses. If a patient had more than one specific diagnosis, both were registered.
Interpretation of registered codes
To avoid overestimation of the incidence rates, a cut-off point of 180 days was established. Thus, if a patient was registered with a new diagnosis less than 180 days from a closed patient contact, the diagnosis was considered part of the already known course of disease and therefore not registered as a new event in the dataset. On the other hand, if a patient was registered with a new diagnosis more than 180 days from closed contact, it was considered evidence of a new shoulder lesion and would therefore be registered as a new lesion in the dataset.
Geographical area was defined as urban for municipalities with population of at least 80,000 in 2005 (the cities of Copenhagen, Aarhus, Odense, Aalborg, Frederiksberg and Esbjerg). All other areas were considered rural.
The study was approved by the Danish Data Protection Agency. According to Danish legislation, no IRB approval was needed, as the study is a retrospective registry study.
Statistical analysis
The primary outcome variable was the incidence of shoulder lesions. The incidence rate was calculated as the number of injuries divided by the person-years at risk (PYRS). The PYRS was defined as the sum of years people were at risk of having an incidence within each year. If persons did not die within the year, they contributed a year, and because of lack of exact death dates for the background population, it was assumed that if a person died at some point during that year, they contributed half a year.
Change in incidence rates was analysed using Poisson regression models. Models were fitted either with intercept only to estimate average incidence rates within the period 1996–2013 or with period variable to estimate average yearly change in incidence rates. Models also included age and sex grouping variables as well as geographical variables to estimate group specific incidence rates. Separate models for all diagnoses; rotator cuff and frozen shoulder were fitted.
Results were considered statistically significant if p values were less than 0.05, and all analysis was done using R 3.2.2. (R Foundation for Statistical Computing, Vienna, Austria).
Results
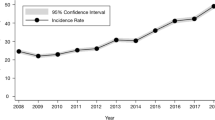
During the 18-year study period, 244,519 patients were registered with a DM 75 diagnosis, 51% male (N = 124,310) and 49% female (N = 120,209). Male-to-female ratio was 51:49. Median age was 51. The 244,519 patients had 303,077 unique contacts with the hospitals. Of these, 198,906 of the patients had one unique course of disease while 45,613 patients were registered with two or more courses of disease (Table 1). In total, 29,509 of the patients had a course of disease registered with a double diagnose (both rotator cuff syndrome and frozen shoulder). A statistically significant increase in overall incidence rate from 149.4 per 105 PYRS in 1996 to 715.3 per 105 PYRS in 2013 was found (p < 0.01) (Fig. 1). Incidence for men was 143.2 per 105 PYRS in 1996, which rose to 745.6 per 105 PYRS in 2013. Men aged 51–70 had the highest incidence with 1085.1 per 105 PYRS in 2013 while mean incidence for men was 413.5 per 105 PYRS (confidence interval (CI), 318.8–508.2 per 105 PYRS). Women had an incidence of 155.3 per 105 PYRS in 1996, which rose to 686 per 105 PYRS in 2013. Mean incidence for women was 387.0 per 105 PYRS (CI 299.2–474.9 per 105 PYRS) (Fig. 1). Most frequent for both sexes was rotator cuff syndrome with a mean incidence rate of 313.3 (CI 241.8–384.8) per 105 PYRS (Fig. 2). The incidence of rotator cuff syndrome showed a statistically significant increase of 465% (p < 0.01) in the study period. The incidence of frozen shoulder showed a statistically significant increase of 411% (p < 0.01) in the study period as well, for both men and women (Fig. 3). In 1996, incidences were 23.7 and 27.7 per 105 PYRS, respectively, while the rates had increased to 105.7 and 101.6 per 105 PYRS, respectively, in 2013, giving mean incidence rates of 68.0 per 105 PYRS (CI 53.7–82.3) for male and 64.1 per 105 PYRS (CI 50.7–77.4) for female. The higher incidence rate for men in 2013 was driven by an increase in the age group 51–70 (Fig. 3).
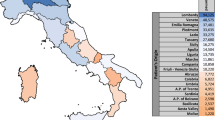
Geographical distribution of shoulder lesions changed over the study period (Fig. 4). In 1996, incidence was highest in the urban areas with 196 against 130 per 105 PYRS in rural areas. In 2013, the incidences had changed giving rural areas a 1.4-fold higher incidence of 774 against 561 per 105 PYRS in urban areas. Mean incidence rates were 326.1 (CI 262.5–389.7) and 426.0 (CI 324.1–527.9) for urban areas and rural areas, respectively. A statistically significant increase in incidence rate (p < 0.01) was found for both urban and rural areas (Fig. 4). The increase in incidence was greater in rural areas compared to urban (580% vs. 285%), and the increase was greatest for the elderly with a 717% increase in incidence for +71-year-olds in the rural areas.
Discussion
The most important findings of this study were the discovery of a dramatic surge in overall incidence rate in all diagnoses investigated mainly due to an increase in the age group 31–50 and 51–70 for both men and women, with men having the highest incidences. The predilection of shoulder lesions for people of working age is well known [5, 6], and our findings are consistent with this.
A recent study of impingement in an active duty US military population from 1999 to 2008 also found high incidence rates of 777 per 105 PYRS and an increasing incidence with age >40 [6]. Another study of patients with shoulder complaints in general practice found an incidence rate of 950 per 105 PYRS [15]. Thus, the incidence found in this study is on a par with what is reported elsewhere.
An explanation for the dramatic surge in incidence of shoulder lesions could reflect earlier underreporting, perhaps in combination with a greater focus on the disease due to easier accessibility to MRI and ultrasound which in the period investigated became more and more widely used. Some of the increase may be correlated with an increase in diagnostic possibilities. Also increasing pain awareness in present years could contribute to the rising incidence. However, if this was the case, one would expect to find the same increase within other frequent health complaints such as chronic back pain. A Danish report from 2007 concluded that the number of patients with back pain was constant (11–13%) in the years 1987–2000 after which the number increased up to 15% in 2005 [9]. A study from Austria investigated the prevalence of back pain throughout three decades based on national health surveys. They found a similar increase in prevalence in the period investigated with the highest prevalence of 32.9% reported in 2006/2007 [4]. An assumption is that a rise in shoulder and back pain both could reflect an increasing pain awareness and a growing willingness to report pain symptoms, thus leading to increasing number of patients receiving an actual diagnose. In the present study, however, we found the incidence of rotator cuff syndrome and frozen shoulder to increase with 465% and 441%, respectively, and a raise in pain awareness can only account for a small part of this.
Another explanation for the dramatic surge in shoulder lesions could be a change in work patterns and work-related problems. There is an agreement that work relating to heavy lifting, awkward postures and work with vibration or repetition increase the risk of developing shoulder lesions [11, 23, 24]. But also psychosocial factors seem to play a role [23, 24], and as such, it is difficult to assess the influence of type of work on the risk of developing work-related shoulder lesions. In the study period, the percentage of people working with traditional heavy shoulder-loading work in the building and construction industry did not increase [26], and therefore, it is unlikely that this is a contributing factor to the increasing incidence.
It is safe to assume that work involving computer and repetitive “mouse movements” has increased, even though no exact data can be extracted. A study from 2001 linked, among other things, unspecific shoulder pain to computer workers [16], but to our knowledge no study has examined a link between computer use and specific shoulder lesions. It requires further investigation to determine whether a link exists between computer use and shoulder lesions, and if so, it calls for preventive measures as computer use is a permanent part of a modern working life.
Incidence in the rural areas was found to be higher compared to urban areas in 2013. Strangely, overall incidence was highest in the cities in 1996. An explanation for this shift could be that new treatment algorithms and diagnoses gain acceptance in the cities first where the level of information is expected to be highest. Also, the shift could relate to manual labour, though there was not an increase in the study period; perhaps, the factories have moved out from the cities to the rural areas, leaving a higher proportion of manual labour in rural areas.
A contributing explanation for the drastic increase in incidence could be that some patients were counted more than once in the analyses. As described, patients were registered with all DM 75 sub-diagnoses, and thus, if a patient was thought to suffer from more than one condition, he/she would have more than one equal weighing diagnosis. In total, 29,509 patients had >1 diagnosis and were therefore counted more than once in the overall analysis of shoulder lesions. They were, however, only counted once in the analyses of rotator cuff syndrome and frozen shoulder. Only 12% of the patient population were registered like this and cannot account for an increase in incidence from 1996 to 2013 of several hundred per cent. Patients, who were cured for their complaints but returned more than 180 days after with a new complaint, were also counted twice in the incidence calculations. In total, 35,628 patients had two courses of disease and 9985 had more than two courses of disease. They account for less than 20% of the population, and again they cannot explain the dramatic increase in incidence.
The above-mentioned factors could contribute and partly explain an increasing incidence, but they cannot immediately account for the dramatic surge seen in the study period though computer work might play a greater role in development of shoulder lesions than previously assumed. Though the incidence is increasing, we know little of the impact on socioeconomic aspects since a diagnosis does not take severity of the disease into consideration. It calls for attention and further investigation in aetiology, consequences and preventive measures.
Frozen shoulder affected slightly more males than females in 2013, primarily due to an increase in incidence for men aged 51–70. The mean incidence rate was higher than elsewhere described [18]. A study of long-term outcome of frozen shoulders examined 269 patients and found women to be more affected than men (male-to-female ratio: 1.6:1.0) [5], but this does not seem to be the case in our nationwide cohort. It is known that there is a correlation with frozen shoulder and diabetes [7], and in the study period, the incidence of patients with diabetes doubled [2].
Since this study was a retrospective register study, it was inherently subject to the strengths and weaknesses of such. Denmark is an optimal setting for a nationwide epidemiological study and the Danish National Patient Register allows for acquisition of huge amount of data and a unique possibility to track a nationwide cohort over a long period [20]. Studies examining the validity of Danish National Patient Register has shown that the highest validity of the primary diagnose code is found in the orthopaedic coding with a positive predictive value of 83–89% [14].
However, it also imposes some serious limitations, as there is a risk of patients being incorrectly diagnosed hence being incorrectly registered and thus results in over- or underestimation. In the Danish National Patient Register, only data regarding age, gender, geographical location and type of hospital treated were retrievable, leaving no opportunity to access journals or previous scans among other things. This makes the present study vulnerable for confounders. The study was designed with a cut-off of 180 days from closed patient–hospital contact with >180 days marking a new event and thus a new registration. One can argue that a cut-off of >180 days is too narrow, having the lesions nature of protracted course of disease in mind, thus resulting in a new registration of the same lesion leading to an artificially high incidence rate. However, less than 20% of the patients had more than one course of disease over an 18-year long period, and thus, double registrations do not represent a big problem.
In regard to patients with degenerative shoulder lesions as a whole and for political decision makers, the findings of this study are highly relevant as a sevenfold increase in any disease calls for further analyses of the magnitude of the problem in order to explain and possibly prevent it. With this study, it is our hope that we have aided this process.
Conclusion
The incidence of degenerative shoulder lesions increased dramatically in the years 1996–2013 primarily due to an increase among people of working age (31–70 years) for both men and women. Incidences were higher in rural areas compared to urban. As shoulder lesions impose a huge socioeconomic burden on society, the present findings call for further investigations in aetiology, consequences and preventive measures.
References
Chiang Colvin A, Egorova N, Harrison AK, Moskowitz A, Flatow EL (2012) National trends in rotator cuff repair. J Bone Jt Surg 94:227–233
Danish Diabetes Association. The National Diabetes Register. http://www.diabetes.dk/. Accessed 22 June 2017
Gerdesmeyer L, Wagenpfeil S, Haake M, Maier M, Loew M, Gassel S (2003) Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff. A randomized controlled trial. J Am Med Assoc 290:2573–2580
Grossschaedl F, Freidl W, Éva R (2014) A 35-year trend analysis for back pain in Austria: the role of obesity. PLoS ONE 9:1–7
Hand C, Clipsham K, Rees JL, Carr AJ, Kingdom U (2008) Long-term outcome of frozen shoulder. J Shoulder Elbow Surg 17:231–236
Hsiao MS, Cameron KL, Tucker CJ, Benigni M, Blaine TA, Owens BD (2015) Shoulder impingement in the United States military. J Shoulder Elbow Surg 24:1486–1492
Hsu JE, Anakwenze OA, Warrender WJ, Abboud JA (2011) Current review of adhesive capsulitis. J Shoulder Elbow Surg 20:502–514
Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ (2014) Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Jt J 96:70–74
Kjøller M, Juel K, F K-J (2007) Folkesundhedsrapporten Danmark
Longo UG, Loppini M, Marineo G, Khan WS, Maffulli N, Denaro V (2011) Tendinopathy of the tendon of the long head of the biceps. Sport Med Arthrosc Rev 19:321–332
Miranda H, Punnett L, Viikari-Juntura E, Heliövaara M, Knekt P (2008) Physical work and chronic shoulder disorder. Results of a prospective population-based study. Ann Rheum Dis 67:218–223
Neer CS (1983) Impingement lesions. Clin Orthop Relat Res 173:70–77
Neviaser AS, Hannafin JA (2010) Adhesive capsulitis: a review of current treatment. Am J Sports Med 38:2346–2356
Nickelsen Nahne T (2002) Datavaliditet og dækningsgrad i Landspatientregisteret. Ugeskr Laeger 164:33–37
Ostör AJK, Richards CA, Prevost AT, Speed CA, Hazleman BL (2005) Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatol (Oxford) 44:800–805
Pascarelli EF, Hsu Y (2001) Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil 11:1–21
Rangan A, Goodchild L, Gibson J, Brownson P, Thomas M, Rees J, Kulkarni R (2015) BESS/BOA patient care pathways frozen shoulder. Shoulder Elbow 7:299–307
Robinson CM, Seah KTM, Chee YH, Hindle P, Murray IR, Chee YH (2012) Frozen shoulder. J Bone Jt Surg Br 9494:1–9
Russell S, Jariwala A, Conlon R, Selfe J, Richards J, Walton M (2014) A blinded, randomized, controlled trial assessing conservative management strategies for frozen shoulder. J Shoulder Elbow Surg Elsevier Ltd 23:500–507
Schmidt M, Schmidt S, Sandegaard J, Eherenstein V, Pedersen L, Sørensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 4:449–490 (In Press)
Seida JC, Leblanc C, Schouten JR, Mousavi SS, Hartling L, Vandermeer B, Tjosvold L, Sheps DM (2010) Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med 153:246–255
Seitz AL, Mcclure PW, Finucane S, Douglas N, Iii B, Michener LA (2011) Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? ☆. JCLB 26:1–12
Shanahan EM (2016) Shoulder pain at the workplace. Best Pract Res Clin Rheumatol Elsevier Ltd 25:59–68
Smith R (2001) The cost of shoulder pain at work. Br Med J 322:64–65
Stäbler MMA, Lienemann CSA (2001) On the impact of calcified deposits within the rotator cuff tendons in shoulders of patients with shoulder pain and dysfunction. Arch Orthop Trauma Surg 121:371–378
Statistics Denmark Statbank Denmark
Sundhedsstyrelsen (2013) NKR for diagnostik og behandling af patienter med udvalgte skulderlidelser
Sundhedsstyrelsen S og B (2011) Impingementsyndrom/rotator cuff-syndrom og traumatisk rotator cuff-ruptur Del 2: Faglige visitationsretningslinjer
van der Windt DA, Koes BW, de Jong BA, Bouter LM (1995) Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis Rheum Dis 54:959–964
Author information
Authors and Affiliations
Contributions
All authors have participated in conception and design of the study as well as revising the manuscript critically. NM is responsible for acquisition and interpretation of data and drafting the manuscript. TK is responsible for all data handling and statistical analyses. KWB was involved in and overall responsible for all phases of the study. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest in relation to the present study.
Funding
This study did not recieve any fundings.
Ethical approval
The study was approved by the Danish Data Protection Agency. According to Danish legislation, no IRB approval was needed, as the study is a retrospective registry study.
Informed Consent
No written consent is necessary for national databases in Denmark.
Rights and permissions
About this article
Cite this article
Monrad, N., Ganestam, A., Kallemose, T. et al. Alarming increase in the registration of degenerative rotator cuff-related lesions a nationwide epidemiological study investigating 244,519 patients. Knee Surg Sports Traumatol Arthrosc 26, 188–194 (2018). https://doi.org/10.1007/s00167-017-4626-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4626-3