Abstract
Purpose
To assess the efficacy of intra-articular hyaluronic acid (HA) injections and exercise-based rehabilitation (EBR) programme, administered as isolated or integrated for the treatment of knee osteoarthritis.
Methods
One hundred sixty-five patients affected by moderate degrees of knee OA were randomly divided into three groups. Group 1 (HA) underwent three HA injections (one every 2 weeks); group 2 (EBR) underwent 20 treatment sessions in a month of an individualized programme; and group 3 (HA + EBR) received both treatments simultaneously. Primary outcome was the Italian version of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index; secondary outcome was the evaluation of active range of movement (AROM). All patients were evaluated before and 1, 3 and 6 months after treatment. Significance was set at p < 0.05.
Results
Two patients in each group were lost to follow-up. No adverse events occurred. All groups experienced improvements at 1-month follow-up. No further improvements could be detected within groups over time. At 1-month follow-up, WOMAC pain subscale showed significant improvement in group 3 compared to group 1 (p = 0.043). WOMAC pain, stiffness and function subscales showed that group 2 significantly worsened between 1 and 6 months after treatment (p = 0.004, p = 0.026 and p = 0.025, respectively). AROM revealed no significant differences between and within groups over time.
Conclusions
Intra-articular HA injections and individualized rehabilitation programmes administered in isolation or in combination are effective in improving knee function and pain relief. The combined treatment showed the greatest pain relief at 1-month follow-up compared to either in isolation. Compared to the previous studies, this is the first study, which proposed an EBR programme tailored to the compartment of the knee joint most involved in the degenerative process.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (OA) is one of the most common joint disorders in the world, and its prevalence increases with age. It affects approximately 15 % of adults older than 45 years and about 50 % of those aged over 75 years [2, 25]. Numerous treatment strategies have been proposed, and several guidelines have been produced by international scientific authorities, such as the European League Against Rheumatism (EULAR) [11], the American College of Rheumatology (ACR) [13], the Osteoarthritis Research Society International (OARSI) [23, 38–40], the UK National Institute for Health and Clinical Excellence (NICE) [26], the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) [5]. A broader approach includes prevention through the reduction in risk factors, such as obesity [9, 11, 16], and combined interventions that can slow down the progression of the disease. Non-surgical treatments, which aim to reduce pain and improve or, at least, stabilize function, include: physical therapy and/or rehabilitation programmes, use of oral corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs), intra-articular injections of corticosteroids, hyaluronic acid (HA) or platelet concentrates [3, 4, 6, 7, 12, 17, 22, 24, 28].
According to the recent literature, exercise therapy remains one of the first-line options [12, 33]. It is fundamental to restore a muscle balance and a correct load distribution, thus relieving pain and improving function. However, the optimal exercise regimen has not been identified yet [20]. Several studies showed that intra-articular injections of HA and oral NSAIDs have comparable efficacy on symptoms, but fewer systemic adverse events have been reported in the HA trials [4]. On the other hand, in comparison with the intra-articular corticosteroids injections, the HA showed longer term benefits, especially between the 5th and 13th week after treatment [17].
Comparative studies between intra-articular HA injections and physical therapy did not show statistically significant differences between the two treatments [18, 20]. However, few studies assessed the efficacy of isolated intra-articular injections or exercise-based rehabilitation (EBR) or physical therapy modalities compared to integrated treatments [14, 34]. No previous studies compared the clinical efficacy of intra-articular HA injections isolated or associated with an EBR programme tailored to the compartment of the knee joint most involved in the degenerative process (medial or lateral tibio-femoral or patello-femoral). The purpose of the present study was to assess the efficacy of intra-articular HA injections and individualized EBR programme, administered as isolated or integrated therapeutic regimens for the treatment of knee OA. The hypothesis of the study was that the difference between the three therapeutic regimens is significant.
Material and methods
This study was designed as a blinded, prospective, randomized controlled study and took place from February 2009 through January 2013.
Participants
Participants were recruited among patients referred for knee pain to the outpatient clinic of the Orthopaedic Institute of the Department of Geriatrics, Neuroscience and Orthopaedics, “Agostino Gemelli” University Hospital at the Catholic University of Rome, Italy, between June 2009 and July 2012.
Two hundred and one patients who have accepted our invitation to enter the study and who have signed an agreement disclosure form were enlisted for this study. All patients were carefully informed about the expected benefits of the procedures.
Men and women aged 18 years or older in good general health with knee OA according to the ACR diagnostic criteria [13] were eligible for inclusion. Knee malalignment (varus or valgus deformity) and OA were confirmed by radiographic examinations in different views: weight-bearing anteroposterior (AP), weight-bearing posteroanterior (PA) according to Rosenberg, standard lateral view and axial patella view at 30° of flexion. Radiographic evidence of knee OA was graded according to the Kellgren and Lawrence [21] classification for the tibio-femoral OA and according to Iwano et al. [15] for the patello-femoral OA. Patients with no radiographic evidence of knee OA or with severe OA (grade IV according to Kellgren and Lawrence [21] and/or stage IV according to Iwano et al. [15]) were excluded. Other exclusion criteria were: inability or unwillingness to sign informed consent, intra-articular injections with steroids or hyaluronic acid in prior 6 months, physiotherapy for knee problems in prior 6 months, congenital or acquired inflammatory or neurological (systemic or local) diseases involving the knee, chronic treatment with steroids or NSAIDs and cognitive or psychiatric disorders.
Randomization
Eligible participants were referred to a physician not involved in the study and provided with detailed information about the experimental protocol. Patients were randomly assigned to one of the three groups of treatment using a random sequence generator (www.random.org). The randomization list was kept by an independent researcher not involved in the study, and allocation to one of the three treatment arms was revealed to the patients at the time of confirmation of enrolment. Allocation concealment was performed using closed envelopes.
Interventions
Patients assigned to group 1 (HA group) underwent three intra-articular injections (one injection every 2 weeks) of high molecular weight hyaluronic acid (Orthovisc 2 ml; 15 mg/ml; Anika Therapeutics Inc., Bedford, MA). All devices were supplied as sterile, pre-filled syringes containing a clear colourless solution. Injections were given by a physician experienced in the procedure using a 21-gauge needle in aseptic conditions.
Patients assigned to group 2 (EBR group) received a detailed programme of knee exercises for a total of 20 treatment sessions in a month (five sessions per week). Patients were further divided into three subgroups based on the knee compartment that was more involved in the degenerative process (medial or lateral tibio-femoral compartment; patello-femoral compartment) (Appendix).
Patients assigned to group 3 (HA + EBR group) received both treatments at the same time: three intra-articular injections (one injection every 2 weeks) of high molecular weight hyaluronic acid (Orthovisc 2 ml) associated with the same EBR programme assigned to the patients in group 2.
In the time interval between the beginning of treatment and the 6-month follow-up, patients were required to refrain from any additional pharmacological or physical treatment for pain management. No instructions regarding activity or home exercise programme during or following supervised therapy were provided to the patients during the study.
Outcome measures
The primary outcome of the study was the Italian version of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index, which was proved to be valid and reliable, with metric properties in agreement with the original version [31]. The scale aims to measure dysfunction and pain associated with OA of the lower extremities by assessing 17 functional activities, 5 pain-related activities and 2 stiffness categories. The Italian WOMAC is available only in its visual analogue scale (VAS) format, and all 24 items are rated by the subject on a 100-mm VAS ranging from 0 (indicating no pain, stiffness or difficulty) to 100 (indicating extreme pain, stiffness or difficulty). The range of the WOMAC scores is: 0–500 for pain, 0–200 for stiffness and 0–1700 for function.
Secondary outcome measure was the objective evaluation of active range of movement (AROM). It was measured with a goniometer, marked in 1° increments. This device has already been reported as reliable (ICC = 0.91–0.99) [29]. The axes of the goniometer were placed at the intersection of the thigh and shank at the knee joint centre of rotation (lateral femoral condyle). One arm was placed along the lateral aspect of the thigh, following the line from the knee joint to the greater trochanter at the hip. The other arm was placed along the lateral aspect of the fibula. Measurement of knee flexion was taken in the supine position by simultaneously flexing the hip and knee, with the foot on the measured side resting on the table as far as possible. The fully extended knee was considered zero position, and the degrees of maximum flexion were recorded. Measurements were repeated three times, and average values were considered for data analysis.
All patients were clinically evaluated before treatment (baseline, T 0) and 1 month (T 1), 3 months (T 3) and 6 months (T 6) after treatment. Outcome measures were determined at baseline and follow-up visits by an investigator blind to the participant allocation.
Assessment of baseline characteristics
The following baseline variables were recorded and considered as potential predictors of outcome: age, gender, body mass index (BMI), timing of symptoms, previous surgeries to the affected knee, compartment involved, Kellgren–Lawrence tibio-femoral OA grade, Iwano patello-femoral OA stage, baseline WOMAC scores and baseline knee AROM.
The protocol and informed consent process have been approved by the local ethics committee (Catholic University, Rome, P/481/CE/2011).
Statistical analysis
Statistical analysis was performed using the SPSS version 19.0 software (IBM SPSS Statistics, Chicago, IL, USA). For all the outcomes and predictors, normality of data was ascertained by the one-sample Kolmogorov–Smirnov’s test for continuous variables and the Chi-square test for categorical variables. Differences in the WOMAC scores between groups over time were analysed via multiple analysis of covariance (MANCOVA) for repeated measures. All the baseline characteristics were included in the model and handled as covariates. A two-factor (time × group) analysis was performed to evaluate the overall group effect, overall time effect and the interaction between group and time. Both multivariate and univariate approaches were tested, and the multivariate model was selected as it yielded the highest p values. In addition, comparisons of WOMAC scores within groups over time were made via an analysis of variance (ANOVA) for repeated measures. Moreover, comparisons of WOMAC scores between groups at each follow-up time point were made via an analysis of covariance (ANCOVA) model adjusted for all the baseline characteristics. Multiple pairwise comparisons within groups and between groups were made by means of post hoc test with Bonferroni’s correction in order to determine the time point and the group in which the observed treatment effect occurred. The AROM was analysed in a similar manner. For all tests, significance was set at p < 0.05.
Missing data at follow-up were managed according to the last observation carried forward (LOCF) method [32]. Data were analysed according to the intention-to-treat principle. Data were expressed as frequencies (percentages) for categorical variables and as means ± standard deviations (SD) or medians and interquartile ranges for normally and non-normally distributed continuous variables, respectively.
Sample size was calculated according to the primary outcome measure (WOMAC scale). Previous studies on pharmacological treatment of knee OA reported that the responsiveness of the WOMAC global score showed a standardized effect size of 0.7. Therefore, a sample size of 44 cases per group was determined using an a priori model of power analysis and a two-sided alternative hypothesis, given an alpha = 0.05 and a power (1 − β) = 0.90. The number of participants was increased to 55 per group to account for a 20 % rate of loss at follow-up.
Results
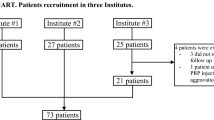
A total of 201 patients were eligible, and 165 were randomized for the interventions (Fig. 1). Participants in the three groups did not differ with respect to all the baseline characteristics considered as potential predictors of outcome (Table 1).
All participants in the groups 1 and 3 completed the treatment protocol, while two patients in the group 2 discontinued the protocol after the first week. A total of six participants (3.6 %) (two in each group) were lost to follow-up during the first month of the study. All these patients were called many times but refused to return for follow-up as they lived far from our region. None of the other participants in the three groups missed more than one follow-up visit. Thus, 157 patients (95 %) completed at least two follow-up visits. No adverse events were observed in each treatment arm.
Effects of treatments on primary and secondary outcome measures
As a whole, data analysis revealed that all treatment groups experienced early improvements in pain relief, stiffness and function compared with baseline values. However, after 1-month follow-up, a deterioration of results could be detected within groups over time, albeit significant improvements were still noted at 6 months from baseline.
Analysis of WOMAC pain subscale (Table 2) revealed that at 1 month, group 3 had a significantly better score than group 1. No other significant differences between groups were observed at the subsequent follow-ups. Within-group analysis revealed no significant changes over time in group 1, while groups 2 and 3 showed a significant deterioration of results between T 1 and T 6. No significant overall group effect (F = 1.522, p = n.s.), no overall time effect (F = 1.890, p = n.s.) and no time × group interaction (F = 0.846, p = n.s.) could be found.
Analysis of WOMAC stiffness subscale (Table 3) showed no significant differences between groups at each follow-up. Group 2 significantly worsened between T 1 and T 6, reaching no significant differences from baseline values. No significant overall group effect (F = 0.930, p = n.s.), no overall time effect (F = 0.991, p = n.s.) and no time × group interaction (F = 0.311, p = n.s.) could be found.
Analysis of WOMAC function subscale (Table 4) showed no significant differences between groups at each follow-up. Within-group analysis revealed that group 2 significantly worsened between T 1 and T 6. No significant overall group effect (F = 1.444, p = n.s.), no overall time effect (F = 1.071, p = n.s.) and no time × group interaction (F = 0.491, p = n.s.) were detected.
Analysis of AROM (Table 5) revealed no significant differences between and within groups over time. No significant overall group effect (F = 1.242, p = n.s.), no overall time effect (F = 1.076, p = n.s.) and no time × group interaction (F = 0.642, p = n.s.) could be found.
Discussion
The main purpose of the present trial was to determine the efficacy of intra-articular HA injections and individualized EBR programmes administered in isolation or in combination. All treatment arms showed an early significant improvement from baseline in the primary outcome measures. After the first month, results maintained stable or deteriorated over time, albeit significant improvements from baseline values were still evident at the final follow-up in each group. Patients treated with HA injections showed the smallest treatment effect, but with maintenance of results over time, while patients who underwent an isolated EBR programme showed a significant deterioration of results for pain, stiffness and function between the first and the last follow-up. Patients who underwent the integrated treatment showed the greatest effect on pain reduction at 1-month follow-up, albeit the result significantly deteriorated at 6 months. No other significant differences between groups were observed at the different time intervals. No significant differences could be found between and within groups over time in the assessment of AROM. Hence, our findings showed that isolated and combined treatments improved knee pain relief and function relative to baseline and that the maintenance of this effect over time was similar in the different treatment arms. Moreover, integrated treatment provided a greater improvement in knee pain relief in the short term.
The optimal management of moderate knee OA is still under debate. It is well known that progression of knee OA depends not only on biological factors, but also on intrinsic and extrinsic mechanical factors that affect load distribution on the lower limbs. Therefore, adequate rehabilitation programmes are fundamental to control, as far as possible, mechanical factors acting on muscle contractures and restoring knee joint moments during walking. A recent systematic review revealed that individually delivered programmes tended to result in greater pain reduction and improvement in physical function, compared to class-based exercise or home-based programmes [12].
Intra-articular injections of HA, corticosteroids or platelet concentrates find their applicability in the treatment of knee OA because they might counterbalance the negative effect of inflammatory mediators on the progression of the disease, thus limiting cartilage destruction, chronic synovitis, joint capsule hypertrophy, subchondral bone remodelling and degenerative changes in ligaments and menisci. Particularly, HA injections aimed to restore the lubricating and shock-absorbing effects of the altered synovial fluid [3]. Recent reviews questioned the real cost-effectiveness of this treatment strategy [1, 3, 30, 34]. It is interesting to notice that the recently published second edition of the evidence-based guidelines approved by the American Academy of Orthopaedic Surgeons (AAOS) [16] did not recommend the use of intra-articular HA injections. Authors explained that although the literature reported statistically significant improvements with the use of high molecular weight HA preparations, these effects were not clinically significant, based on a lack of minimum clinically important improvement (MCII). Moreover, the risk of publication bias was judged to be very high [4, 16, 30]. Obviously, this strong recommendation can have a huge impact on clinical daily practice. Hence, looking at the results of the present study, we cannot affirm the superiority of one treatment over another, but we support the idea that combined treatment can substantially improve pain relief in the short term.
Previous studies [14] compared the use of isolated and combined therapies and showed results consistent with the findings of the present study, albeit this is the first study which proposed an EBR programme tailored to the compartment of the knee joint most involved in the degenerative process. Huang et al. [14] compared the effect of isolated and combined treatments with isokinetic exercises, pulsed ultrasounds and intra-articular hyaluronan therapy in 140 patients and showed that integration of the three modalities led to the best functional results. Similarly, Stitik et al. [34] assessed the efficacy of intra-articular HA injections used in isolation or in association with a home exercise programme in 60 patients. The authors reported that patients who underwent the combined treatment showed a significantly faster pain relief.
The present study has several important limitations. The main limitation is probably the absence of a placebo group, which does not allow to rule out the possibility that the improvements detected were due to a placebo effect. However, several placebo-controlled studies support the efficacy of HA [6, 8, 10, 19, 27, 35–37]. Secondly, although a radiographic staging of knee OA was performed as inclusion criteria in the study, no further imaging examinations were required at follow-up visits; therefore, it was not possible to infer about the effects of treatments on the progression of the disease. Finally, only patients with moderate knee OA were included, and then, results cannot be extended to patients with more severe grade of OA.
Conclusion
The use of intra-articular HA injections and individualized rehabilitation programmes administered in isolation or in combination for the conservative management of mild to moderate degrees of knee OA is effective in improving knee function and pain relief relative to baseline values. The combined treatment showed the greatest pain relief at 1-month follow-up.
References
Altman RD, Schemitsch E, Bedi A (2015) Assessment of clinical practice guideline methodology for the treatment of knee osteoarthritis with intra-articular hyaluronic acid. Semin Arthritis Rheum 45:132–139
Arden N, Nevitt MC (2006) Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol 20:3–25
Ayhan E, Kesmezacar H, Akgun I (2014) Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop 5:351–361
Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G (2006) Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev 2:CD005321
Bruyère O, Cooper C, Pelletier J-P, Branco J, Luisa Brandi M, Guillemin F, Hochberg MC, Kanis JA, Kvien TK, Martel-Pelletier J, Rizzoli R, Silverman S, Reginster J-Y (2014) An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally: a report from a task force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin Arthritis Rheum 44:253–263
Campbell KA, Erickson BJ, Saltzman BM, Mascarenhas R, Bach BR, Cole BJ, Verma NN (2015) Is local viscosupplementation injection clinically superior to other therapies in the treatment of osteoarthritis of the knee: a systematic review of overlapping meta-analyses. Arthroscopy 31(2036–2045):e14
Campbell KA, Saltzman BM, Mascarenhas R, Khair MM, Verma NN, Bach BR, Cole BJ (2015) Does intra-articular platelet-rich plasma injection provide clinically superior outcomes compared with other therapies in the treatment of knee osteoarthritis? A systematic review of overlapping meta-analyses. Arthroscopy 31:2213–2221
Chareancholvanich K, Pornrattanamaneewong C, Narkbunnam R (2014) Increased cartilage volume after injection of hyaluronic acid in osteoarthritis knee patients who underwent high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 22:1415–1423
Christensen R, Bartels EM, Astrup A, Bliddal H (2007) Effect of weight reduction in obese patients diagnosed with knee osteoarthritis: a systematic review and meta-analysis. Ann Rheum Dis 66:433–439
Colen S, van den Bekerom MPJ, Mulier M, Haverkamp D (2012) Hyaluronic acid in the treatment of knee osteoarthritis: a systematic review and meta-analysis with emphasis on the efficacy of different products. BioDrugs 26:257–268
Fernandes L, Hagen KB, Bijlsma JWJ, Andreassen O, Christensen P, Conaghan PG, Doherty M, Geenen R, Hammond A, Kjeken I, Lohmander LS, Lund H, Mallen CD, Nava T, Oliver S, Pavelka K, Pitsillidou I, da Silva JA, de la Torre J, Zanoli G, Vliet Vlieland TPM, European League Against Rheumatism (EULAR) (2013) EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 72:1125–1135
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL (2015) Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 1:CD004376
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, Towheed T, Welch V, Wells G, Tugwell P, American College of Rheumatology (2012) American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 64:465–474
Huang M-H, Yang R-C, Lee C-L, Chen T-W, Wang M-C (2005) Preliminary results of integrated therapy for patients with knee osteoarthritis. Arthritis Rheum 53:812–820
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin Orthop Relat Res 252:190–197
Jevsevar DS, Brown GA, Jones DL, Matzkin EG, Manner PA, Mooar P, Schousboe JT, Stovitz S, Sanders JO, Bozic KJ, Goldberg MJ, Martin WR, Cummins DS, Donnelly P, Woznica A, Gross L, AmericanAcademy of Orthopaedic Surgeons (2013) The American Academy of Orthopaedic Surgeons evidence-based guideline on: treatment of osteoarthritis of the knee, 2nd edition. J Bone Joint Surg Am 95:1885–1886
Jüni P, Hari R, Rutjes AWS, Fischer R, Silletta MG, Reichenbach S, da Costa BR (2015) Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 10:CD005328
Karatosun V, Unver B, Gocen Z, Sen A, Gunal I (2006) Intra-articular hyaluranic acid compared with progressive knee exercises in osteoarthritis of the knee: a prospective randomized trial with long-term follow-up. Rheumatol Int 26:277–284
Karlsson J, Sjögren LS, Lohmander LS (2002) Comparison of two hyaluronan drugs and placebo in patients with knee osteoarthritis. A controlled, randomized, double-blind, parallel-design multicentre study. Rheumatology (Oxford) 41:1240–1248
Kawasaki T, Kurosawa H, Ikeda H, Takazawa Y, Ishijima M, Kubota M, Kajihara H, Maruyama Y, Kim S-G, Kanazawa H (2009) Doi T Therapeutic home exercise versus intraarticular hyaluronate injection for osteoarthritis of the knee: 6-month prospective randomized open-labeled trial. J Orthop Sci 14:182–191
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Laudy ABM, Bakker EWP, Rekers M, Moen MH (2015) Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med 49:657–672
McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, Hawker GA, Henrotin Y, Hunter DJ, Kawaguchi H, Kwoh K, Lohmander S, Rannou F, Roos EM, Underwood M (2014) OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr Cartil 22:363–388
Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD (2015) Efficacy of intra-articular platelet-rich plasma injections in knee Osteoarthritis: a systematic review. Arthroscopy. doi:10.1016/j.arthro.2015.08.005
Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, Dragomir A, Kalsbeek WD, Luta G, Jordan JM (2008) Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 59:1207–1213
National Clinical Guideline Centre (UK) (2014) Osteoarthritis: care and management in adults. National Institute for Health and Care Excellence, London
Petrella RJ, Petrella M (2006) A prospective, randomized, double-blind, placebo controlled study to evaluate the efficacy of intraarticular hyaluronic acid for osteoarthritis of the knee. J Rheumatol 33:951–956
Rodriguez-Merchan EC (2013) Intraarticular injections of platelet-rich plasma (PRP) in the management of knee osteoarthritis. Arch Bone Jt Surg 1:5–8
Rothstein JM, Miller PJ, Roettger RF (1983) Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther 63:1611–1615
Rutjes AWS, Jüni P, da Costa BR, Trelle S, Nüesch E, Reichenbach S (2012) Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis. Ann Intern Med 157:180–191
Salaffi F, Leardini G, Canesi B, Mannoni A, Fioravanti A, Caporali R, Lapadula G, Punzi L, Gonorthrosis and Quality Of Life Assessment (GOQOLA) (2003) Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) osteoarthritis index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil 11:551–560
Schafer JL (1999) Multiple imputation: a primer. Stat Methods Med Res 8:3–15
Stemberger R, Kerschan-Schindl K (2013) Osteoarthritis: physical medicine and rehabilitation—nonpharmacological management. Wien Med Wochenschr 163:228–235
Stitik TP, Blacksin MF, Stiskal DM, Kim JH, Foye PM, Schoenherr L, Choi E-S, Chen B, Saunders HJ, Nadler SF (2007) Efficacy and safety of hyaluronan treatment in combination therapy with home exercise for knee osteoarthritis pain. Arch Phys Med Rehabil 88:135–141
Strand V, Baraf HSB, Lavin PT, Lim S, Hosokawa H (2012) A multicenter, randomized controlled trial comparing a single intra-articular injection of Gel-200, a new cross-linked formulation of hyaluronic acid, to phosphate buffered saline for treatment of osteoarthritis of the knee. Osteoarthr Cartil 20:350–356
Strand V, McIntyre LF, Beach WR, Miller LE, Block JE (2015) Safety and efficacy of US-approved viscosupplements for knee osteoarthritis: a systematic review and meta-analysis of randomized, saline-controlled trials. J Pain Res 8:217–228
Van der Weegen W, Wullems JA, Bos E, Noten H, van Drumpt RAM (2015) No difference between intra-articular injection of hyaluronic acid and placebo for mild to moderate knee osteoarthritis: a randomized, controlled double-blind trial. J Arthroplast 30:754–757
Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P (2007) OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthr Cartil 15:981–1000
Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P (2008) OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil 16:137–162
Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M, Hochberg M, Hunter DJ, Kwoh K, Lohmander LS, Tugwell P (2010) OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr Cartil 18:476–499
Author information
Authors and Affiliations
Corresponding author
Appendix: Rehabilitation protocols
Appendix: Rehabilitation protocols
-
Varus knee (medial tibio-femoral compartment)
-
Manual therapy;
-
Stretching of the following muscles: psoas, hip external rotators, medial flexors, biceps femoris and gastrocnemius;
-
Isometric exercises for quadriceps, biceps femoris and tensor fascia lata;
-
Isotonic exercises with elastic resistance (tubing) for quadriceps, biceps femoris and tensor fascia lata;
-
Proprioceptive rehabilitation.
-
-
Valgus knee (lateral tibio-femoral compartment)
-
Manual therapy;
-
Stretching of the following muscles: psoas, medial flexors, biceps femoris, tensor fascia lata and gastrocnemius;
-
Isometric exercises for quadriceps, hip adductors and medial flexors;
-
Isotonic exercises with elastic resistance (tubing) for quadriceps, hip adductors and medial flexors;
-
Proprioceptive rehabilitation.
-
-
Patello-femoral osteoarthritis
-
Manual therapy;
-
Stretching of the following muscles: psoas, hip external rotators, medial flexors, biceps femoris, tensor fascia lata and gastrocnemius;
-
Isometric exercises for quadriceps;
-
Isotonic exercises in closed kinetic chain for quadriceps with elastic resistance;
-
Proprioceptive rehabilitation.
-
Rights and permissions
About this article
Cite this article
Saccomanno, M.F., Donati, F., Careri, S. et al. Efficacy of intra-articular hyaluronic acid injections and exercise-based rehabilitation programme, administered as isolated or integrated therapeutic regimens for the treatment of knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 24, 1686–1694 (2016). https://doi.org/10.1007/s00167-015-3917-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3917-9