Abstract
Purpose
Although trans-portal and outside-in techniques are commonly used for anatomical ACL reconstruction, there is very little information on variability in tunnel placement between two techniques.
Methods
A total of 103 patients who received ACL reconstruction using trans-portal (50 patients) and outside-in techniques (53 patients) were included in the study. The ACL tunnel location, length and graft–femoral tunnel angle were analyzed using the 3D CT knee models, and we compared the location and length of the femoral and tibial tunnels, and graft bending angle between the two techniques. The variability in each technique regarding the tunnel location, length and graft tunnel angle using the range values was also compared.
Results
There were no differences in the average of femoral tunnel depth and height between the two groups. The ranges of femoral tunnel depth and height showed no difference between two groups (36 and 41 % in trans-portal technique vs. 32 and 41 % in outside-in technique). The average value and ranges of tibial tunnel location also showed similar results in two groups. The outside-in technique showed longer femoral tunnel than the trans-portal technique (34.0 vs. 36.8 mm, p = 0.001). The range of femoral tunnel was also wider in trans-portal technique than in outside-in technique. Although the outside-in technique showed significant acute graft bending angle than trans-portal technique in average values, the trans-portal technique showed wider ranges in graft bending angle than outside-in technique [ranges 73° (SD 13.6) vs. 53° (SD 10.7), respectively].
Conclusions
Although both trans-portal and outside-in techniques in ACL reconstruction can provide relatively consistent in femoral and tibial tunnel locations, trans-portal technique showed high variability in femoral tunnel length and graft bending angles than outside-in technique. Therefore, the outside-in technique in ACL reconstruction is considered as the effective method for surgeons to make more consistent femoral tunnel.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The one of the most important factors for successful ACL reconstruction is the making of accurate tunnels in anatomical position. However, several studies reported the difficulty of anatomical tunnel placement by the trans-tibial technique; hence, making femoral tunnels using anteromedial portal or outside-in techniques have become popular for anatomical ACL reconstruction [5, 13, 22, 31].
Anteromedial portal or outside-in techniques can make femoral tunnels independently from tibial tunnels with more anatomical tunnels than the trans-tibial technique [10, 18, 22, 25, 26, 28, 32]. Anatomical studies using cadavers have provided a better understanding of the footprint anatomy of ACL [7–9, 14, 21]. However, the application of the knowledge of ACL anatomy to tunnel positioning under arthroscopic view remains a challenge. Although it is important to determine which techniques provide consistent and reproducible ACL reconstruction, there is very little information on variability in femoral tunnel placement between the trans-portal and outside-in techniques [30]. Moreover, some studies reported that the femoral tunnel position showed large variability in trans-portal technique in ACLR due to different knee flexion angles [1].
The purpose of this study was to compare the tibial and femoral tunnel locations, as well as tunnel lengths and graft bending angles between trans-portal and outside-in techniques in ACL reconstruction. The variability of them between the two techniques in ACL reconstruction was also determined. The hypothesis was that the outside-in technique in ACL reconstruction is a more reliable method for consistent anatomical tunnel position in ACL reconstruction by reducing the variability of tunnel locations.
Materials and methods
One hundred and three patients who received ACL reconstruction using trans-portal (50 patients) and outside-in techniques (53 patients) by four surgeons were included in the study according to the intra-operative method used for femoral tunnel drilling. The four participating surgeons in this study had previously performed more than 100 ACL reconstructions. The femoral tunnels were drilled using the portal technique through accessory anteromedial portal by two surgeons (50 cases) and outside-in technique by two surgeons (53 cases).
For ACL reconstruction, tibial tunnel preparation using a drill guide (ConMed Linvatec, Largo, FL, USA) at 45°–50° within the centre of the ACL insertion was made in both techniques. Notchplasty was not performed in any knee in either group during reconstruction. The tibialis allograft or hamstring autograft were fixed using a bio-interference screw and screw washer for tibial side in both groups with the knee in 10°–20° of flexion. The femoral tunnel was created at the centre of the footprint from the accessory anteromedial portal at about 110°–120° of knee flexion under arthroscopic visualization through anterolateral portal in trans-portal technique [10, 26]. However, in the outside-in technique, the femoral tunnel was placed using femoral guide (Arthrex, Naples, Florida) through anterolateral portal under arthroscopic visualization from accessory anteromedial portal at the centre of the footprint at about 70°–90° of knee flexion [23].
The institutional (Chonnam national university Hwasun hospital) review boards approved the study design (TPM-15-155), and the written consents were obtained from all patients to undergo computed tomography (CT) scan after ACL reconstruction using the same scanning protocol. The ACL tunnel location, length and graft–femoral tunnel angle were analyzed using the 3D knee models with tunnels.
The location and length of the femoral and tibial tunnels, and graft bending angle were compared between the two techniques. The inter-surgeon variabilities in each technique regarding the tunnel location, length and graft tunnel angle using ranges and standard deviation (SD) were also compared.
Measurement of tunnel location and length, and graft bending angle
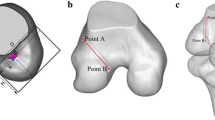
Computed tomography (CT) knee scans (GE Medical Systems, Milwaukee, WI, USA) at a 0° of knee flexion were performed between 2 and 6 weeks after the ACL reconstruction with the patients’ consent. 3D models of the distal femur, proximal tibias including bony tunnels were created using DICOM CT images by Mimics 12.0 software (Materialise, Leuven, Belgium). For the measurement of femoral tunnel, the axis of diaphysis was determined and rotated the 3D model to exactly overlapped medial and lateral femoral condyle, which was similar to direct lateral radiograph. After removing the medial femoral condyle at the top of intercondylar notch virtually, the medial–lateral (M–L) view of the lateral femoral condyle was taken at the true lateral position for the measurement of the femoral tunnel position. The top view of the proximal tibia was taken for measurement of the tibial tunnel position [25, 30].
The measurement method for the femoral tunnel location was adapted from the quadrant method described by Bernard et al. [4]. The depth of the femoral tunnel (A/D) was measured from the centre of the tunnel to the deepest subchondral bone contour (A) in the percentage of the D (lateral femoral condyle diameter along intercondylar notch roof). The height of the femoral tunnel (B/H) was evaluated and expressed from the centre of the tunnel to the intercondylar notch roof (B) as in percentages of the H (intercondylar notch roof height) (Fig. 1). The measurement of the tibial tunnel position was by the method of Lertwanich (Fig. 2) [15]. The tibial tunnel position was quantified from the anterior border (A) and the medial border (B) of this reference frame and expressed in percentages of the total anteroposterior distance (D) and mediolateral width (W) of the proximal tibia (A/D, B/W). The lengths of the femoral and tibial tunnels were also measured on 3D models (Fig. 3). The tunnel length was defined the length of line between the centre point of outer apertures of femoral or tibial tunnels and the centre points of inner aperture of femoral or tibial tunnel. The graft bending angle at the femoral tunnel was measured as the angle between axis of femoral tunnel and the graft axis (Fig. 3) [25].
All measurements for each model were performed using Mimics 12.0 software (Materialise, Leuven, Belgium). Two orthopaedic surgeons (independent observers who were blinded to surgical group during measurement) measured tunnel position. They carried out the measurement twice with an interval of 2 weeks. They were blinded to each other’s measurement, as well their own prior measurement.
Statistical analysis
Sample size was estimated based on results of the first twenty patients in this study (first ten cases in the trans-portal group and first ten cases in the outside-in group). Forty-four patients per group were needed to detect a 4.5° difference with 7.5° SD in graft bending angle between groups (power = 0.8 confidence level 0.05). This size also satisfied a power of 80 % to detect a difference of 3.3 mm with a 5.5 mm SD in the femoral tunnel length between the groups.
All statistical analyses were performed using SPSS for Windows (version 16; SPSS, Chicago, Illinois). Inter-observer reliabilities were measured using the intraclass correlation coefficient (ICC), and normal data distribution was evaluated using the Kolmogorov–Smirnov test. The independent t test was used for comparison of tunnel location, length and graft bending angles between the two groups for inter-technique variability. For inter-surgeon variability analysis, mean values, SDs and the range between surgeons in tunnel location, length and graft bending angles were calculated (absolute in mm or degree and relative in %) and compared between two surgeons in each technique (i.e. trans-portal and outside-in techniques). Scatter plots were generated for inter-technique variability in each parameter. All statistical significance was accepted for p values of <0.05. The inter-observer reliabilities for the measurement of tunnel position (0.79–0.88), tunnel length (0.85–0.91) and graft bending angles (0.71–0.85) were quite high.
Results
The depth of femoral tunnel from the posterior wall was similar between the two groups (31 ± 7 % in trans-portal and 31 ± 7 % in outside-in techniques, p = n.s). Moreover, there was no difference in height of femoral tunnel from inferior femoral condyle between the two groups (42 ± 8 % in trans-portal and 40 ± 9 % in outside-in techniques, p = n.s). In terms of inter-surgeon variability in each group, the ranges of femoral tunnel depth and height were 36 and 41 % in trans-portal technique and 32 and 41 % in outside-in technique (Table 1, Fig. 4).The mean anteroposterior position of tibial tunnel was 41 ± 8 % in trans-portal and 44 ± 6 % in outside-in techniques (p = n.s), and the mean mediolateral position of tibial tunnel was 46 ± 3 % in trans-portal and 45 ± 4 % in outside-in techniques (p = n.s). In terms of tunnel location, the ranges of tibial tunnel anteroposterior position (31 and 25 % in trans-portal and outside-in techniques) were wider than the mediolateral positions (13 % in trans-portal and 16 % in outside-in techniques) (Table 2; Fig. 5).
The outside-in technique showed greater femoral tunnel length than the trans-portal technique (36.8 ± 4.3 vs. 34.0 ± 6.6 mm, p = 0.001). The range of femoral tunnel was wider in trans-portal technique (28 mm) than in outside-in technique (18 mm). However, the tibial tunnel length showed similar results in terms of average values (38.9 ± 4.9 mm in trans-portal vs. 37.2 ± 4.7 mm in outside-in techniques) and ranges (18 and 21 mm) (Table 3).
Although the outside-in technique showed significant acute angle between graft and femoral tunnel than trans-portal technique in average values (98.7 ± 10.7° vs. 112.4 ± 13.6°, respectively), the trans-portal technique showed more variable ranges than outside-in technique (ranges 73° vs. 53°, respectively) (Table 4; Fig. 5).
Discussion
The main finding of this study was that trans-portal technique showed high variability in femoral tunnel length and graft bending angles than outside-in techniques although both trans-portal and outside-in techniques in ACL reconstruction can provide relatively consistent femoral and tibial tunnel locations. Moreover, the bending angle between graft and femoral tunnel at extension was significantly acute in outside-in technique than in trans-portal technique.
The trans-portal or outside-in techniques in ACL reconstruction are recommended over the traditional trans-tibial technique for the making of an anatomical femoral tunnel in ACL reconstruction [10, 24–26, 32]. Although both techniques provide more anatomical femoral tunnel than standard trans-tibial technique, the variability in tunnel placement of two techniques is not known. Consistent with other results [24–26, 32], we found both techniques could provide horizontal anatomical femoral tunnel positioning (42 and 40 % height in trans-portal and outside-in techniques, respectively). Moreover, both techniques showed wide ranges (about 40 %) in femoral tunnel depth and height without intergroup differences. It is likely that both techniques may not provide constant femoral tunnel position, which might be due to inherent error of arthroscopic view and different flexion angles during femoral tunnel placement.
Although the location of tibial tunnel is a little posterior to avoid roof impingement in traditional ACL reconstruction, the tibial tunnel is placed in the centre of footprint in current anatomical ACL reconstruction [11, 20]. Although we could make anatomical tibial tunnel regardless of techniques in this study, wider variability was noted in the anteroposterior than in the mediolateral position of the tibial tunnel (ranges, 32 % in AP and 14 % in ML position). These results were similar to Topliss and Webb’s study [27]. They found higher variability between surgeons on the tibial sagittal depth measure than on the tibial placement in the coronal plane. It is likely that inter-surgeon variability reflects the range of preferences and occasional error inherent to ACL reconstruction.
The trans-portal technique for ACL reconstruction has a well-known risk of short femoral tunnel length, which is consistent with the results of our study (34.7 mm in trans-portal group) [3, 6, 16, 22, 29]. Moreover, the length of femoral tunnel in outside-in techniques was also a little shorter than the previously reported results of trans-tibial techniques. However, the variability of tunnel length was wider in trans-portal technique than in outside-in techniques (34 vs. 36.8 mm).
Recently, it was reported in several studies that trans-portal technique in ACL reconstruction had a risk of acute angle between the graft and the femoral tunnel in extension [12, 17, 22–24, 28]. Kim et al. [12] showed that the graft bending angle was more acute in outside-in technique, which was consistent with the result of this study (115.6° in trans-portal and 98° in outside-in techniques). However, the range of graft bending angle was more variable in trans-portal technique than in outside-in technique, which might be due to different flexion angles in trans-portal technique [2, 19].
For interpretation of the study results, the following points need to be considered. First, this study lacks any report of clinical outcome differences within the technique or among surgeons. It is unclear what magnitude difference in tunnel measurement constitutes a significant clinical difference. Second, this study included only four surgeons (two each in trans-portal and in outside-in techniques). Third, the measurement of femoral tunnel using the Bernard’s method was determined on the radiographs, not in the CT image. However, several studies [12, 20, 23, 25] used this method to evaluate femoral tunnel location on the CT images. Last, surgeon’s preference or inherent error could reflect the range of tunnel variability.
Conclusions
Although both trans-portal and outside-in techniques in ACL reconstruction can provide relatively consistent in femoral and tibial tunnel locations, trans-portal technique showed high variability in femoral tunnel length and graft bending angles than outside-in techniques. The graft tunnel angle showed significant acute angle in outside-in technique. Therefore, the outside-in ACL reconstruction can be considered as the more effective method for surgeons to make consistent tunnel than the trans-portal technique.
References
Alavekios D, Peterson A, Patton J, McGarry MH, Lee TQ (2014) The relation between knee flexion angle and anterior cruciate ligament femoral tunnel characteristics: a cadaveric study comparing a standard and a far anteromedial portal. Arthroscopy 30:1468–1474
Basdekis G, Abisafi C, Christel P (2008) Influence of knee flexion angle on femoral tunnel characteristics when drilled through the anteromedial portal during anterior cruciate ligament reconstruction. Arthroscopy 24:459–464
Bedi A, Raphael B, Maderazo A, Pavlov H, Williams RJ (2010) Transtibial versus anteromedial portal drilling for anterior cruciate ligament reconstruction: a cadaveric study of femoral tunnel length and obliquity. Arthroscopy 26:342–350
Bernard M, Hertel P, Hornung H, Cierpinski T (1997) Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg 10:14–21
Brown CH Jr, Spalding T, Robb C (2013) Medial portal technique for single-bundle anatomical anterior cruciate ligament (ACL) reconstruction. Int Orthop 37:253–269
Chang CB, Yoo JH, Chung BJ, Seong SC, Kim TK (2010) Oblique femoral tunnel placement can increase risks of short femoral tunnel and cross-pin protrusion in anterior cruciate ligament reconstruction. Am J Sports Med 38:1237–1245
Edwards A, Bull AM, Amis AA (2007) The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament, part 1: tibial attachment. Knee Surg Sports Traumatol Arthrosc 15(12):1414–1421
Harner CD, Baek GH, Vogrin TM et al (1999) Quantitative analysis of human cruciate ligament insertions. Arthroscopy 15:741–749
Hwang MD, Piefer JW, Lubowitz JH (2012) Anterior cruciate ligament tibial footprint anatomy: systematic review of the 21st century literature. Arthroscopy 28(5):728–734
Keller TC, Tompkins M, Economopoulos K et al (2014) Tibial tunnel placement accuracy during anterior cruciate ligament reconstruction: independent femoral versus transtibial femoral tunnel drilling techniques. Arthroscopy 30(9):1116–1123
Kim HS, Seon JK, Jo AR (2013) Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res 25:165–173
Kim JG, Wang JH, Ahn JH, Kim HJ, Lim HC (2013) Comparison of femoral tunnel length between transportal and retrograde reaming outside-in techniques in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21:830–838
Kopf S, Forsythe B, Wong AK et al (2012) ACL reconstruction technique fails to position drill tunnels anatomically in vivo 3D CT study. Knee Surg Sports Traumatol Arthrosc 20:2200–2207
Kopf S, Musahl V, Tashman S et al (2009) A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc 17:213–219
Lertwanich P, Martins CA, Asai S et al (2011) Anterior cruciate ligament tunnel position measurement reliability on 3-dimensional reconstructed computed tomography. Arthroscopy 27:391–398
Lubowitz JH, Konicek J (2010) Anterior cruciate ligament femoral tunnel length: cadaveric analysis comparing anteromedial portal versus outside-in technique. Arthroscopy 26:1357–1362
Nishimoto K, Kuroda R, Mizuno K et al (2009) Analysis of the graft bending angle at the femoral tunnel aperture in anatomic double bundle anterior cruciate ligament reconstruction: a comparison of the transtibial and the far anteromedial portal technique. Knee Surg Sports Traumatol Arthrosc 17:270–276
Noh JH, Roh YH, Yang BG, Yi SR, Lee SY (2013) Femoral tunnel position on conventional magnetic resonance imaging after anterior cruciate ligament reconstruction in young men: transtibial technique versus anteromedial portal technique. Arthroscopy 29:882–890
Osaki K, Okazaki K, Tashiro Y, Matsubara H, Iwamoto Y (2015) Influences of knee flexion angle and portal position on the location of femoral tunnel outlet in anterior cruciate ligament reconstruction with anteromedial portal technique. Knee Surg Sports Traumatol Arthrosc 23:777–784
Parkinson B, Gogna R, Robb C, Thompson P, Spalding T (2015) Anatomic ACL reconstruction: the normal central tibial footprint position and a standardised technique for measuring tibial tunnel location on 3D CT. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3683-8
Piefer JW, Pflugner TR, Hwang MD, Lubowitz JH (2012) Anterior cruciate ligament femoral footprint anatomy: systematic review of the 21st century literature. Arthroscopy 28:872–881
Robin BN, Jani SS, Marvil SC et al (2015) Advantages and disadvantages of transtibial, anteromedial portal, and outside-in femoral tunnel drilling in single-bundle anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 31:1412–1417
Shin YS, Ro KH, Lee JH, Lee DH (2013) Location of the femoral tunnel aperture in single-bundle anterior cruciate ligament reconstruction: comparison of the transtibial, anteromedial portal, and outside-in techniques. Am J Sports Med 41:2533–2539
Sohn OJ, Lee DC, Park KH, Ahn HS (2014) Comparison of the modified transtibial technique, anteromedial portal technique and outside-in techniques in ACL reconstruction. Knee Surg Relat Res 26:241–248
Song EK, Kim SK, Lim HA, Seon JK (2014) Comparisons of tunnel-graft angle and tunnel length and position between transtibial and transportal techniques in anterior cruciate ligament reconstruction. Int Orthop 38:2357–2362
Tashiro Y, Okazaki K, Uemura M et al (2014) Comparison of transtibial and transportal techniques in drilling femoral tunnels during anterior cruciate ligament reconstruction using 3D-CAD models. Open Access J Sports Med 5:65–72
Topliss C, Webb J (2014) An audit of tunnel position in anterior cruciate ligament reconstruction. Arthroscopy 30:1116–1123
Tudisco C, Bisicchia S (2012) Drilling the femoral tunnel during ACL reconstruction: transtibial versus anteromedial portal techniques. Orthopedics 35:1166–1172
Wang JH, Kim JG, do Lee K, Lim HC, Ahn JH (2012) Comparison of femoral graft bending angle and tunnel length between transtibial technique and transportal technique in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:1584–1593
Wolf BR, Ramme AJ, Wright RW et al (2013) Variability in ACL tunnel placement: observational clinical study of surgeon ACL tunnel variability. Am J Sports Med 41:1265–1273
Yau WP, Fok AW, Yee DK (2013) Tunnel positions in transportal versus transtibial anterior cruciate ligament reconstruction: a case control magnetic resonance imaging study. Arthroscopy 29:1047–1052
Youm YS, Cho SD, Lee SH, Youn CH (2014) Modified transtibial versus anteromedial portal technique in anatomic single-bundle anterior cruciate ligament reconstruction: comparison of femoral tunnel position and clinical results. Am J Sports Med 42:2941–2947
Acknowledgments
This study was supported by a Grant of the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2014R1A1A2059147).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sim, JA., Kim, JM., Lee, S. et al. Comparison of tunnel variability between trans-portal and outside-in techniques in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 25, 1227–1233 (2017). https://doi.org/10.1007/s00167-015-3950-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3950-8