Abstract
Purpose
To quantify the dynamic balance deficits that characterise a group with chronic ankle instability compared to lateral ankle sprain copers and non-injured controls using kinematic and kinetic outcomes.
Methods
Forty-two participants with chronic ankle instability and twenty-eight lateral ankle sprain copers were initially recruited within 2 weeks of sustaining a first-time, acute lateral ankle sprain and required to attend our laboratory 1 year later to complete the current study protocol. An additional group of non-injured individuals were also recruited to act as a control group. All participants completed the anterior, posterior-lateral and posterior-medial reach directions of the star excursion balance test. Sagittal plane kinematics of the lower extremity and associated fractal dimension of the centre of pressure path were also acquired.
Results
Participants with chronic ankle instability displayed poorer performance in the anterior, posterior-medial and posterior-lateral reach directions compared with controls bilaterally, and in the posterior-lateral direction compared with lateral ankle sprain copers on their ‘involved’ limb only. These performance deficits in the posterior-lateral and posterior-medial directions were associated with reduced flexion and dorsiflexion displacements at the hip, knee and ankle at the point of maximum reach, and coincided with reduced complexity of the centre of pressure path.
Conclusion
In comparison with lateral ankle sprain copers and controls, participants with chronic ankle instability were characterised by dynamic balance deficits as measured using the SEBT. This was attested to reduced sagittal plane motions at the hip, knee and ankle joints, and reduced capacity of the stance limb to avail of its supporting base.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic ankle instability is an encompassing term used to classify an individual who presents with both mechanical and functional instability of the ankle joint following an initial lateral ankle sprain injury [5]. The manifestations of functional instability include impairments in sensorimotor control [27, 33], which have been previously quantified by means of static [18, 26, 35] and dynamic [28] balance tasks. The star excursion balance test (SEBT) is one of the most commonly utilised measures of dynamic balance in lateral ankle sprain populations, capably identifying those who are at an increased risk of sustaining an ankle sprain injury [4, 30], who have a current acute lateral ankle sprain injury [7], who are proceeding along the recovery trajectory of this injury [6], and who develop the chronic sequalae of chronic ankle instability [2, 13, 14, 16]. However, despite the tendency for a high proportion of individuals to develop chronic ankle instability following an acute lateral ankle sprain (up to 74 %) [1], some recover from this injury with no symptom progression. The existence of these individuals, who have been labelled lateral ankle sprain copers [34], has given rise to a hypothesis that recovery following lateral ankle sprain injury is dependent on the sensorimotor control strategies adopted post-injury [7, 9].
While lateral ankle sprain copers have previously been shown to display superior dynamic balance capacity as measured with the SEBT to individuals with chronic ankle instability and similar to that of non-injured individuals [2], the overall discriminatory ability of the SEBT’s clinically oriented outcome (reach distance) is poor relative to laboratory oriented outcomes such as the kinematics of the reach [2]. Indeed, no laboratory analysis is currently available which evaluates the reach distances and movement patterns employed to achieve these distances in individuals with chronic ankle instability compared with lateral ankle sprain copers and non-injured controls.
The current investigation is part of a larger longitudinal analysis whereby participants were prospectively followed after they sustained a first-time acute lateral ankle sprain injury in the determination of outcome (chronic ankle instability vs lateral ankle sprain coper). Data previously published on these individuals combined measures of platform stabilometry and lower extremity joint kinematics to evaluate the sensorimotor control underpinning SEBT performance in the anterior (ANT) posterior-lateral (PL) and posterior-medial (PM) reach directions compared with healthy controls [6, 7]. The current study pertains to data acquired from these participants 1 year after sustaining their injury, thus allowing them to be classified as having chronic ankle instability or being a lateral ankle sprain coper. The same kinematic and stabilometric measures were combined to compare task performance between these groups, in addition to a group of non-injured controls. It was hypothesised that individuals with chronic ankle instability would exhibit the same deficits in proximal joint sensorimotor control that were evident in the acute phase of injury (reduced hip and knee flexion displacements with reduced stance limb COP path complexity) in comparison with lateral ankle sprain copers and non-injured controls [6, 7].
Materials and methods
Seventy-one participants were recruited at convenience from a university-affiliated hospital Emergency Department within 2 weeks of sustaining a first-time acute lateral ankle sprain injury as part of the larger longitudinal analysis currently being conducted at our institution, and attended our laboratory 12 months after this recruitment to complete the protocol to which the current study pertains. An additional convenience group of twenty participants with no prior history of lateral ankle sprain were recruited from the hospital catchment area population using posters and flyers to act as a control group. All lateral ankle sprain participants were provided with standard guidance on applying ice and compression on discharge from the Emergency Department: they were encouraged to weight-bear and walk within the limits of pain. Activities of daily living were also encouraged. Whether participants sought additional formal medical healthcare services for council or rehabilitation of their lateral ankle sprain was documented on arrival to the testing laboratory but not controlled for as part of the current investigation.
The following exclusion criteria were utilised for all participants at the time of recruitment: (1) no previous history of ankle sprain injury on either limb (excluding the initial acute episode for the lateral ankle sprain groups); (2) no other severe lower extremity injury in the last 6 months; (3) no history of ankle fracture; (4) no previous history of major lower limb surgery and (5) no history of neurological disease, vestibular or visual disturbance or any other pathology that would impair their motor performance [8]. Lateral ankle sprain participants’ designation as chronic ankle instability or lateral ankle sprain coper status was completed according to recently published guidelines [10–12]. Self-reported ankle instability was confirmed with the Cumberland Ankle Instability Tool (CAIT) [10–12]; individuals with a score of <24 were designated as having chronic ankle instability, while lateral ankle sprain copers were designated with a score of ≥24, in the avoidance of potential false positives for this group [36]. Furthermore, to be designated as a lateral ankle sprain coper, participants must have reported to have returned to pre-injury levels of activity and function [34]. The activities of daily living and sports subscales of the Foot and Ankle Ability Measure (FAAMadl and FAAMsport) were utilised as a means to evaluate general self-reported foot and ankle function [10–12]. All participants completed the CAIT and subscales of the FAAM on arrival to the testing laboratory. Based on these criteria, twenty-eight individuals in the lateral ankle sprain group were designated as having chronic ankle instability, and forty-two as lateral ankle sprain copers; one lateral ankle sprain coper participant was excluded because he did not return to pre-injury levels of activity participation. Participant characteristics and questionnaire scores for these seventy individuals, in addition to the non-injured controls, are presented in Table 1.
All participants provided written informed consent, and the study was approved by the Human Research Ethics Committee of University College Dublin.
Protocol
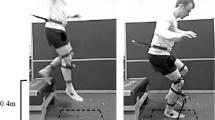
Collection methods for this study have been previously documented and were completed by one investigator (C.D) [6, 7]. Briefly, following completion of the questionnaires, each participant was instrumented with the Codamotion bilateral lower limb gait set-up (Charnwood Dynamics Ltd., Leicestershire, UK) and asked to perform specified reach directions of the SEBT [ANT; PL and PM], while standing on two adjacent force plates. Dynamic balance performance of both limbs was assessed. The SEBT was performed in line with the recommendations of Gribble et al. [15], and which has been previously described by Doherty et al. [6, 7]. The SEBT has been shown to have excellent intrarater and test–retest reliability [17, 30]. Pictorial representation of the experimental set-up is presented in Fig. 1. The onset and end of each trial were determined using a 10 N threshold of the vertical component of the ground reaction force data of the reaching (non-stance) limb. Reach distances were divided by limb length (measured from the anterior superior iliac spine to the ipsilateral medial malleolus) and multiplied by 100 to calculate a dependent variable that represents reach distance as a percentage of limb length [15].
Kinematic and stabilometric data were acquired for the stance limb during the three reach attempts using three Codamotion cx1 units (Charnwood Dynamics Ltd., Leicestershire, UK) and two AMTI (Watertown, MA) walkway embedded force plates, respectively. COP data acquired for the stance limb on the force plate during each SEBT reach attempt were used to compute the fractal dimension (FD) of the combined anterior-posterior (AP) and medial-lateral (ML) COP paths for that reach [24]. FD is a unit-less measure that describes the complexity of the COP signal [24], thus giving an indication of the extent to which the participant is utilising the available base of support [31]. Values range from 1 (low complexity or reduced capacity to avail of the supporting base) to 2 (high complexity) [24]. The AP and ML time series were passed through a fourth-order zero-phase Butterworth low-pass digital filter with a 5-Hz cut-off frequency.
For each participant, a mean of three successful trials in each reach direction was calculated for each dependent variable (reach distance, discrete sagittal plane lower extremity joint angular displacement values at the point of maximum reach and the FD of the COP path).
Statistical analysis
For both the chronic ankle instability and lateral ankle sprain coper groups, the limb to which the lateral ankle sprain was incurred at the time of recruitment was labelled as ‘involved’ and the non-injured limb as ‘uninvolved’. With regard to the control group, limbs were randomly assigned as ‘involved’ and ‘uninvolved’ in all cases and matched accordingly.
Reach distances
A separate two-way between-groups ANOVA was conducted to explore whether the chronic ankle instability group would demonstrate decreased reach distances for the ANT, PL and PM reach directions of the SEBT compared with the lateral ankle sprain coper and control groups. The independent variables were group (chronic ankle instability; lateral ankle sprain coper; control) and limb (involved and uninvolved). The dependent variable was reach distance. As the three reach directions of the SEBT were considered to represent separate tasks (ANT, PL, PM), the significance level for this analysis was not adjusted and set a priori at p < 0.05. Post hoc comparisons were completed using a Tukey HSD test where appropriate. The significance level for post hoc analyses was set at p < 0.05 for all reach directions.
Kinematics
Discrete joint angular displacement values were determined for the hip, knee and ankle joints in the sagittal plane of motion at the point of maximum reach for each reach direction and compared between chronic ankle instability, lateral ankle sprain coper and control groups. A two-way between-groups MANOVA model was adopted for each direction (ANT; PL; PM). The independent variables were group (chronic ankle instability; lateral ankle sprain coper; control) and limb (involved; uninvolved). The dependent variables were joint positions of the hip, knee and ankle in the sagittal plane. An alpha-level of p < 0.05 was used to determine significant differences for each analysis [21]. Post hoc comparisons were completed using a Tukey HSD test where appropriate. The significance level for post hoc analyses was set with a Bonferroni-adjusted alpha of p < 0.02 (0.05/3 joint positions) [23].
Kinetics (fractal dimension)
A two-way between-groups ANOVA was conducted separately for each SEBT reach direction. The independent variables were group and limb. The dependent variable was FD of the COP path. The significance level for this analysis was set a priori at p < 0.05. Post hoc comparisons were completed using a Tukey HSD test where appropriate. The significance level for post hoc analyses was set at p < 0.05 for all directions.
All statistical analyses were performed with IBM SPSS Statistics 20 (IBM Ireland Ltd., Dublin, Ireland).
Results
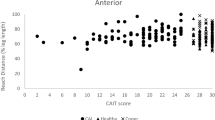
SEBT reach distance scores
There was a statistically significant main effect for group in the ANT, PL and PM directions. Post hoc analysis and inspection of the mean scores revealed that chronic ankle instability participants displayed poorer performance in the ANT direction compared with controls bilaterally (p < 0.01), in the PL direction compared with both lateral ankle sprain copers (p < 0.02; involved limb) and controls (p < 0.01; bilateral), and in the PM direction compared with controls only (p < 0.01; bilateral). Reach distance scores specific to limb and direction are presented in Table 2.
Kinematics
Regarding the kinematics of each reach attempt, there was a statistically significant main effect for group in the PL and PM reach directions. When the results of the dependent variables were considered separately, the knee (p < 0.01, η 2 p = 0.10) and ankle (p = 0.01, η 2 p = 0.55) joints were significant in the PL direction, and the hip (p < 0.01, η 2 p = 0.06) and knee (p < 0.01, η 2 p = 0.10) were significant in the PM direction. Post hoc analysis and inspection of the mean scores revealed that chronic ankle instability participants exhibited less knee flexion than both lateral ankle sprain copers (p < 0.01) and controls (p < 0.01), in addition to less ankle dorsiflexion than lateral ankle sprain copers (p = 0.04) and controls (p = 0.01), in the PL direction. These deficits were evident bilaterally, based on inspection of the group means. In the PM direction, chronic ankle instability participants exhibited less hip flexion than lateral ankle sprain copers on their involved limb (p < 0.01), and less knee flexion bilaterally than both controls (p < 0.01) and lateral ankle sprain copers (p < 0.01). Means and SDs for the kinematic dependent variables specific to limb and reach direction are presented in Table 3. Graphical representation of the kinematic group means for the ANT, PL and PM directions are presented in Fig. 2.
Kinematic ‘radar’ graph for denoting sagittal plane joint positions (°) for the hip, knee and ankle for the involved and uninvolved limbs of the CAI, LAS coper and control groups during performance of the anterior, posterior-lateral and posterior-medial reach directions. Flexion and dorsiflexion values are positive. Extension and plantar flexion values are negative. CAI = chronic ankle instability; LAS = lateral ankle sprain
Stabilometry
Regarding the kinetic variables of interest, there was a statistically significant main effect for group in the ANT, PL and PM directions. Post hoc analysis and inspection of the mean scores revealed that chronic ankle instability participants exhibited lower FD of the COP path trajectory on their involved limb compared with controls (p = 0.02) in the ANT direction. In the PL direction, chronic ankle instability participants displayed a bilateral reduction in the FD of the COP path compared with both lateral ankle sprain copers and controls (p < 0.01). Finally, in the PM reach direction, chronic ankle instability participants displayed significantly lower FD of the COP path on both limbs compared with controls only (p < 0.01). Means and SDs for the stabilometric dependent variables specific to limb and reach direction are presented in Table 4.
Discussion
The most important finding of the present study was that chronic ankle instability participants displayed poorer dynamic balance compared with both lateral ankle sprain copers and controls as determined by their reach distance scores during the SEBT. Interestingly, no differences were noted between lateral ankle sprain copers and controls. To the authors’ knowledge, this is the first documentation of a laboratory analysis of chronic ankle instability and lateral ankle sprain coper participants during the SEBT tested exactly 12 months after a first-time lateral ankle sprain injury.
One solitary analysis was previously conducted analysing SEBT reach distance performance in chronic ankle instability, lateral ankle sprain coper and control groups: a study by Plante et al. [29] revealed that only in the PM reach direction were deficits evident in the chronic ankle instability cohort. On the basis of this group’s findings, the PM direction seemed best suited in identifying dynamic balance deficits in participants with chronic ankle instability [29], a hypothesis which is reinforced in view of a number of laboratory analyses comparing chronic ankle instability groups to non-injured controls. The aforementioned analyses determined that the PM reach direction is most representative of overall SEBT performance [16] because it necessitates maximal amounts of hip and knee flexion in achieving superior reach distances [13, 14].
The above-mentioned findings were partially replicated in the current study, as the chronic ankle instability group did indeed exhibit significantly poorer performance in the PM reach direction compared with the control group, with a decrease in knee flexion displacement at the point of maximum reach. However, no differences were evident relative to lateral ankle sprain copers in terms of reach distance for this direction, despite the chronic ankle instability group displaying a significantly less flexed position of both the hip and knee.
A number of discrepancies do exist between our findings and those of previous studies, however. First, chronic ankle instability participants in the current study seemingly performed better than those in the studies we have alluded to. Taking the involved limb scores for the PM direction as an example, the chronic ankle instability group mean in the current investigation was 100.67 ± 7.97 %, a value substantially higher than that reported for the chronic ankle instability group in the study by Plante et al. (83.5 ± 6.5 %) [29], and those reported in previous studies, which have ranged from 85 to 92 % [16, 19, 22]. This may stem from the fact that the chronic ankle instability participants recruited for the current study, who were classified according to the recommendations of recently published guidelines [10–12], may be representative of a population early in the disease process; it is plausible that the chronic ankle instability paradigm worsens with time, whereby individuals with years of chronic ankle instability-associated disability are privy to time-dependent deteriorations in functional ability, as may have been the case in previously conducted studies [16, 19, 22, 29]; it is unlikely that an exact 1-year cut-off exists whereby the degenerative process of chronic ankle instability reaches relative stasis.
A second observation unique to this analysis is that chronic ankle instability participants seemingly displayed the most deficits in the PL direction compared with both lateral ankle sprain copers and controls. In fact, only in the PL reach direction did chronic ankle instability participants exhibit such differences, bilaterally, and in all the acquired parameters (performance, kinematic and stabilometric) compared with both lateral ankle sprain copers and controls. Specifically, chronic ankle instability participants displayed a reduction in the reach distance achieved on both their ‘involved’ and ‘uninvolved’ limbs. This coincided with less knee flexion and ankle dorsiflexion at the point of maximum reach, along with a reduced FD of the COP path. The constraints of the PL direction necessitate the utilisation of the trunk as a mobile counter-lever while the reaching limb moves in a ‘circular’ fashion. The potential result of this complex motion is a rotation torque about the ankle joint, a stimulus of potential difficulty for an individual with chronic ankle instability. While it has been established that the PM direction best encompasses the functional demands of the SEBT, and is the most sensitive to participants with chronic ankle instability, the study that made these assertions did not limit hand placement as part of SEBT task constraints [16], which is in contrast to the protocol used in this instance. That hand placement was not limited, which permits an additional motor control strategy (namely the use of the upper limb as a counter-lever) to compensate for the apparent increased difficulty of the rotatory movement. This may explain why in the current study, the PL direction was ‘most elucidative’ of performance deficits between all three groups, and not so in the others we have alluded to.
Despite these disparities with previous literature, a number of the observations in the current study were in agreement with the 2-week and 6-month analyses of these same lateral ankle sprain participants, prior to their stratification into chronic ankle instability and lateral ankle sprain coper groups: impairments in knee flexion displacement were evident both in the PL and PM reach directions [6, 7], as was the case in the current investigation, whereby chronic ankle instability participants exhibited less knee flexion than both lateral ankle sprain copers and controls for these components, in addition to ankle dorsiflexion. Furthermore, reduced complexity of the COP path, as determined using the FD calculation, has been a consistent theme of each analysis: lateral ankle sprain participants were shown to exhibit a lower FD of the COP path relative to controls [6, 7], as did chronic ankle instability participants relative to both lateral ankle sprain copers and controls in the current investigation. This has been evident in the PL direction in particular, where bilateral reductions have been noted at all time-points [6, 7]. This suggests that utilisation of the available base of support is implicit as part of achieving a better reach distance (particularly for the PL direction) and that an inability to do so may result in poorer outcome following lateral ankle sprain [8, 31].
While dorsiflexion range of motion has been shown to be an important contributor to the reach distance achieved in the ANT direction [20], no dorsiflexion restriction was evident in the kinematic data for this direction in the current study, despite an apparent performance impairment (in the chronic ankle instability group relative to controls). Therefore, the reason for the poorer performance achieved by the chronic ankle instability group in the ANT direction is not immediately apparent based on the current kinematic data. There are, however, a number of potential explanations for this. First, hip and knee flexion are corollaries of ankle dorsiflexion, and inadequacies of any one of these three may be masked by the ‘redirection’ of the motor apparatus. Such ‘redirection’ may be expressed in the form of a shift in the contribution of any one of these joints to the total ratio of flexion–dorsiflexion displacement of the lower extremity during task performance [3], and may be hidden during data aggregation. The lower FD displayed by chronic ankle instability participants relative to controls in the ANT direction may give some signal of this ‘redirection’ hypothesis, as this parameter identified poorer use of the available base of support by the former group, despite the absence of between-groups differences in kinematic data. Second, progressive ranges of sagittal plane hip and knee motion are never likely to develop without some degree of transverse and/or frontal plane motion. Thus, the movement required for any given reach is probably predicated by the flexion–dorsiflexion displacement of the lower extremity as a whole [32], and a conglomeration of highly variable 3D motion [3]. Chronic ankle instability participants may have ultimately performed poorer relative to controls, and this may be explained by the frontal and transverse plane movement patterns not acquired in this study.
The clinical implications of this study must be considered in light of the previously published findings in these groups. Deficits consistent across the current cohort of chronic ankle instability participants, and this cohort as a whole (chronic ankle instability and lateral ankle sprain coper) at the 2-week [7] and 6-month [6] time-points, were bilateral restrictions in flexion and dorsiflexion displacements. Clinicians should seek to tackle these deficits in the development of rehabilitation programmes. A recently published systematically conducted consensus statement [25] has advocated the implementation of balance and coordination training in the prevention of recurrence following lateral ankle sprain. Therefore, dynamic balance exercises such as the SEBT are likely to be beneficial and should be considered useful as part of training and rehabilitation programs. Limitations in the design of the current study mean that it is unknown as to whether the deficits exhibited by the chronic ankle instability group actually contributed to their outcome of having persistent functional insufficiency. Furthermore, because no data are available for these participants pre-injury, it is unknown whether these restrictions are central or peripherally sourced, or whether they preceded or occurred as a result of the injury. However, in comparing these individuals to lateral ankle sprain copers earlier in the recovery process, it was first elucidated that deficits manifested bilaterally and proximally, of which there was a continuation after 6 months. That the individuals with chronic ankle instability again displayed deficits bilaterally and proximally may implicate the subsidence in lateral ankle sprain copers of a centrally controlled movement impairment provoked by a distal injury constraint (of which there is a continuation in individuals with chronic ankle instability).
The research implications of this study are that our findings will likely inform our choice of variables in developing the prediction model designed to address the aforementioned issue as part of the longitudinal analysis this study developed in accordance with.
Conclusion
In conclusion, participants with chronic ankle instability who were tested 1 year after a first-time lateral ankle sprain exhibit bilateral and proximal deficits of sensorimotor control in an assessment of dynamic balance when compared with both lateral ankle sprain copers and controls. These deficits coincided with an alteration in the stance limb kinematical profile and COP behaviour during performance of the task.
References
Anandacoomarasamy A, Barnsley L (2005) Long term outcomes of inversion ankle injuries. Br J Sports Med 39:e14; discussion e14
Brown C, Bowser B, Orellana A (2010) Dynamic postural stability in females with chronic ankle instability. Med Sci Sports Exerc 42:2258–2263
Davids K, Glazier P, Araújo D, Bartlett R (2003) Movement systems as dynamical systems: the functional role of variability and its implications for sports medicine. Sports Med 33:245–260
de Noronha M, Franca LC, Haupenthal A, Nunes GS (2012) Intrinsic predictive factors for ankle sprain in active university students: a prospective study. Scand J Med Sci Sports 23:541–547
Delahunt E, Coughlan GF, Caulfield B, Nightingale EJ, Lin CW, Hiller CE (2010) Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med Sci Sports Exerc 42:2106–2121
Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E (2015) Dynamic balance deficits 6-months following first-time acute lateral ankle sprain: a laboratory analysis. J Orthop Sports Phys Ther 45: 626–633
Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E (2015) Laboratory measures of postural control during the star excursion balance test following acute ankle sprain. J Athl Train. doi:10.4085/1062-6050-50.1.09
Doherty C, Bleakley C, Hertel J, Caulfield B, Ryan J, Delahunt E (2014) Postural control strategies during single limb stance following acute lateral ankle sprain. Clin Biomech (Bristol Avon) 29:643–649
Glazier P, Davids K (2009) Constraints on the complete optimization of human motion. Sports Med 39:15–28
Gribble P, Delahunt E, Bleakley C, Caulfield B, Docherty C, Fourchet F et al (2013) Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the international ankle consortium. J Orthop Sports Phys Ther 43:585–591
Gribble PA, Delahunt E, Bleakley C, Caulfield B, Docherty C, Fourchet F et al (2014) Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the international ankle consortium. Br J Sports Med 48:1014–1018
Gribble PA, Delahunt E, Bleakley CM, Caulfield B, Docherty CL, Fong DTP et al (2014) Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the international ankle consortium. J Athl Train 49:121–127
Gribble PA, Hertel J, Denegar CR (2007) Chronic ankle instability and fatigue create proximal joint alterations during performance of the star excursion balance test. Int J Sports Med 28:236–242
Gribble PA, Hertel J, Denegar CR, Buckley WE (2004) The effects of fatigue and chronic ankle instability on dynamic postural control. J Athl Train 39:321–329
Gribble PA, Hertel J, Plisky P (2012) Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train 47:339–357
Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC (2006) Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther 36:131–137
Hertel J, Miller S, Denegar C (2000) Intratester and intertester reliability during the star excursion balance test. J Sport Rehabil 9:104–116
Hertel J, Olmsted-Kramer LC (2007) Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture 25:33–39
Hoch M, Staton G, Medina McKeon J, Mattacola C, McKeon P (2012) Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport 15:574–579
Hoch MC, Staton GS, McKeon PO (2011) Dorsiflexion range of motion significantly influences dynamic balance. J Sci Med Sport 14:90–92
Hopkins W, Marshall S, Batterham A, Hanin J (2009) Progressive statistics for studies in sports medicine and exercise science. Med Sci Sports Exerc 41:3–13
Hubbard TJ, Kramer LC, Denegar CR, Hertel J (2007) Contributing factors to chronic ankle instability. Foot Ankle Int 28:343–354
Huberty C, Morris J (1989) Multivariate analysis versus multiple univariate analyses. Psychol Bull 105:302–308
Katz MJ, George EB (1985) Fractals and the analysis of growth paths. Bull Math Biol 47:273–286
Kerkhoffs G, van den Bekerom M, Elders L, van Beek P, Hullegie W, Bloemers G et al (2012) Diagnosis, treatment and prevention of ankle sprains: an evidence-based clinical guideline. Br J Sports Med 46:854–860
McKeon PO, Hertel J (2008) Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord 9:76
Munn J, Sullivan S, Schneiders A (2010) Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport 13:2–12
Olmsted LC, Carcia CR, Hertel J, Shultz SJ (2002) Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability. J Athl Train 37:501–506
Plante J, Wikstrom E (2013) Differences in clinician-oriented outcomes among controls, copers, and chronic ankle instability groups. Phys Ther Sport 14:221–226
Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB (2006) Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther 36:911–919
Prieto T, Myklebust J, Hoffmann R, Lovett E, Myklebust B (1996) Measures of postural steadiness: differences between healthy young and elderly adults. IEEE Trans Biomed Eng 43:956–966
Robinson R, Gribble P (2008) Kinematic predictors of performance on the star excursion balance test. J Sport Rehabil 17:347–357
Sefton JM, Hicks-Little CA, Hubbard TJ, Clemens MG, Yengo CM, Koceja DM et al (2009) Sensorimotor function as a predictor of chronic ankle instability. Clin Biomech (Bristol Avon) 24:451–458
Wikstrom EA, Brown C (2014) Minimum reporting standards for copers in chronic ankle instability research. Sports Med 44:251–268
Wikstrom EA, Fournier KA, McKeon PO (2010) Postural control differs between those with and without chronic ankle instability. Gait Posture 32:82–86
Wright C, Arnold B, Ross S, Linens S (2014) Recalibration and validation of the cumberland ankle instability tool cutoff score for individuals with chronic ankle instability. Arch Phys Med Rehabil 95:1853–1859
Acknowledgments
This study was supported by the Health Research Board (HRA_POR/2011/46). There were no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doherty, C., Bleakley, C., Hertel, J. et al. Dynamic balance deficits in individuals with chronic ankle instability compared to ankle sprain copers 1 year after a first-time lateral ankle sprain injury. Knee Surg Sports Traumatol Arthrosc 24, 1086–1095 (2016). https://doi.org/10.1007/s00167-015-3744-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3744-z