Abstract
Purpose
The purpose of this study was to analyse the factors affecting the conversion from posterior cruciate ligament (PCL)-retaining (CR) to PCL-substituting (PS) prostheses during total knee arthroplasty (TKA).
Methods
A total of 920 TKAs, which had been preoperatively planned to undergo implantation of CR-type prostheses, were reviewed retrospectively. Of these, 83 knees (9.0 %) were converted intraoperatively to PS prostheses. The clinical and radiological factors of the non-converted (CR) and converted (PS) groups were compared. Clinically, age, gender, body mass index, angle of flexion contracture, size of the femoral component, and thickness of the polyethylene insert were compared between the CR and PS groups. Radiologically, the severity of the varus deformity and the posterior tibial slope angle (PSA) were compared between the CR and PS groups.
Results
No significant differences in age, gender, body mass index, range of motion, thickness of the polyethylene insert, or severity of varus deformity were identified. The average preoperative angle of flexion contracture was 5.9° ± 7.4° in the CR group and 8.1° ± 9.1° in the PS group (p = 0.002). The average preoperative PSA was 9.6° ± 4.0° in the CR group and 11.0° ± 5.0° in the PS group (p = 0.018). The conversion rates to a PS-type femoral component of size C, D, and E were 13.1, 7.0, and 6.3 %, respectively (p = 0.004).
Conclusion
The conversion rate from CR- to PS-type prostheses was high in patients with severe flexion contracture, steep posterior slope, and a small femoral component size. These factors should be carefully considered for appropriate selection of prosthesis type.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Two classic options for primary total knee arthroplasty (TKA) are available, namely posterior cruciate ligament (PCL) retaining (CR) and PCL substituting (PS) [35]. The decision as to whether to retain or sacrifice the PCL remains a controversial issue in TKA [1, 5, 6, 12, 16, 27]. Some authors prefer the CR type of prosthesis, believing that it confers theoretical advantages such as proprioceptive function, joint stability, and physiological kinematics [15, 17, 21, 38, 41]. A balanced flexion/extension gap is an important goal in TKA [4, 14, 33]. A flexion gap in CR-TKA is influenced by the tension of the PCL, the amount of resected posterior femoral condyle and tibia, and the angle of the resected tibial surface slope [3, 4, 14]. When the flexion gap is tight during a CR-TKA, additional procedures such as a partial release of the PCL [4, 40], increasing the resected tibial surface slope [16], and downsizing the femoral component [14, 29] are essential. However, the PCL is resected, and conversion to PS-TKA is required, when the flexion and extension gaps continue to appear inadequate despite the above-mentioned procedures [22].
In general, CR-TKA can be difficult in severely deformed knees [28, 29, 32]. The decision to use CR-type prostheses in knees with relatively mild and moderate deformity is taken prior to surgery. However, intraoperative conversion to a PS-type prosthesis is unavoidable in several cases to achieve appropriate soft tissue balance. In a previous study, the conversion rate to PS-TKA was determined to be 17 % [20].
Most modern knee systems allow an intraoperative switch from CR type to PS type. However, there are no criteria relating to the retaining or resection of the PCL. The flexion and extension, and mediolateral gap situation, of each knee shows variation too wide to allow such a switch to be predicted prior to surgery [23]. Kaneyama et al. [23] argued that the decision of whether to preserve the PCL had to be made from the intraoperative gap measurements with an intact PCL to achieve adequate gap balancing. Ritter et al. [37] reported that the clinical difference between TKAs using CR- and PS-type prostheses may not be due solely to the difference in treatment of the PCL but also to more complex variables such as the surgeon, and also various patient factors. Therefore, it was necessary to study the affecting factors about the conversion to a PS-type prosthesis in knees that had been preoperatively planned to undergo implantation of a CR-type prosthesis. There have been a number of reports comparing the results between CR-type and PS-type prostheses [6, 9, 30]. However, to our knowledge, this is the first study to evaluate factors affecting the conversion from a CR-type to a PS-type prosthesis during CR-TKA.
The purpose of this study was to determine whether intraoperative conversion from a CR-type to a PS-type prosthesis during TKA is associated with certain underlying clinical or radiological factors.
Materials and methods
This retrospective review was approved by the Institutional Review Board of Kyung Hee University Hospital (KMC IRB 1538-08).
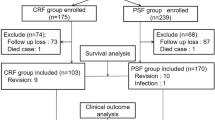
As part of this study, we reviewed 920 primary TKAs (725 patients) where the original preoperative plan had been to use a NexGen® (Zimmer, Warsaw, IN) CR-type prosthesis. Patients initially enrolled in this study underwent TKA between 1998 and 2008. Among them, 83 knees (9.0 %) underwent intraoperative conversion to a PS-type prosthesis. Patients who met the following criteria were excluded from the retrospective review: knees that used another type of prosthesis, knees with a valgus or recurvatum deformity, knees with an extra-articular deformity, haemophilic arthropathy, or partial ankylosis with a range of motion (ROM) <90°. The inclusion criteria were: moderate osteoarthritic knees (Kellgren–Lawrence grade 4) with a preoperative angle of flexion contracture <30° and varus deformity <15°. A total of 698 women and 27 men with an average age of 66 ± 7 years (range 31–90 years) were included in the study. The median body mass index (BMI) was 26.0 kg/m2 (range 18.1–37.6 kg/m2).
Surgical technique
All TKAs were performed using a midline skin incision and medial parapatellar arthrotomy. Bone cuts were made using a measured resection technique. Rotation of the femoral component was determined with reference to the transepicondylar axis, and the size was selected using the anterior-referencing method. The tibial slope was usually set to 7° of the posterior slope in the sagittal plane [11]. Any contracted medial or lateral soft tissue was evaluated carefully with palpation and then selectively released. In cases of flexion tightness or lift-off and/or disturbance of rollback during flexion, the PCL was recessed carefully or the posterior slope of the tibia was increased as necessary. PCL recession was required in 258 cases, and an increase in posterior slope of the tibia was required in 142 cases. The tibial cut surface was trimmed and adjusted using a sharp electric saw. When flexion and extension and mediolateral gaps were still mismatched despite soft tissue balancing using a CR-type prosthesis, intraoperative conversion to a PS-type prosthesis was performed. The post-operative rehabilitation was similar to the general protocol [2]. No knees were required manipulation under anaesthesia because of post-operative limitation of ROM.
Measurement methods
The clinical and radiological factors affecting the non-converted (CR) and converted (PS) groups were compared. The CR group included 837 knees, and the PS group included 83 knees.
Clinically, age, gender, BMI, angle of flexion contracture, size of the femoral component, and thickness of the polyethylene insert were compared between the CR and PS groups. The sizes of the femoral components used in our study were C, D, and E, although the particular prosthesis is available in sizes A–H. The anteroposterior lengths of the femoral components C, D, and E were 53.5, 57.5, and 61.5 mm, respectively, with an increment of 4 mm [13]. The thicknesses of the polyethylene insert used in our study were 9, 10, and 12 mm.
Radiologically, the severity of the varus deformity and the posterior tibial slope angle (PSA) were compared between the CR and PS groups (Fig. 1). Preoperative weight-bearing anteroposterior and lateral radiographs of the knee were reviewed to assess the severity of the varus deformity and the PSA using a picture archiving and communication system (PACS) [2, 3]. Consistent films in the neutral position were obtained. The normality of all radiographs was checked, and to reduce observation bias, two independent investigators repeated all radiographic measurements. The intra- and interobserver reliabilities of all measurements were assessed using intraclass correlation coefficients (ICC) [24], which were >0.8 for all measures, for both intra- and interobserver reliabilities.
a The femorotibial angle for coronal plane alignment was defined as the angle between the femoral and tibial shaft axes on true anteroposterior radiograph. b The preoperative PSA was defined as the angle between the reference line of the medullary canal and a line connecting the anterior and posterior borders of the medial tibial plateau on true lateral radiograph
Statistical analysis
The distributions of continuous variables, such as age, BMI, angle of flexion contracture, femorotibial angle, and PSA, were compared between the CR and PS groups (Student’s t test). The frequencies of the non-continuous variables, such as gender, size of the femoral component, and thickness of the polyethylene insert, were compared between the CR and PS groups (Chi-squared, χ 2 test). The continuous variables that were statistically significantly different were categorized according to subgroups, and the frequency of conversion was also compared between the two groups (χ 2 test).
Univariate analysis was performed to establish the relationships between all independent factors and the conversion to a PS-type prosthesis from a CR-type prosthesis during TKA. Factors that were determined to have a significant relationship were included in multivariate analysis.
A post hoc power analysis was conducted to estimate the minimum sample size of patients needed to observe a significant difference between groups. The present study was adequate to detect a significant difference (α < 0.05) with 80 % power. This degree of power would be achieved with study groups comprising at least 675 knees in the CR group and 61 knees in the PS group.
Results
In univariate analysis, no significant differences were identified in age, gender, BMI, range of motion, or thickness of the polyethylene insert (Table 1). The mean preoperative angle of flexion contracture was 5.9° ± 7.4° in the CR group and 8.1° ± 9.1° in the PS group (p = 0.002). Flexion contracture was classified as follows: <5°, 5°–10°, 10°–15°, 15°–20°, and >20°. The conversion rates to a PS-type prosthesis were 7.8, 7.4, 10.3, 12.5, and 14.3 %, respectively, depending on the degree of flexion contracture (p = 0.025).
No significant difference was found radiographically in the severity of preoperative varus deformity (Table 2). The average preoperative PSA varied, with values of 9.6° ± 4.0° in the CR group and 11.0° ± 5.0° in the PS group (p = 0.018). The conversion rates to a PS-type prosthesis in patients with preoperative PSA <3°, 3°–6°, 6°–9°, 9°–12°, 12°–15°, and >15°, were 7.7, 7.9, 6.7, 8.5, 10.9, and 13.6 %, respectively (p = 0.02).
The conversion rates to a PS-type femoral component of size C, D, and E were 13.1, 7.0, and 6.3 %, respectively (p = 0.004) (Table 1).
Multivariate analysis revealed three significant variables: preoperative angle of flexion contracture (p = 0.045), preoperative PSA (p = 0.032), and size of the femoral component (p = 0.011).
Discussion
The most important finding was that the conversion rate from a CR prosthesis to a PS prosthesis was high in patients with severe flexion contracture, steeper posterior tibial slope, and a smaller femoral component. There is ongoing debate regarding the most appropriate selection criteria for PCL-retaining or PCL-substituting procedure in TKA [1, 15, 16, 21, 26, 27, 42]. At present, the surgeon’s preference and the intraoperative status of the PCL and soft tissue determine whether or not a PCL should be resected [28]. Lombardi et al. [28] recommended CR-TKA only for patients without severe coronal deformity and flexion contracture. They also recommended PS-TKA for patients with inflammatory arthritis, a history of previous patellectomy or tibial osteotomy, coronal deformity >15°, moderate to severe flexion contracture, and severe contracture or dysfunction of the PCL [25, 36]. Pereira et al. [36] argued that PCL resection should be considered in knees requiring extensive soft tissue release and complex ligament balancing.
Although the selection criteria for a CR-type prosthesis differ depending on the author, a CR-type prosthesis is preferred in knees with mild varus deformity and flexion contracture. In the present study, CR-TKA was prepared preoperatively in patients with varus deformity <15° and flexion contracture <30°. The conversion rate to a PS-type prosthesis was 9.0 %. The factors that affected the conversion to PS from a CR-type prosthesis were the severity of preoperative flexion contracture, the steepness of the posterior tibial slope, and the size of the femoral component.
Flexion contracture can be resolved by removal of osteophytes located at the posterior section of the distal femur and the proximal tibia, release of the posterior capsule, additional resection of the distal femur, decreasing the slope of the tibial cut surface, and careful release of the PCL during CR-TKA [7, 28, 29]. Conversion to a PS-type prosthesis is necessary in cases with flexion tightness despite application of these techniques [7]. Berend et al. [7] performed TKA using this algorithm for conversion to a PS-type prosthesis, and 31 of 52 (59.6 %) knees were implanted with a CR-type prosthesis in patients with flexion contracture >20°. However, Mihalko et al. [34] performed TKA in 103 knees with flexion contracture >20°; the PCL was not resected in any of these knees. The PCL was partially released in only 25 knees, and the majority of the flexion contracture was resolved with careful release of the collateral ligament. In the present study, the conversion to a PS-type prosthesis was necessary in a small number of knees with flexion contracture <10°, and the conversion rate increased as the flexion contracture increased (p = 0.025). In addition, we implanted a converted PS-type prosthesis in 13 knees (14.3 %) in patients with flexion contracture of 20°–30°. These results suggest that adequate flexion and extension gaps can be acquired using a CR-type prosthesis in a large number of patients with moderate to severe flexion contracture >20°.
In the present study, the average preoperative PSA was 9.6° in the CR group and 11.0° in the PS group (Fig. 2). The recommended slope of the tibial cut surface for the NexGen® CR-type prosthesis is 7° in the sagittal plane [11]. Limited resection of the bone at the posterior aspect of the tibial plateau is anticipated in patients with excessive preoperative PSA. Flexion tightness and flexion/extension gap mismatch can also occur in these patients [3, 19]. It is important, therefore, not to excessively resect the distal femur, especially in patients with a greater PSA.
Pre- and post-operative radiographs of total knee arthroplasties (TKA) converted to a NexGen® LPS prosthesis from a NexGen® cruciate-retaining (CR) prosthesis during TKA in patients with a unilateral steep tibial slope. a A 66-year-old female had osteoarthritic knees. The range of motion was 0°–130° on both sides. The tibial posterior slope angle was 9.5° in the right knee and 16.9° in the left knee. b A CR-TKA could be performed in the right knee with a small tibial posterior slope. The conversion to a PS prosthesis from a CR prosthesis was required to achieve accurate gap balancing in the left knee with a large tibial slope angle
The conversion rates to a PS type of femur component of size C, D, and E were 13.1, 7.0, and 6.3, respectively, in the present study. The conversion rate increased with the use of smaller femoral components (p = 0.004). These results were considered to be due to the morphological characteristics of the distal femur and the aspect ratio (AP/ML ratio) in Asian populations [10, 18]. Numerous morphological studies have demonstrated that Asians have a small and narrow width of femoral condyles [10, 39]. Hitt et al. [18] reported mismatches in both size and aspect ratio and found that the prostheses do not account for the changes in aspect ratio across the femoral condylar size, and that the mediolateral sizing of the contemporary femoral components tends to be too large and thus overhang for smaller knees. The mediolateral overhang can result in irritation of the soft tissue or overstuffing of the joint space [8, 31]; it also increases the incidence of femoral component downsizing [13]. Both findings could make accurate flexion/extension balancing difficult and may have increased the incidence of conversion to a PS-type prosthesis in the present study.
This study had several limitations. First, it was a retrospective study from a consecutive series using a single prosthesis. Most of the patients were female, and all had osteoarthritic knees with varus deformities. This female predominance in the distributions of varus deformity is common in Asian populations because of differences in disease demographics among ethnic groups and gender differences in the incidence of bowed legs. Other limitations were that the femoral component size, final slope of the tibial cut surface, and the decision for conversion to the PS-type prosthesis were determined by the planning and experience of a single surgeon. Last, the clinical and radiographic results were not compared between the CR and PS groups. However, this was not necessary to evaluate the aims of the present study.
In general, the use of a CR-type prosthesis was predicted prior to surgery in patients with radiologically mild deformity. There were several knees in which the conversion to a PS-type prosthesis was required intraoperatively for balanced flexion and extension gaps, even in patients with mild deformity. Anticipating the possibility of converting the prosthesis aided the operation team in dealing appropriately with the conversion. The back table could be prepared, and operation time could be shortened.
Conclusion
The conversion rate from a CR- to a PS-type prosthesis was high in patients with severe flexion contracture, steep posterior slope, and a small femoral component size. These factors should be carefully considered for appropriate selection of prosthesis type.
References
Abdel MP, Morrey ME, Jensen MR, Morrey BF (2011) Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Joint Surg Am 93:2072–2078
Bae DK, Song SJ, Yoon KH (2010) Total knee arthroplasty following closed wedge high tibial osteotomy. Int Orthop 34:283–287
Bae DK, Song SJ, Yoon KH, Noh JH, Moon SC (2012) Comparative study of tibial posterior slop angle following cruciate-retaining total knee arthroplasty using one of three implants. Int Orthop 36:755–760
Baldini A, Scuderi GR, Aglietti P, Chalnick D, Insall JN (2004) Flexion-extension gap changes during total knee arthroplasty: effect of posterior cruciate ligament and posterior osteophytes removal. J Knee Surg 17:69–72
Becker MW, Insall JN, Faris PM (1991) Bilateral total knee arthroplasty. One cruciate retaining and one cruciate substituting. Clin Orthop Relat Res 271:122–124
Bercik MJ, Joshi A, Parvizi J (2013) Posterior cruciate-retaining versus posterior-stabilized total knee arthroplasty: a meta-analysis. J Arthroplasty 28:439–444
Berend KR, Lombardi AV Jr, Adams JB (2006) Total knee arthroplasty in patients with greater than 20 degrees flexion contracture. Clin Orthop Relat Res 452:83–87
Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E (2013) Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc 21:2314–2324
Chen JY, Lo NN, Chong HC, Pang HN, Tay DK, Chin PL, Chia SL, Yeo SJ (2014) Cruciate retaining versus posterior stabilized total knee arthroplasty after previous high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23:3607–3613
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ (2009) Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 16:341–347
Chiu YS, Chen WM, Huang CK, Chiang CC, Chen TH (2004) Fracture of the polyethylene tibial post in a NexGen posterior-stabilized knee prosthesis. J Arthroplasty 19:1045–1049
Clark CR, Rorabeck CH, MacDonald S, MacDonald D, Swafford J, Cleland D (2001) Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res 392:208–212
Dai Y, Scuderi GR, Penninger C, Bischoff JE, Rosenberg A (2014) Increased shape and size offerings of femoral components improve fit during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:2931–2940
Fitz W, Sodha S, Reichmann W, Minas T (2012) Does a modified gap-balancing technique result in medial-pivot knee kinematics in cruciate-retaining total knee arthroplasty? A pilot study. Clin Orthop Relat Res 470:91–98
Fuchs S, Tibesku CO, Genkinger M, Laass H, Rosenbaum D (2003) Proprioception with bicondylar sledge prostheses retaining cruciate ligaments. Clin Orthop Relat Res 406:148–154
Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD (2008) Midterm comparison of posterior cruciate-retaining versus -substituting total knee arthroplasty using the Genesis II prosthesis. A multicenter prospective randomized clinical trial. Knee 15:217–221
Hino K, Ishimaru M, Iseki Y, Watanabe S, Onishi Y, Miura H (2013) Mid-flexion laxity is greater after posterior-stabilised total knee replacement than with cruciate-retaining procedures: a computer navigation study. Bone Joint J 95-B:493–497
Hitt K, Shurman JR, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA (2003) Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 85-A(Suppl 4):115–122
In Y, Kim JM, Woo YK, Choi NY, Sohn JM, Koh HS (2009) Factors affecting flexion gap tightness in cruciate-retaining total knee arthroplasty. J Arthroplasty 24:317–321
In Y, Kim SJ, Kim JM, Woo YK, Choi NY, Kang JW (2009) Agreements between different methods of gap balance estimation in cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 17:60–64
Joglekar S, Gioe TJ, Yoon P, Schwartz MH (2012) Gait analysis comparison of cruciate retaining and substituting TKA following PCL sacrifice. Knee 19:279–285
Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y (2001) Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res 391:210–217
Kaneyama R, Otsuka M, Shiratsuchi H, Oinuma K, Miura Y, Tamaki T (2014) Criteria for preserving posterior cruciate ligament depending on intra-operative gap measurement in total knee replacement. Bone Joint Res 3:95–100
Lachin JM (2004) The role of measurement reliability in clinical trials. Clin Trials 1:553–566
Laskin RS (1996) The insall award. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop Relat Res 331:29–34
Li G, Zayontz S, Most E, Otterberg E, Sabbag K, Rubash HE (2001) Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty 16:150–156
Liu HG, Zhu W, Zhang ZX (2015) Comparison of outcomes after bilateral simultaneous total knee arthroplasty using posterior-substituting versus cruciate-retaining prostheses. Saudi Med J 36:190–195
Lombardi AV Jr, Berend KR (2006) Posterior cruciate ligament-retaining, posterior stabilized, and varus/valgus posterior stabilized constrained articulations in total knee arthroplasty. Instr Course Lect 55:419–427
Lombardi AV Jr, Mallory TH, Fada RA, Hartman JF, Capps SG, Kefauver CA, Adams JB (2001) An algorithm for the posterior cruciate ligament in total knee arthroplasty. Clin Orthop Relat Res 392:75–87
Lutzner J, Firmbach FP, Lutzner C, Dexel J, Kirschner S (2015) Similar stability and range of motion between cruciate-retaining and cruciate-substituting ultracongruent insert total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1638–1643
Mahoney OM, Kinsey T (2010) Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences. J Bone Joint Surg Am 92:1115–1121
Matsuzaki T, Matsumoto T, Kubo S, Muratsu H, Matsushita T, Kawakami Y, Ishida K, Oka S, Kuroda R, Kurosaka M (2014) Tibial internal rotation is affected by lateral laxity in cruciate-retaining total knee arthroplasty: an intraoperative kinematic study using a navigation system and offset-type tensor. Knee Surg Sports Traumatol Arthrosc 22:615–620
Mihalko WM, Miller C, Krackow KA (2000) Total knee arthroplasty ligament balancing and gap kinematics with posterior cruciate ligament retention and sacrifice. Am J Orthop (Belle Mead NJ) 29:610–616
Mihalko WM, Whiteside LA (2003) Bone resection and ligament treatment for flexion contracture in knee arthroplasty. Clin Orthop Relat Res 406:141–147
Nguyen LC, Lehil MS, Bozic KJ (2015) Trends in total knee arthroplasty implant utilization. J Arthroplasty 30:739–742
Pereira DS, Jaffe FF, Ortiguera C (1998) Posterior cruciate ligament-sparing versus posterior cruciate ligament-sacrificing arthroplasty. Functional results using the same prosthesis. J Arthroplasty 13:138–144
Ritter MA, Davis KE, Farris A, Keating EM, Faris PM (2014) The surgeon’s role in relative success of PCL-retaining and PCL-substituting total knee arthroplasty. HSSJ 10:107–115
Sierra RJ, Berry DJ (2008) Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty 23:20–23
Vaidya SV, Ranawat CS, Aroojis A, Laud NS (2000) Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty 15:79–85
Yamakado K, Worland RL, Jessup DE, Diaz-Borjon E, Pinilla R (2003) Tight posterior cruciate ligament in posterior cruciate-retaining total knee arthroplasty: a cause of posteromedial subluxation of the femur. J Arthroplasty 18:570–574
Zhang K, Mihalko WM (2012) Posterior cruciate mechanoreceptors in osteoarthritic and cruciate-retaining TKA retrievals: a pilot study. Clin Orthop Relat Res 470:1855–1859
Zhang Z, Zhu W, Zhang W (2015) High-flexion posterior-substituting versus cruciate-retaining prosthesis in total knee arthroplasty: functional outcome, range of motion and complication comparison. Arch Orthop Trauma Surg 135:119–124
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bae, D.K., Song, S.J., Kim, K.I. et al. Intraoperative factors affecting conversion from cruciate retaining to cruciate substituting in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24, 3247–3253 (2016). https://doi.org/10.1007/s00167-015-3971-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3971-3