Abstract
Purpose
The purpose of this study was to evaluate the effects on knee biomechanics of rotating the distal end of the bone-patellar tendon graft 90° in anatomic single-bundle (SB) anterior cruciate ligament (ACL) reconstruction with a porcine model.
Methods
Twenty (n = 20) porcine knees were evaluated using a robotic testing system. Two groups and three knee states were compared: (1) intact ACL, (2) deficient ACL and (3) anatomic SB ACL reconstruction with (a) non-rotated graft or (b) rotated graft (anatomic external fibre rotation). Anterior tibial translation (ATT), internal (IR) and external rotation (ER) and the in situ tissue force were measured under an 89-N anterior tibial (AT) load and 4-N m internal and external tibial torques.
Results
A significant difference from the intact ACL was found in ATT at 60° and 90° of knee flexion for rotated and non-rotated graft reconstructions (p < 0.05). There was a significant difference in the in situ force from the intact ACL with AT loading for rotated and non-rotated graft reconstructions at 60° and 90° of knee flexion (p < 0.05). Under IR loading, the in situ force was significantly different from the intact ACL at 30° and 60° of knee flexion for rotated and non-rotated graft reconstructions (p < 0.05). There were no significant differences in ATT, IR, ER and the in situ force between rotated and non-rotated reconstructions.
Conclusion
Graft rotation can be used with anatomic SB ACL reconstruction and not have a deleterious effect on knee anterior and rotational biomechanics. This study has clinical relevance in regard to the use of graft rotation to better reproduce the native ACL fibre orientation in ACL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroscopic anterior cruciate ligament (ACL) surgery is one of the most commonly performed surgical procedures in orthopaedic surgery [33]. Sub-optimal outcomes in long-term follow-up studies [21, 30] have been responsible for a re-evaluation of the surgical technique leading to technical modifications in arthroscopic ACL surgery. Recommendations related to modifications of ACL reconstruction vary; however, among them graft rotation in the joint space is frequently recommended and performed by many orthopaedic surgeons prior to graft tibial fixation [2, 5, 12]. Studies have suggested that the benefits of graft rotation in ACL reconstruction are reduced tibio-femoral separation, reproduction of the natural collagen fibre orientation of the ACL, increased graft strength and improved graft isometry [2–5, 8, 12, 19, 28, 29].
In the literature, the direction of ACL graft rotation has been discussed and some authors have recommended rotating the graft 90° medially (internally) [3, 5, 6], while others have advocated rotating laterally (externally) before fixation [28]. However, to mimic the native ACL fibre orientation requires 90° of lateral twisting of the graft before tibial fixation [2, 7, 8, 28, 33].
A clinical study found no difference in short-term knee laxity between patients with a non-twisted graft and a 90° externally twisted graft [8]. Hame et al., using a bone-patellar bone allograft, found that graft rotation, in either direction after fixation, leads to less knee laxity and an increase in graft tension, while graft rotation prior to fixation had no effect between neutral rotation, 90° of external and 90° internal rotation at any knee flexion [12]. According to a study by Thambyah et al., who compared untwisted and 90° twisted patellar tendon grafts, twisting significantly increased the stiffness and maximum load under axial loading [32]. In contrast, another biomechanical study found that soft tissue grafts with parallel strands were significantly stronger and stiffer than those with strands twisted 180° of a 30-mm length [19].
Cooper et al. [7] tested 37 bone-patellar tendon-bone grafts and found that twisting the graft 90° increased the strength approximately 30%, but further twisting to 180° did not increase the strength. A cadaver study found that a 90° lateral rotation of a patellar tendon graft leads to a tibial rotation similar to the intact ACL. Arnold et al. [2] found in patients that a 180° degree internal and external rotation had an unpredictable effect on the maximal force of ACL graft. A recent study that examined the use of large graft rotations, up to 900°, to shorten grafts, found that with a porcine patella tendon rotation reduced the modulus of elasticity, but did not affect strength [24]. In summary, many of the prior studies that have examined graft twisting in regard to altering mechanical strength of the graft and those that considered the effect on knee kinematics have found inconclusive or differing results.
Although there have been some studies of graft twist on knee kinematics, none have been done with the anatomic single-bundle ACL reconstruction. Thus, the effect of graft rotation with anatomic ACL reconstruction on knee biomechanics has not been studied. The purpose of this study was to evaluate the knee biomechanical effects of rotating the distal end of the bone-patellar tendon graft 90° in anatomic SB ACL reconstruction with a porcine model. The hypothesis of this study is that rotating the distal end of the bone-patellar tendon graft 90° in anatomic SB ACL reconstruction will not affect knee biomechanics. Rotating the graft 90° would better reproduce clinically the native ACL fibre orientation.
Materials and methods
Two groups of ten (n = 10) fresh frozen porcine hind limbs were obtained for this study, and institutional approval was not required. The specimens were kept frozen at −20 °C and thawed at room temperature prior to testing. The integrity of all internal knee structures was verified arthroscopically in each specimen before testing. The tibia and femur were sectioned mid-shaft, with tissues being preserved for approximately 10 cm proximally and distally from the joint with all capsular structures and ligaments kept intact. The femur and tibia bones were then embedded in heavyweight epoxy putty and secured in custom cylindrical grips.
Testing of the knees was done using a robotic system (CASPAR Staubli, Orto MAQUET) that can repeat positions within ±0.02 mm at each joint and a load cell (UFS; Model 4015; JR3 Inc.) that has a force and moment accuracy of ±0.2 N and ±0.1 N m, respectively. A MATLAB (Math Works Inc.) program controlled displacements and the forces/moments in all six degrees of freedom (DOF) while performing data acquisition. A MATLAB (Math Works Inc.) program controlled displacements well as the forces/moments in all six degrees of freedom (DOF) while simultaneously performing data acquisition. For testing, the tibial custom clamp was connected to the robot and the femoral custom clamp was secured to a fixed platform [11]. The passive flexion–extension path from 30° (porcine knee full extension) to 90° of knee flexion by minimizing the external forces and moments applied to the joint at 0.5° increments of flexion [27]. An algorithm that minimized the internal forces and moments in the knee joint determined the passive path of flexion–extension of the joint [17].
The anatomic SB ACL reconstructions were performed on all the knee specimens with a non-rotated graft in one group of specimens (n = 10) and the other group with rotated grafts (n = 10). Each group was tested with the following knee states: intact ACL, deficient ACL and either anatomic SB ACL reconstruction with a rotated graft or non-rotated graft. Three different external loads were applied to the knees during testing: (a) an 89-N anterior tibial (AT) load (simulated KT1000 test) [9, 34] to test anterior tibial translation (ATT) (mm), (b) a 4-N m internal tibial torque to test internal rotation (IR) (degrees) and (c) a 4-N m external tibial torque to test external rotation (ER) (degrees). ATT was measured at 30° (full extension), 60° and 90° of knee flexion [25] and IR and ER at 30° and 60° knee flexion [15, 16, 22].
Repeated testing after the removal of the ACL allowed in situ forces of the ACL to be determined using the principle of superposition [20, 26]. The change in force between the intact and deficient ACL knee and between the deficient and reconstructed knee, at the same joint positions and loading conditions, represents the ACL and the graft in situ force, respectively [27].
The reconstructions were performed using a three-portal technique with a 30° arthroscope [10]. Limited fat pad debridement was performed to obtain better visualization. The ACL was first cut using a number 11 surgical blade, then a punch, a shaver and an ablator (Vulcan EAS Electro-Thermal Arthroscopy System, Smith and Nephew, Endoscopy, Andover, Mass). The centre of the ACL insertion sites on the femur and tibia was marked with an awl and an ablator.
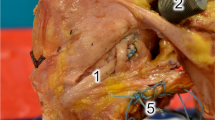
Anatomic SB ACL reconstruction was performed with the femoral and tibial tunnels placed within the marked ACL insertion sites on the femur and tibia, respectively [33]. Previously harvested porcine patellar tendon grafts, 8 mm in width and 15 mm in length, with single-side bone blocks were used for the reconstructions. The free ends of the folded grafts were whip-stitched using ultra-braided sutures with a tapered needle, and an extra-cortical button was added to the patellar bone block. One half of the graft width was coloured with a surgical pen to assess graft rotation during reconstruction (Fig. 1). For tunnel placement, a 2.4-mm guide wire was inserted into the centre of femoral ACL footprint. The femoral tunnel was drilled with a 7-mm cannulated femoral drill and then dilated with a 7.5-mm dilator through the accessory medial portal using the anteromedial portal to visualize of the femoral footprint (Fig. 2). A guide wire was inserted into the centre of tibial ACL footprint from the anteromedial aspect of tibia using a tibial drill guide system (Smith and Nephew Endoscopy, Andover, MA). The tibial ACL aimer angle was set to 55°, while the tibial tunnel was drilled with a 7-mm drill and then dilated with a 7.5-mm dilator after which point the graft was passed through the tibial tunnel [1, 14, 17, 23].
The bone block of the graft was compacted into the femoral tunnel with a compacter [1, 14, 23] (Fig. 3). In the non-rotated graft group, the tibial side of the graft was placed with the coloured side lying anteriorly, while in the rotated graft group the graft’s distal end was rotated externally (anatomic external fibre rotation) [8, 28] leaving the coloured side lying posteriorly with knee in 90° of knee flexion during arthroscopy (Fig. 4). Following graft placement, 20 flexion–extension movements were applied to the knees for pre-tensioning. The graft was tensioned at 60° of knee flexion (30° is full porcine extension) with a 40-N force applied by a ligament tension meter (Meira Corp., Nagoya, Aichi, Japan) [31]. The graft was fixed with an extra-cortical button on the femur and a screw/spiked washer on the tibia. A metallic interference screw was placed in parallel to the joint line to prevent graft rotation inside the tibial tunnel. For this study, IACUC/IRB approval was not required at the University of Pittsburgh, and all the porcine knees were acquired by a local butcher.
Statistical analysis
Differences in ATT displacement, internal and external rotation angles and in situ forces at the different knee flexion angles were analysed using one-factor analysis of variance (ANOVA) with knee state as the factor, followed by Tukey’s method for post hoc comparison. Statistical significance was set at p < 0.05, and all statistical analyses were performed using Minitab version 16 (Minitab; Minitab Inc.). To estimate the number of samples, an a priori power analysis was performed (G*power 3.1.9.2) using a significance level of 0.05, a power of 0.80 and being able to detect a difference in ATT of 2.5 mm based on previous data [17], which resulted in n = 8.
Results
Both reconstructed groups restored ATT compared to that of the intact ACL at 30° of knee flexion, but neither restored ATT at 60° and 90° of knee flexion (p < 0.05) (Fig. 5). The in situ forces were higher between both reconstruction groups and the intact ACL during AT loading at 60° and 90° knee flexion (p < 0.05) (Fig. 6). In response to internal and external tibial torques, there were no significant differences found in rotation between both reconstruction groups and the intact ACL in both IR and ER (p < 0.05) (Fig. 7). The in situ force under IR loading for both reconstructed groups was higher than that of the intact ACL at 30° of knee flexion and was higher for the non-rotated graft compared to the intact ACL at 60° of knee flexion (p < 0.05) (Fig. 8). Under ER loading, there was no significant difference in the in situ force carried in both reconstructed groups and the intact ACL (p < 0.05) (Fig. 8). Finally, no significant differences were found between the rotated and non-rotated reconstructions for ATT (p < 0.05) (Fig. 5), IR and ER (p < 0.05) (Fig. 7), and in the in situ forces for AT loading (p < 0.05) (Fig. 6) or IR–ER loading (p < 0.05) (Fig. 8).
Discussion
The most important finding of the present study was that graft rotation had minimal effect on knee kinematics. Rotating the distal end of an ACL graft in the tibial tunnel has been recommended and performed in some studies to obtain the fibre orientation of the native ACL in single-bundle ACL reconstruction [3, 8, 28]. It has been suggested that twisting the graft may also offer benefits of improving load sharing, the graft’s mechanical properties and prevention of graft-tunnel mismatch [12]. Unlike previous studies that found a difference between rotated and non-rotated ACL reconstruction graft rotation [7, 19], with anatomic reconstruction graft rotation had minimal effect on anterior stability and rotational stability in the porcine knee. In this study, there were no significant differences found between the rotated and non-rotated grafts for anterior tibial translation (ATT), internal–external rotation (IR–ER), and in the in situ forces for AT or IR–ER loading in the porcine knee. The only difference between the two reconstructions was that the non-rotated graft did not restore ER of the intact knee at 60° of knee flexion.
According to hypothesis of this study that graft rotation may not affect knee biomechanics in the ACL reconstructed knee, in terms of anterior laxity, there was no significant difference in ATT, and the in situ force at all knee flexion angles between the rotated and non-rotated graft. This is not in accordance with a cadaver study performed by Hame et al. [12] who compared the anterior–posterior laxity of the knee and graft forces before and after rotating the graft with bone-patellar tendon-bone allograft. They found that rotating an ACL allograft decreases anterior–posterior (AP) laxity of the knee and increases graft force at full extension regardless of the direction of the rotation. The graft was rotated and locked at the tip of the load cell after it had been pre-tensioned. With this protocol, twisting the graft acted to shorten it and therefore AP laxity may be decreased. When the graft was rotated prior to fixation, laxity was unchanged. In our study, the graft was rotated and tensioned before fixation which would similar to clinical practice.
The direction of graft rotation has been discussed in the literature. Some authors have recommended rotating the graft 90° medially (internally) [3, 5, 6] and others have advocated rotating laterally (externally) before fixation [28]. To mimic the native ACL fibre orientation requires 90° of lateral twisting of the graft [7, 28]. There is concordance with a study by Samuelson et al. [28], where no changes in graft force or knee laxity were found and that cautioned against external rotation of the graft. The change in graft force was not significantly different from the neutral position of the graft; additionally, unlike our study, they found that knee laxity decreased only minimally at 30° of knee flexion. Although there are several studies which graft rotation was used in ACL reconstruction, none employed anatomic ACL reconstruction [3, 8, 12, 28]. In Samuelson et al. [28] and Hame et al. [12], the method was not specified as being anatomic, and Arnold et al. [2] used transtibial ACL reconstruction.
Rotating a graft has also been shown to change some of its intrinsic mechanical properties under axial loading; however, the effects are unclear and may be tissue dependent. Cooper et al. [7] found that twisting bone-patellar tendon-bone graft 90° increased the ultimate tensile load approximately 30%, but further twisting of the graft to 180° had no significant effect compared with twisting to 90°. On the other hand, according to a study by Kim et al. [19] twisting or braiding hamstring tendons decreased the failure load and graft stiffness. A recent study using porcine patella tendon grafts that studied graft rotations up to 900° found that rotation did not change graft strength but did have an effect on elastic modulus [24].
Diduch et al. [8] in a clinical study which used anatomic ACL reconstruction found no short-term side-to-side laxity differences between a group of 60 patients who had a 90° external twist of the graft before fixation and a control group of 60 patients with no graft twist.
Thus, given that external twisting of the graft better duplicates the fibre orientation of the native ACL, it may potentially improve biological healing and remodelling.
There are some limitations to this study. Compared to the human knee, the porcine knee has a greater range of internal and external rotation and cannot fully extend (30° is full knee extension in porcine). However, several studies have used the porcine knee due to its similarity to the human knee morphology [13, 17, 18] and it serves a model for biomechanical testing. Also, the knees were evaluated at time zero which does not take into account the influence of the post-operative healing. This study has clinical relevance in regard to the use of graft rotation in ACL reconstruction because it shows that rotating the bone-patellar tendon graft in anatomic SB ACL reconstruction in order better reproduce the native ACL fibre orientation will not have a deleterious affect knee biomechanics.
Conclusion
Unlike previous studies that found a difference between rotated and non-rotated ACL reconstructions, 90° of graft rotation with anatomic reconstruction had minimal effect on anterior stability and rotational stability and the graft in situ force. Thus, graft rotation did not have a deleterious effect on knee biomechanics and may be used in ACL reconstruction.
References
Al-Husseiny M, Batterjee K (2004) Press-fit fixation in reconstruction of anterior cruciate ligament, using bone-patellar tendon-bone graft. Knee Surg Sports Traumatol Arthrosc 12(2):104–109
Arnold MP, Blankevoort L, ten Ham A, Verdonschot N, van Kampen A (2004) Twist and its effect on ACL graft forces. J Orthop Res 22(5):963–969
Beck C, Paulos LE, Rosenberg TD (1992) Anterior cruciate ligament reconstruction with the endoscopic technique. Oper Tech Orthop 2(2):86–98
Björnsson H, Desai N, Musahl V, Alentorn-Geli E, Bhandari M, Fu F, Samuelsson K (2015) Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc 23(3):696–739
Blum MF, Garth WP Jr, Lemons JE (1995) The effects of graft rotation on attachment site separation distances in anterior cruciate ligament reconstruction. Am J Sports Med 23(3):282–287
Buss DD, Warren RF, Wickiewicz TL, Galinat BJ, Panariello R (1993) Arthroscopically assisted reconstruction of the anterior cruciate ligament with use of autogenous patellar-ligament grafts. Results after twenty-four to forty-two months. J Bone Joint Surg Am 75(9):1346–1355
Cooper DE, Deng XH, Burstein AL, Warren RF (1993) The strength of the central third patellar tendon graft. A biomechanical study. Am J Sports Med 21(6):818–823 (discussion 823-814)
Diduch DR, Mann J, Geary SP, Scott WN, Huie G (1998) The effect of pretwisting the ACL autograft on knee laxity. Am J Knee Surg 11(1):15–19
Ejerhed L, Kartus J, Sernert N, Kohler K, Karlsson J (2003) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med 31(1):19–25
Fu FH, Shen W, Starman JS, Okeke N, Irrgang JJ (2008) Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am J Sports Med 36(7):1263–1274
Fujie HLG, Woo SL, Kashiwaguchi S, Blomstrom G (1995) The use of a universal force-moment sensor to determine in situ forces in ligaments: a new methodology. J Biomech Eng 117(1):1–7
Hame SL, Markolf KL, Gabayan AJ, Hunter DM, Davis B, Shapiro MS (2002) The effect of anterior cruciate ligament graft rotation on knee laxity and graft tension: an in vitro biomechanical analysis. Arthroscopy 18(1):55–60
Herbort M, Heletta S, Raschke MJ, Schliemann B, Osada N, Petersen W, Zantop T (2012) Accidental perforation of the lateral femoral cortex in ACL reconstruction: an investigation of mechanical properties of different fixation techniques. Arthroscopy 28(3):382–389
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13(4):248–255
Kanamori A, Woo SL, Ma CB, Zeminski J, Rudy TW, Li G, Livesay GA (2000) The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: a human cadaveric study using robotic technology. Arthroscopy 16(6):633–639
Kanamori A, Zeminski J, Rudy TW, Li G, Fu FH, Woo SL (2002) The effect of axial tibial torque on the function of the anterior cruciate ligament: a biomechanical study of a simulated pivot shift test. Arthroscopy 18(4):394–398
Kato Y, Ingham SJ, Kramer S, Smolinski P, Saito A, Fu FH (2010) Effect of tunnel position for anatomic single-bundle ACL reconstruction on knee biomechanics in a porcine model. Knee Surg Sports Traumatol Arthrosc 18(1):2–10
Kato Y, Ingham SJ, Linde-Rosen M, Smolinski P, Horaguchi T, Fu FH (2010) Biomechanics of the porcine triple bundle anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 18(1):20–25
Kim DH, Wilson DR, Hecker AT, Jung TM, Brown CH Jr (2003) Twisting and braiding reduces the tensile strength and stiffness of human hamstring tendon grafts used for anterior cruciate ligament reconstruction. Am J Sports Med 31(6):861–867
Livesay GA, Fujie H, Kashiwaguchi S, Morrow DA, Fu FH, Woo SL (1995) Determination of the in situ forces and force distribution within the human anterior cruciate ligament. Ann Biomed Eng 23(4):467–474
Lohmander LS, Ostenberg A, Englund M, Roos H (2004) High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 50(10):3145–3152
Miura K, Woo SL, Brinkley R, Fu YC, Noorani S (2006) Effects of knee flexion angles for graft fixation on force distribution in double-bundle anterior cruciate ligament grafts. Am J Sports Med 34(4):577–585
Musahl V, Abramowitch SD, Gabriel MT, Debski RE, Hertel P, Fu FH, Woo SL (2003) Tensile properties of an anterior cruciate ligament graft after bone-patellar tendon-bone press-fit fixation. Knee Surg Sports Traumatol Arthrosc 11(2):68–74
Oliveira DR, Garcia ET, Fuso FA, Pereira CA, Lages MM, Almeida AM, Fernandes TL, Pedrinelli A, Hernandez AJ (2016) The biomechanical effects of graft rotation on ACL reconstruction tunnel mismatch. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4070-9
Oster DM, Grood ES, Feder SM, Butler DL, Levy MS (1992) Primary and coupled motions in the intact and the ACL-deficient knee: an in vitro study in the goat model. J Orthop Res 10(4):476–484
Rudy TW, Livesay GA, Woo SL, Fu FH (1996) A combined robotic/universal force sensor approach to determine in situ forces of knee ligaments. J Biomech 29(10):1357–1360
Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH (1997) In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res 15(2):285–293
Samuelson TS, Drez D Jr, Maletis GB (1996) Anterior cruciate ligament graft rotation. Reproduction of normal graft rotation. Am J Sports Med 24(1):67–71
Shi D, Zhou J, Yapici C, Linde-Rosen M, Smolinski P, Fu FH (2015) Effect of graft fixation sequence on knee joint biomechanics in double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 23(3):655–660
Snow M, Stanish WD (2010) Double-bundle ACL reconstruction: how big is the learning curve? Knee Surg Sports Traumatol Arthrosc 18(9):1195–1200
Suzuki T, Shino K, Otsubo H, Suzuki D, Mae T, Fujimiya M, Yamashita T, Fujie H (2014) Biomechanical comparison between the rectangular-tunnel and the round-tunnel anterior cruciate ligament reconstruction procedures with a bone-patellar tendon-bone graft. Arthroscopy 30(10):1294–1302
Thambyah A, Thiagarajan P, Goh JC (2000) Biomechanical study on the effect of twisted human patellar tendon. Clin Biomech 15(10):756–760
van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J, Fu FH (2010) “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 26(9 Suppl):S2–S12
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36(1):65–72
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Funding
This study was funded by Department of Orthopaedic Surgery at the University of Pittsburgh.
Ethical approval
No ethical approval was required from IACUC.
Informed consent
Informed consent was not applicable to this study.
Rights and permissions
About this article
Cite this article
Surer, L., Michail, K., Koken, M. et al. The effect of anterior cruciate ligament graft rotation on knee biomechanics. Knee Surg Sports Traumatol Arthrosc 25, 1093–1100 (2017). https://doi.org/10.1007/s00167-016-4381-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4381-x