Abstract
Purpose
To analyse the non-response group in the Swedish Knee Ligament Register (SKLR).
Methods
All 3588 patients in the SKLR who had undergone anterior cruciate ligament surgery in 2010 were included. Respondents (n = 1865) and non-respondents (n = 1723) at the 2-year follow-up survey were assessed for potential differences in demographics and baseline data. KOOS/EQ5D questionnaires were sent to non-respondents together with a non-response survey asking questions about reasons for dropout.
Results
Respondents had a significantly higher mean age (27.8 years, range 9–64) than non-respondents (25.9 years, range 12–65) (p < 0.001). Women had a higher rate of response 927 (62.8 %) than men 938 (44.4 %) even after correction for age (p < 0.001). Alpine/telemark skiing was the only activity at time of injury that showed higher rate of respondents 280 (62.5 %) compared to non-respondents 168 (37.5 %) (p < 0.001). No differences in EQ5D at 2-year follow-up were found between the groups. The change in KOOS from 0 to 2 years showed difference in the subscale pain with 9.4 in the response group compared to 6.3 in the late-response group (p < 0.05) and the subscale quality of life with a difference of 26.1 and 22.6, respectively (p < 0.05). The non-response questionnaire showed shortcomings in patient information regarding the importance of the SKLR.
Conclusion
The register is valid concerning baseline surgical data, but higher age, female gender and perhaps higher socioeconomic status improve the response rates. KOOS showed small differences of questionable clinical significance. The SKLR patient information could be improved.
Level of evidence
Retrospective comparative study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An injury to the anterior cruciate ligament (ACL) is a common and serious knee injury with a high risk of morbidity in the young and active population. The annual incidence in Sweden is estimated to be 78 per 100,000 inhabitants with a mean age of 32 years [13]. The treatment is rehabilitation or reconstructive surgery depending on the patient’s need and the degree of subjective knee laxity [17]. In Sweden, 36 % of the cruciate ligament-injured population undergoes surgery, with a mean age of 27 years (59 % being male) [13].
Knee ligament procedures in Sweden are registered in the Swedish Knee Ligament Register (SKLR) with coverage of more than 90 % [18]. The overall objective of the registry is to promote improved care of individuals with ACL injuries. The SKLR database utilizes a web-based interface and consists of two parts, a patient and a surgeon section. The surgeon section includes factors such as graft selection, previous surgery, activity at time of injury, time between injury and surgery, associated injuries of the meniscus, cartilage or other ligaments of the knee and method of graft fixation. The patient section consists of Knee injury and Osteoarthritis Outcome Score (KOOS) and EQ5D.
A main problem for patient registries is low compliance in follow-up registrations. In order to draw valid conclusions from registry data, it is of great importance that the data quality of key variables is validated. Historically, a response rate of 60 % has been used as a threshold for acceptability and a benchmark for measuring the validity of survey quality [8]. This is, however, not a scientifically proven minimal acceptable rate but more of an arbitrary “rule of thumb” [8]. It is also important to analyse whether the distribution of respondents is a fair representation of the whole group or whether the baseline and demographic data between respondents and non-respondents differ systematically.
The 1- and 2-year follow-up KOOS response rate in the SKLR 2012 was 60 and 52 %, respectively, and the primary aim of this study was to investigate whether respondents and non-respondents of the 2-year follow-up differed significantly with respect to the nature of ACL injury, the method of surgery and demographic variables. The second aim was to analyse whether the outcome variables KOOS and EQ5D differed between respondents and non-respondents. The third aim was to examine reasons for dropout in order to be able to improve data collection in the future.
This is the first non-response analysis of the SKLR, and we hypothesize that the information given in the register is valid with no significant differences between respondents and non-respondents.
Materials and methods
Ethical permission for use of the register has been approved by the regional ethics committee, Karolinska Institutet (D-number: 2011/337-31/3).
Study sample
Validation of key baseline data
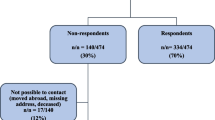
All patients in the SKLR who had undergone ACL surgery in 2010 (n = 3588) were included in the analysis. The sample was divided into the groups “respondents” (R) and “non-respondents” (NR) based on whether the patient had responded or not to the standard 2-year follow-up. The following patient characteristics were included: age, gender, time between injury and surgery, concomitant meniscal and/or cartilage injuries, type of graft, primary or revision surgery and activity at time of injury (ATI) (Fig. 1).
Outcome analysis (KOOS and EQ5D)
The same sample is used for outcome analysis of KOOS and EQ5D. The patients who had not answered their 2-year follow-up (NR-group) had an additional reminder sent to them by postal letter with instruction to reply on the 2-year follow-up. The patients who replied to the reminder and had registered KOOS and EQ5D preoperatively were labelled late responders (LR). Since not all patients in the R-group had preoperative data, a different response group is used: responder outcome (RO). All patients did not reply to both KOOS and EQ5D-questionnaires; thus, the number of patients in each outcome group (KOOS and EQ5D) is not consistent (Fig. 1).
The non-response survey
In order to obtain information concerning the reasons for dropout, a non-response survey was included with the reminder to the NR-group in March 2013. The survey was created after consultation with the board of the SKLR and consisted of seven pages. The first page was information about the survey. The second page consisted of two “Yes or No” questions (B1–B2) and five statements (B3–B7) where the patient reported level of agreement on a scale from 1 to 10 where 10 was full agreement. A box for optional comments was included at the end of the page. The last five pages consisted of the standard KOOS and EQ5D questions. A postage-paid self-addressed return envelope was provided. The patients who replied to the non-response survey did not always reply to the KOOS and EQ5D questions; thus, the number of patients is inconsistent compared to the outcome analysis.
Statistical analysis
Two separate databases—the inquiry of reasons for dropout and the ACL database—were analysed. All statistics were collected with SPSS, version 22.0. All variables were summarized with standard descriptive statistics such as frequencies, means, standard deviations (SD) and range. Differences in distributions of categorical variables were analysed with Pearson’s Chi-square test. If an expected frequency in any cell was 5 or less, Fisher’s exact test was applied. Provided that the distribution of a variable was not severely skewed, differences between groups were analysed with parametric tests. Difference between groups in age was analysed with a Student’s t test for independent groups. Since there were significant differences in age and gender, all group differences were analysed with analyses of covariance (Group × Gender with age as covariate). The distributions of responses in the non-response survey were severely skewed; that is, the skewness statistics was greater than 1.5; thus, the interrelationships between items were calculated as Kendall’s rank correlation coefficients. The significance level in all analyses was 5 % (two-tailed).
Results
Validation of key baseline data
A total of 3588 patients (2112/58.9 % men and 1476/41.1 % women) who had undergone ACL surgery in 2010 were identified in the SKLR, 1865 were R and 1723 were NR at 2 years. The mean age was significantly higher for R (27.8 years, range 9–64) than NR (25.9 years, range 12–65) (p < 0.001). Women had a significantly higher rate of response (62.8 %) than men (44.4 %) (p < 0.001) (Table 1). Thus, the remaining baseline and outcome data were statistically corrected for age and gender.
There was no significant difference between R and NR in the distribution of concomitant meniscal or cartilage injuries, number of days between injury and surgery, type of graft or primary versus revision surgery. The responder frequencies of activity at time of injury varied between 48.7 and 51.7 % except for “Alpine and telemark skiing” which had a significantly higher response rate of 62.5 % (p < 0.001) (Table 2).
KOOS analysis
The change in KOOS between preoperatively and 2-year follow-up was analysed in the RO-group (n = 1358) and the LR-group (n = 291) (Fig. 1). Only patients who had registered KOOS both preoperatively and 2-years postoperatively were included. Each subscale is presented for the RO-group and the LR-group in Table 3.
Two subscales showed significant differences: “pain” with an improvement in KOOS of 9.4 in the RO-group compared to 6.3 in the LR-group (p = 0.043), “quality of life” with an improvement in KOOS of 26.1 in the RO-group compared to 22.6 in the LR-group (p = 0.039). All other subscales showed no statistical significant differences. The results are shown in Fig. 2.
EQ5D analysis
As with the KOOS analysis, the change in EQ5D preoperatively was compared to EQ5D 2 years postoperatively in the RO-group (n = 1233) and the LR-group (n = 261). Only patients who had registered EQ5D both preoperatively and 2-years postoperatively were included (Table 4). The results showed no statistical significant differences (Fig. 3).
Non-response survey
In total, 359, 214 men and 145 women, of 1723 (20.8 %) patients answered the non-response questionnaire. Sixty per cent of the patients considered that they had been given information about the SKLR at the time of surgery and 81 % had been asked to answer the 2-year follow-up questionnaire (Fig. 4). There was one minor but significant difference between genders, the women with a mean score of 2.57 found the EQ5D and KOOS questions harder to understand than men with a mean score of men 2.13 (p = 0.038), but most patient disagreed to the statement B5. Of 55 comments in the non-response survey, 29 were variants on; “I forgot/I did not have the time/I am lazy” and 15 dealt with log in difficulties to the website “www.aclregister.nu”.
The statements B3–B7 had a low percentage of agreement (Fig. 4). In Table 5, the relationships between the items of the non-response inventory are shown. The magnitude of the coefficients ranged between 0.00 and 0.37. Although some of the coefficients were statistically significant, the relationships were generally weak (86 % or 18 out of 21 were ≤0.30, i.e. 9 % common variance), indicating that the items seem to reflect different aspects of reasons for non-responding.
Discussion
This is the first non-response survey of the SKLR. Since the response rates declines to a level below what is generally accepted, a thorough analysis of the non-response group is of great importance in order to use registry data in research [8]. The response rate per se is not the only important factor for evaluating register data, but of equal importance is how respondents differ from non-respondents regarding demographic and baseline data, a non-response bias [8].
Women and older patients in our material had a significantly higher rate of response, which is consistent with findings in other studies [3, 5, 20]. This could be of concern since older patients in the SKLR have better improvement in KOOS after surgery, which is seen gradually from the age of 30 and is significant in the age group >40 years [4]. The older group of patients might be less prone to undergo surgery which could indicate that there is a better selection of patients in need of surgery and this could explain why their outcome is better. Women on the other hand tend to have lower postoperative KOOS compared to men after ACL surgery [1]. Thus, all our analyses were statistically corrected for age and gender. The mean age difference of less than 2 years between the groups, respondents 27.8 and non-respondents 25.9, is important to notice but considered too small to be clinically relevant.
Soccer is the primary aetiology of ACL injuries in the SKLR, Norwegian Knee Ligament Register (NKLR) and the Danish Knee Ligament Register (DKLR) [7]. In the SKLR, “Alpine and telemark skiing” and “floorball” is the second and third most common activity at time of injury [18]. In our analysis, Alpine/Telemark skiing was the only activity at time of injury (ATI) which had a significant higher rate of respondents compared to other ATI’s. Finnish research has shown that downhill skiing among adolescents is associated with higher socioeconomic status [9, 19], and epidemiologic studies have shown a positive correlation between response rate and socioeconomic status [6]. If we assume that the group Alpine/Telemark belongs to a higher socioeconomic status, this may be one possible explanation for the different response rates between the groups.
The risk of meniscal and cartilage injuries increases with time between injury and surgery [2] and concomitant injuries may affect KOOS and could cause bias in the register if it differs between respondents and non-respondents. We found no significant difference in time between injury and surgery. Neither could we detect any differences in concomitant meniscal and/or cartilage injuries, type of graft or primary surgery and revision surgery between respondents and non-respondents.
In our KOOS analysis, two out of five subscales showed significant differences. These results differ when compared to a study of the DKLR [14]. In this study by Rahr-Wagner et al., none of the five KOOS subscales showed any significant difference between respondents and non-respondents at the 1-year follow-up. However, the two analyses differ in several ways. Our study analysed the improvement between KOOS preoperative and 2 year postoperatively instead of analysing the outcome at one-year only. The two groups were also selected differently; the Danish study selected 100 patients randomly from each group and only 62 % of the respondents and 39 % of the non-respondents completed the questionnaire. We used the existing information in the SKLR together with the new information gathered with our questionnaire. This resulted in substantially larger groups (respondents n = 1358, late respondents n = 291) compared to the study of Rahr-Wagner.
Nevertheless, our study showed statistical differences regarding improvement in the KOOS subscales pain and quality of life in the 2-year follow-up. These differences persisted when corrected for age and gender. Whether these differences are relevant can be questioned [16]. Our interpretation is that the clinical differences regarding KOOS at the 2-year follow-up between the studied groups are small, but should be taken into consideration when analysing register data. Outcome of other non-respondent surveys shows a tendency towards worse outcome in the group of non-respondents [10, 12].
Previous reports from the SKLR have shown that female patients has worse EQ5D scores preoperatively than male patients, but at 1 and 2 years postoperatively no sex differences can be found [1]. The EQ5D analysis in our study showed no significant difference, after correction for age and gender, between the respondents and late respondents.
In the non-response survey, 40 % had not been given information about the SKLR at the time of surgery. There is thus room for improvement with regard to information about the registry to patients. The statement that most patients agreed upon was that registering in the SKLR was time-consuming, but only 31 % pointed this out. The most common given reason for non-response was—“I forgot/I did not have the time/I am lazy”. This is similar to other studies of non-response [11, 15]. It seems, therefore, that the way the follow-up is designed is not the main reason for the dropout at 2-year follow-up, but it is important to have a good balance between the information you wish to collect and the size and depth of the questionnaire.
We have not been able to analyse the subjective outcome of the whole non-response group, which is a weakness. We can only assume that the late-response group is representable of the group of non-respondents regarding subjective outcome variables.
There are inconsistent group sizes in the different analysis since the analyses are made on changes over time and only patients who had replied both preoperatively and at 2-year follow-up were included.
Conclusion
The register is valid concerning baseline surgical data, but higher age, female gender and perhaps higher socioeconomic status improve the response rates. KOOS showed small differences of questionable clinical significance. The SKLR patient information could be improved.
References
Ageberg E, Forssblad M, Herbertsson P, Roos EM (2010) Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish Knee Ligament Register. Am J Sports Med 38(7):1334–1342
Barenius B, Forssblad M, Engström B, Eriksson K (2013) Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 21(4):914–927
Christensen AI, Ekholm O, Glumer C, Andreasen AH, Hvidberg MF, Kristensen PL, Larsen FB, Ortiz B, Juel K (2012) The Danish National Health Survey 2010. Study design and respondent characteristics. Scand J Public Health 40(4):391–397
Desai N, Bjornsson H, Samuelsson K, Karlsson J, Forssblad M (2014) Outcomes after ACL reconstruction with focus on older patients: results from The Swedish National Anterior Cruciate Ligament Register. Knee Surg Sports Traumatol Arthrosc 22(2):379–386
Eaker S, Bergstrom R, Bergstrom A, Adami HO, Nyren O (1998) Response rate to mailed epidemiologic questionnaires: a population-based randomized trial of variations in design and mailing routines. Am J Epidemiol 147(1):74–82
Ekholm O, Gundgaard J, Rasmussen NK, Hansen EH (2010) The effect of health, socio-economic position, and mode of data collection on non-response in health interview surveys. Scand J Public Health 38(7):699–706
Granan L-P, Forssblad M, Lind M, Engebretsen L (2009) The Scandinavian ACL registries 2004–2007: baseline epidemiology. Acta Orthop 80(5):563–567
Johnson TP, Wislar JS (2012) Response rates and nonresponse errors in surveys. JAMA 307(17):1805–1806
Kantomaa MT, Tammelin TH, Nayha S, Taanila AM (2007) Adolescents’ physical activity in relation to family income and parents’ education. Prev Med 44(5):410–415
Kim J, Lonner JH, Nelson CL, Lotke PA (2004) Response bias: effect on outcomes evaluation by mail surveys after total knee arthroplasty. J Bone Joint Surg Am 86-A(1):15–21
Kotaniemi JT, Hassi J, Kataja M, Jonsson E, Laitinen LA, Sovijarvi AR, Lundback B (2001) Does non-responder bias have a significant effect on the results in a postal questionnaire study? Eur J Epidemiol 17(9):809–817
Murray DW, Britton AR, Bulstrode CJ (1997) Loss to follow-up matters. J Bone Joint Surg Br 79(2):254–257
Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L (2012) A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: incidence, treatment, and sex differences. Am J Sports Med 40(8):1808–1813
Rahr-Wagner L, Thillemann TM, Lind MC, Pedersen AB (2013) Validation of 14,500 operated knees registered in the Danish Knee Ligament Reconstruction Register: registration completeness and validity of key variables. Clin Epidemiol 5:219–228
Ronmark E, Lundqvist A, Lundback B, Nystrom L (1999) Non-responders to a postal questionnaire on respiratory symptoms and diseases. Eur J Epidemiol 15(3):293–299
Roos EM, Lohmander LS (2003) The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Spindler KP, Wright RW (2008) Clinical practice. Anterior cruciate ligament tear. N Engl J Med 359(20):2135–2142
Swedish Knee Ligament Register. Swedish national ACL database homepage. Accessed 12 July 2015
Tammelin T, Nayha S, Hills AP, Jarvelin MR (2003) Adolescent participation in sports and adult physical activity. Am J Prev Med 24(1):22–28
Tolonen H, Helakorpi S, Talala K, Helasoja V, Martelin T, Prattala R (2006) 25-Year trends and socio-demographic differences in response rates: Finnish adult health behaviour survey. Eur J Epidemiol 21(6):409–415
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reinholdsson, J., Kraus-Schmitz, J., Forssblad, M. et al. A non-response analysis of 2-year data in the Swedish Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 25, 2481–2487 (2017). https://doi.org/10.1007/s00167-015-3969-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3969-x