Abstract
Purpose
The goal of this study was to identify factors prior to surgery that are associated with an increased length of hospital stay after TKA using a fast-track protocol.
Materials and methods
In total, 879 consecutive patients who underwent primary TKA were included in this retrospective cohort study. A length of stay greater than or equal to three nights was considered an increased length of hospital stay. Univariable and multivariable generalized linear mixed models were used to identify potential factors associated with increased length of hospital stay.
Results
Length of hospital stay was significantly associated with age [OR 1.01 (95 % CI 1.01–1.02); p < 0.001], gender [female vs. male, OR 1.07 (95 % CI 1.00–1.15); p = 0.04], ASA [ASA III/IV vs. ASA I, OR 1.22 (95 % CI 1.06–1.39); p = 0.005], living situation (alone vs. together, OR 1.08 (95 % CI 1.00–1.16); p = 0.04], neurological comorbidities [OR 1.14 (95 % CI 1.06–1.23); p < 0.001], musculoskeletal comorbidities [OR 0.91 (95 % CI 0.85–0.97); p = 0.005], anaesthesia [spinal vs. general, OR 0.86 (95 % CI 0.76–0.97); p = 0.02], and weekday of surgery [Thursday vs. Monday, OR 1.12 (95 % CI 1.02–1.23); p = 0.02].
Conclusions
Older age, female gender, ASA III/IV, people living alone, the presence of neurological comorbidities, general anaesthesia and surgery on Thursday were associated with an increased length of hospital stay. In clinical practice, the knowledge of factors associated with an increased length of hospital stay can be used to further optimize peri-operative protocols for patients at risk for an increased length of hospital stay after TKA.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last few years, length of hospital stay (LOS) after total knee arthroplasty (TKA) has decreased following the introduction of fast-track protocols [12]. These protocols focus on pain management, organizational factors, limiting peri- and post-operative complications, and promote early mobilization [12]. Fast-track TKA has been shown to be safe and feasible, with similar or better outcome for the patient [6, 11].
In the Reinier the Graaf hospital, a large teaching hospital in the Netherlands, a fast-track protocol for primary TKA was introduced in 2009. Introduction was incremental and was complete by February 2011. After the implementation of this fast-track rehabilitation protocol, the mean LOS for primary TKA decreased from 4.5 to 3.0 nights for unselected patients in our hospital (unpublished data). However, despite the mean reduction in LOS, several patients still have an extended hospital stay. In literature, LOS after primary TKA has been reported to be influenced by pre-, peri-, and post-operative variables, such as comorbidities, pain, anaesthetic technique, age, complications, orthostatic intolerance, muscle function and inadequate social support. [5, 12, 14, 16].
The proper identification of patients who need more rehabilitation time and more extensive care might provide further optimization of discharge and rehabilitation planning. Therefore, the goal of this study was to identify factors prior to surgery that are associated with an increased LOS after TKA using a fast-track protocol.
It was hypothesized that age, comorbidities and living situation are factors that influence LOS after TKA using a fast-track protocol.
Materials and methods
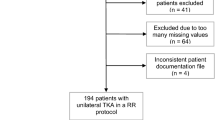
A total of 879 consecutive patients who underwent primary TKA between 1 February 2011 and 1 January 2015 were included in this retrospective cohort study. All surgeries were performed in a fast-track setting. Patients were admitted to the hospital at the day of surgery.
The procedures were performed by seven orthopaedic surgeons. All surgeons used the medial parapatellar approach to perform the TKA, except for one patient who was operated on by a lateral approach. All patients received the NexGen® LPS-High Flex Knee (Zimmer®, Warsaw, IN, USA) implant. The preferred type of anaesthesia was spinal anaesthesia with a low dose of bupivacaine (4–6 mg). If spinal anaesthesia was contraindicated, patients received general anaesthesia. No drains were used post-operatively. Furthermore, propofol was given by target controlled infusion, which is often used in anaesthesia to control the concentration of selected drugs in the plasma or at the site of its effect. A standardized protocol of oral post-operative medication consisted of 1 g paracetamol four times a day, celecoxib 200 mg, gabapentin 300 mg and tramadol 100 mg (one dose of each, only for the first night after operation). Rescue medication consisted of the opioid piritramide 10 mg (maximum six times a day) and extra celecoxib 200 mg (maximum once a day). All patients received local infiltration analgesia during surgery (ropivacaine and epinephrine). A tourniquet was used for all patients until 31 December 2012. From 1 January 2013 no tourniquet was used during surgery. From 1 January 2013 all patients received 1000 mg tranexamic acid intravenously. Post-operative physiotherapy was undertaken twice a day, starting four to six hours after surgery and focused on regaining function, movement and gait. The discharge criteria were both functional and clinical. Patients had to be able to walk 30 m with crutches, to climb stairs, to get dressed independently and to go to the toilet independently. In addition, adequate pain relief had to be achieved with oral medication before discharge, with a VAS <3 at rest and <5 during mobilization. Furthermore, if the patient had a raised temperature or severely decreased haemoglobin levels, the patient’s hospital stay had to be prolonged.
The outcome was LOS, which was defined as the number of nights spent in the hospital. LOS was dichotomized by performing a median split. A LOS greater than or equal to the median was considered a prolonged LOS. Potential factors associated with a prolonged hospital stay were obtained from patient files. These included age, living situation (alone vs. living together with cohabitants), gender, BMI, ASA classification, comorbidities, weekday of surgery and surgeon.
Health status was scored using the ASA classification and categorized into ASA I, ASA II and ASA III/IV. For each patient, comorbidities were assessed and categorized into cardiovascular, pulmonary, neurological, musculoskeletal, endocrine and ‘other’ comorbidities. Comorbidities were dichotomized in either present or absent. The comorbidities were independently extracted from the patient files by three reviewers (CL and TM, medical students, NM, senior scientist). Disagreements in these assessments were solved by discussion, and a final decision of a fourth reviewer (HV) was not necessary.
Since this study did not fall under the scope of the Medical Research Involving Human Subjects Act in the Netherlands, no ethical approval was necessary.
Statistical analysis
The associations between each variable and LOS were examined with generalized linear mixed models. We considered a given surgeon’s TKAs to be non-independent, and therefore, we nested patients within surgeon. A random intercept for each surgeon was fit in order to control for the individual surgeon effect. Factors that were associated with the outcome in univariable analyses (p values <0.15) were included in a multivariable generalized linear mixed model. In the multivariable model p values <0.05 were considered significant.
Data analyses were performed using ‘R’ version 3.1.2 with package ‘nlme’ (R Foundation, Vienna Austria).
Results
The mean LOS for the group as a whole was 2.9 nights (±1.6) with a median of 3.0 nights. Of the total of 879 patients, 403 (45.8 %) patients had a LOS < 3 nights and 476 (54.2 %) a LOS ≥ 3 nights. Demographics of both groups are listed in Table 1.
Results of the univariable and multivariable models are presented in Table 2.
In the multivariable model, factors that were significantly associated with an increased LOS were age [OR 1.01 (95 % CI 1.01–1.02); p < 0.001], gender [female vs. male; OR 1.07 (95 % CI 1.00–1.15); p = 0.04] ASA [ASA III/IV vs. ASA I; OR 1.22 (95 % CI 1.06–1.39); p = 0.005], living situation [alone vs. together; OR 1.08 (95 % CI 1.00–1.16); p = 0.04], neurological comorbidities [OR 1.14 (95 % CI 1.06–1.23); p < 0.001], general anaesthesia [spinal vs. general (OR 0.86 (95 % CI 0.76–0.97); p = 0.02] and weekday of surgery [Thursday vs. Monday; OR 1.12 (95 % CI 1.02–1.23); p = 0.02] (Table 2). Musculoskeletal comorbidities [OR 0.91 (95 % CI 0.85–0.97); p = 0.005] were significantly associated with a decreased LOS after TKA.
Discussion
The most important finding of the present study was that an increased LOS was associated with older age, female gender, ASA III/IV, people living alone, the presence of pulmonary or neurological comorbidities, general anaesthesia and surgery on Thursday. The mean LOS in our study was 2.9, which is shorter than what most other studies that evaluate factors associated with LOS after TKA report [9, 15, 17, 18, 23]. This difference might be explained by the fact that most of these studies did not include a fast-track protocol. However, even studies that did include a fast-track protocol reported an average LOS between 3 and 5 days after TKA. [5, 7, 11, 21].
In the present study, age was associated with a prolonged LOS. This is in accordance with other studies [5, 9, 11, 15, 17, 18, 23] on LOS after TKA, in fast-track settings as well as in non-fast-track settings. Moreover, in another study at our institution on LOS after THA in a fast-track programme, age was also found to be associated with a prolonged hospital stay [4].
General anaesthesia was found to be associated with an increased hospital stay when compared to spinal anaesthesia with a low dose of bupivacaine. Local anaesthesia is preferable over general anaesthesia in a fast-track setting because it has been shown to result in a decrease in complications and side effects [13]. Moreover, local anaesthesia improves early mobilization and rehabilitation [3, 13].
As part of our fast-track protocol, all patients received local infiltration analgesia during surgery. According to Holm et al. [5] local infiltration analgesia has little or no effect beyond 24 h after surgery to achieve a short stay of approximately 3 days. However, if LOS after TKA shortens, local infiltration analgesia might be predictive for an early discharge.
Patients with ASA III or IV were more likely to have a longer hospital stay than patients with ASA I. This is in accordance with other studies [9, 21]. ASA provides a classification system for the fitness of a patient; however, it does not take into account all relevant comorbidities possibly associated with a prolonged LOS. Therefore, the patients’ comorbidities were included in our analyses. The presence of neurological comorbidities was associated with an increased LOS. Ong and Pua also found that a greater number of comorbidities were associated with an increased LOS after primary TKA [15]. In the study of Jans et al. [8] pre-operative anaemia, cardiac disease and pulmonary disease appeared to be risk factors for a prolonged LOS after primary TKA. Jorgensen et al. [11] showed that cardiopulmonary disease was significantly related to a LOS of more than 4 days. In our study, however, cardiovascular comorbidities were not associated with a prolonged LOS after primary TKA. No explanation could be found for the association between the presence of musculoskeletal comorbidities and a decreased LOS.
Gender did have a significant effect on LOS following TKA (p = 0.04), which is in accordance with other studies [7, 22]. However, Tan et al. [18] did not find an association between gender and LOS.
In our model, living situation was associated with LOS. Others also found an association between living situation and LOS following TKA [11, 15, 18].
BMI was not significantly associated with an increase in hospital stay after TKA. This is in accordance with the results of Smith et al. [17] and Van der Belt et al. [21]. In contrast, others did find LOS to be influenced by BMI [2, 9]. An elevated BMI was associated with an increased risk of complications following total joint arthroplasty [2], and therefore, an association of BMI with LOS might have been expected.
Surgeries performed on Thursday were associated with an increased LOS, even though discharge was also possible during weekends. However, in general less personnel is present during weekends, which might explain the differences. This is in agreement with the results of Husted et al. [7], although others [17, 21] did not show significant differences between weekdays.
Some limitations should be discussed. First, we performed a median split to dichotomize LOS. In the absence of a prior cut-off point the most common approach is to take the sample median. Using the sample median implies that various cut-off points will be used in different studies so that their results might not easily be compared. In addition, using the sample median means that much information is lost (e.g. all the values above the median are considered equal), so the statistical power to detect a relation might be reduced. However, this appears not to have been a problem in the present study. [1] Several others used the median as cut-off point to define an increased hospital stay. [4, 9].
Second, pre-operative knee scores (patient-reported outcome measures) were not available for all patients. Therefore, we could not include these variables in our model. Moreover, the effects of walking aids, mobility and post-operative ROM at day 0 were not included in the present study although these have been reported to be associated with LOS after primary TKA in other studies. Moreover, we did not include smoking and alcohol use in our study. Smoking and alcohol did not have any influence on LOS in a fast-track setting, according to Jorgensen et al. [10]. In contrast, in studies with a LOS of about 8–14 days, patient who smoked or drank >2 units of alcohol daily were regarded as having a higher risk of developing post-surgical complications leading to an increased hospital stay [19, 20].
Another limitation is that no psychological instruments were incorporated in our multivariable approach. Literature has suggested that pre-operative levels of depression and internalizing/catastrophizing are associated with less improvement in pain and physical functioning after TKA and with a prolonged hospital stay [15, 23]. These authors hypothesized that patients who catastrophize pre-operatively will tend to avoid movements and physical activity post-operatively, whereas in a fast-track setting, patients are mobilized on the day of surgery. Therefore, further research should investigate the influence of pre-operative levels of depression and catastrophizing on outcome and LOS after TKA in a fast-track setting.
Conclusion
In conclusion, older age, female gender, ASA III/IV, people living alone, the presence of pulmonary or neurological comorbidities, general anaesthesia and surgery on Thursday were associated with a prolonged LOS after primary TKA using a fast-track protocol. In clinical practice, the knowledge of factors associated with an increased LOS can be used to further optimize perioperative protocols for patients at risk for an increased LOS after TKA.
References
Altman DG, Royston P (2006) The cost of dichotomising continuous variables. BMJ 332:1080
Alvi HM, Mednick RE, Krishnan V, Kwasny MJ, Beal MD, Manning DW (2015) The effect of BMI on 30 day outcomes following total joint arthroplasty. J Arthroplasty 30:1113–1117
Awad IT, Cheung JJ, Al-Allaq Y, Conroy PH, McCartney CJ (2013) Low-dose spinal bupivacaine for total knee arthroplasty facilitates recovery room discharge: a randomized controlled trial. Can J Anaesth 60:259–265
Hartog YM, Mathijssen NM, Hannink G, Vehmeijer SB (2015) Which patient characteristics influence length of hospital stay after primary total hip arthroplasty in a ‘fast-track’ setting? Bone Joint J 97-B:19–23
Holm B, Kristensen MT, Myhrmann L, Husted H, Andersen LO, Kristensen B, Kehlet H (2010) The role of pain for early rehabilitation in fast track total knee arthroplasty. Disabil Rehabil 32:300–306
Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL, Kehlet H (2010) What determines length of stay after total hip and knee arthroplasty? A nationwide study in Denmark. Arch Orthop Trauma Surg 130:263–268
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 79:168–173
Jans O, Jorgensen C, Kehlet H, Johansson PI (2014) Role of preoperative anemia for risk of transfusion and postoperative morbidity in fast-track hip and knee arthroplasty. Transfusion 54:717–726
Jonas SC, Smith HK, Blair PS, Dacombe P, Weale AE (2013) Factors influencing length of stay following primary total knee replacement in a UK specialist orthopaedic centre. Knee 20:310–315
Jorgensen CC, Kehlet H (2013) Outcomes in smokers and alcohol users after fast-track hip and knee arthroplasty. Acta Anaesthesiol Scand 57:631–638
Jorgensen CC, Kehlet H (2013) Role of patient characteristics for fast-track hip and knee arthroplasty. Br J Anaesth 110:972–980
Kehlet H (2013) Fast-track hip and knee arthroplasty. Lancet 381:1600–1602
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Napier RJ, Spence D, Diamond O, O’Brien S, Walsh T, Beverland DE (2013) Modifiable factors delaying early discharge following primary joint arthroplasty. Eur J Orthop Surg Traumatol 23:665–669
Ong PH, Pua YH (2013) A prediction model for length of stay after total and unicompartmental knee replacement. Bone Joint J 95-B:1490–1496
Schneider M, Kawahara I, Ballantyne G, McAuley C, Macgregor K, Garvie R, McKenzie A, Macdonald D, Breusch SJ (2009) Predictive factors influencing fast track rehabilitation following primary total hip and knee arthroplasty. Arch Orthop Trauma Surg 129:1585–1591
Smith ID, Elton R, Ballantyne JA, Brenkel IJ (2008) Pre-operative predictors of the length of hospital stay in total knee replacement. J Bone Joint Surg Br 90:1435–1440
Tan C, Loo G, Pua YH, Chong HC, Yeo W, Ong PH, Lo NN, Allison G (2014) Predicting discharge outcomes after total knee replacement using the risk assessment and predictor tool. Physiotherapy 100:176–181
Tonnesen H, Kehlet H (1999) Preoperative alcoholism and postoperative morbidity. Br J Surg 86:869–874
Turan A, Mascha EJ, Roberman D, Turner PL, You J, Kurz A, Sessler DI, Saager L (2011) Smoking and perioperative outcomes. Anesthesiology 114:837–846
van den Belt L, van Essen P, Heesterbeek PJ, Defoort KC (2015) Predictive factors of length of hospital stay after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:1856–1862
Vincent HK, Alfano AP, Lee L, Vincent KR (2006) Sex and age effects on outcomes of total hip arthroplasty after inpatient rehabilitation. Arch Phys Med Rehabil 87:461–467
Witvrouw E, Pattyn E, Almqvist KF, Crombez G, Accoe C, Cambier D, Verdonk R (2009) Catastrophic thinking about pain as a predictor of length of hospital stay after total knee arthroplasty: a prospective study. Knee Surg Sports Traumatol Arthrosc 17:1189–1194
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mathijssen, N.M.C., Verburg, H., van Leeuwen, C.C.G. et al. Factors influencing length of hospital stay after primary total knee arthroplasty in a fast-track setting. Knee Surg Sports Traumatol Arthrosc 24, 2692–2696 (2016). https://doi.org/10.1007/s00167-015-3932-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3932-x