Abstract
Purpose
To evaluate the influence of mild depression on pain perception after total knee arthroplasty (TKA).
Methods
Hamilton depression (HDRS) and numeric rating (NRS) scales were used to evaluate depression severity and pain perception at various intervals surrounding TKA. The Hospital for Special Surgery (HSS) knee and pain scores (NRS) in patients with signs of mild depression (HDRS < 20 points) were compared to a control group of patients with no signs of depression (HDRS < 8 points).
Results
Prior to surgery, there were no statistical differences in pain perception (NRS) or individual components of HSS knee score including range of motion, pain, and function between patients with mild depression compared to controls. However, following surgery, patients with signs of mild depression were more likely to report more pain (p < 0.001) and have lower HSS scores even at 1 year post-operatively (p < 0.001).
Conclusions
A significant number of patients in this series undergoing routine primary TKA had signs of subclinical depression. These patients are more likely to report increased pain even at 1 year following surgery compared to patients without signs of depression preoperatively. Psychometric evaluation prior to surgery can help identify the at-risk patient and allow for proper management of patient expectations, thus improving clinical results and patients’ satisfaction after TKA.
Level of evidence
Prospective comparative study, II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has been shown effective at relieving pain and improving function in patients with end-stage arthritis of the knee [4, 5, 10, 18, 23]. However, several studies have also shown that despite well-functioning knee prosthesis, up to 20 % of patients remain dissatisfied following surgery [3, 7, 8]. Residual pain and stiffness are among the leading causes of patient dissatisfaction following TKA [13, 22]. While mechanical or infectious causes of pain must be ruled out in patients with painful knees, there are a significant number of patients whose pain cannot be explained [21, 31]. Therefore, it is important to investigate patient factors or conditions that can contribute to pain following surgery.
In recent years, preoperative mental status, patient expectations, and ethnic and socio-economic factors have been recognized as important contributors to a patient’s final outcome following TKA [7]. Bonnin and Basiglini also identified 3 main factors influencing patient satisfaction following surgery which include: (1) functional outcome, (2) level of residual pain, and (3) preoperative expectations [7]. Additionally, Wylde and Dieppe [32] concluded that satisfaction correlated strongly with a patient’s ability to perform social functions and mental health. Finally, socio-demographic, medical, psychosocial, and other biological factors (i.e. female gender, low socio-economic status) have also been identified as possible risk factors for unexplained pain following TKA [15].
Depressive symptoms are commonly found in patients with musculoskeletal complaints [16]. While some studies have shown that depression and anxiety can negatively influence clinical outcomes following primary TKA [1, 28, 30], but others have shown no significant impact [6, 24]. Furthermore, because anxiety and depressive symptoms have also been shown to affect a patient’s perception of pain [26], understanding the impact of psychological comorbidities on clinical outcomes is equally as important as knowing the effects of physical comorbidities such as diabetes, obesity, and liver dysfunction on TKA results.
The psychological factors and their contributions to patient satisfaction following TKA remain unknown. Studies have shown that psychological factors can influence clinical outcomes in TKA [20]. Physical impairments associated with hip and knee joint arthritis can also have psychological and emotional effects in patients. However, while several authors have evaluated the impact of clinical depression on TJA outcomes, to our knowledge, there has not been a published report looking at the prevalence and effects of subclinical depression in patients undergoing TKA. Understanding of the impact of a patient’s preoperative psyche on outcome measures such as pain perception and knee society scores is important to improving patient selection, education, and counselling to maximize patient satisfaction following TKA. Therefore, preoperative psychometric testing to identify these patients for proper counselling is equally as important as testing and optimization of physical comorbidities to minimize complications and dissatisfaction following TKA.
Consequently, the purpose of this study is to determine (1) the prevalence of mild depression in patients undergoing TKA and evaluate the effect of mild depression on (2) pain perception and (3) the HSS knee scores during the first 12 months following primary TKA.
Materials and methods
This prospective, observational investigation was presented to all patients undergoing primary TKA between 2010 and 2011 at our institution. To be eligible, a patient needed to meet the following criteria: (1) undergoing unilateral primary TKA for arthritis, (2) no known history of mental impairments such as cognitive diseases or depression, (3) no physical comorbidities such as morbid obesity, diabetes, inflammatory diseases, lymphedema, or immunosuppression, and (4) ability to understand and participate in the perioperative evaluation programme. Patients with rheumatic diseases and those with valgus preoperative deformity were excluded. These patients were excluded from the study because they might perceive and rate pain differently compared to patients with varus alignment and osteoarthritis. Finally, patients were excluded from the final analysis if they developed any post-operative complications (i.e. wound complications, deep venous thrombosis, or infection).
Preoperatively, the presence or absence of depression was evaluated using the Hamilton depression rating scale (HDRS), and a patient’s pain level rated using a numeric rating scale (NRS). The HDRS is a validated questionnaire to evaluate the presence of depression in which a score of 0–7 points is normal and a score of greater than 20 points indicates the presence of severe depression [17]. This validated questionnaire was designed for adults to rate the severity of their depression by probing mood, feelings of guilt, suicidal ideation, insomnia, agitation or retardation, anxiety, weight loss, and somatic symptoms. This simple and reliable tool, which should not be used for the diagnosis of clinical depression, was incorporated in the study design following consultation with a psychology to determine its appropriate use and relevance. For this study, a patient was considered to have signs of mild depression if he/she scored 8–19 points on the HDRS (Group D), while patients with HDRS scores less than 8 points were considered nondepressed (Group ND). All patients underwent TKA using a standardized surgical technique with the same posterior cruciate sacrificing knee implant (Nexgen, Zimmer. Warsaw, IN). Post-operatively, all patients were subjected to the same, standardized post-operative rehabilitation protocol. Clinical outcomes (Hospital for Special Surgery (HSS) knee scoring system), pain perception (NRS), and psychometric evaluations (HDRS) were prospectively collected at standardized intervals (preoperatively (T0), three months (T1), 6 months (T2), and 12 months (T3). The results of patients with depressive symptoms (Group D) were compared to patients without signs of depression prior to TKA (Group ND).
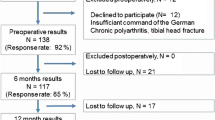
Out of 260 primary TKAs performed during this time period, a total of 67 patients met the above criteria, enrolled, and were included in the final analysis. One hundred and three patients refused to participate, and 23 patients were lost to follow-up. Other excluded included 10 patients with diabetes, post-operative infection (n = 1), rheumatoid arthritis (n = 12), other comorbidities (n = 8), prior contralateral TKA (n = 22), and 14 patients who could not understand or complete the questionnaires. There were 17 men and 50 women with a median age of 72 (range 47–83). During the study period, 1 patient from Group ND was dropped from the final analysis secondary to the development of a deep-vein thrombosis.
All patients gave informed consent prior to their inclusion in the study, which has been performed in accordance with the ethical standards as certified by the protocol 0044131/S from the Institution Città della Salute e della Scienza di Torino.
Statistical analysis
A priori power analysis of the data with repeated measures was performed. Assuming an average group difference of 2 points over time on the pain NRS scores to be clinically significant, a study with a sample size of 20 patients would yield a power of 83 % at the 0.05 alpha level.
Continuous variables were expressed as median and interquartile range and compared using a Mann–Whitney U test. Categorical variables were expressed as counts and percentages and analysed using the Chi-square test. Time effects were compared between the study and control groups. A generalized least-square regression model was performed to ascertain whether a significant interaction occurred between the two groups and time from surgery. Additionally, a correlation structure was specified to account for repeated measures over time.
A correlation structure was specified to account for the non-independent observations on the same subject over time. A continuous-time autoregressive of order 1 (CAR1) correlation structure was found to yield the best model fit according to the Akaike Information Criterion (AIC). Age and sex were then entered into this model and their effects tested using the Wald test. Restricted cubic splines were used to deal with the nonlinear NRS scores over time. The data were analysed using R version 2.15. A p value below 0.05 was considered significant.
HDRS questionnaire contains 21 items, and the scoring is based on the first 17, which is pertaining to symptoms of depression experienced in the previous week. Each question has between 3 and 5 possible responses on a Likert scale, which increases in severity. In particular, eight items are scored on a 5-point scale, ranging from 0 (symptom not present) to 4 (severe symptom), and nine are scored from 0 to 2. Cronbach’s alpha statistic, which is used to evaluate internal reliability, was estimated ≥0.70 reflect adequate reliability. Retest reliability, which assesses the extent to which more than one administrations generate the same results, ranges from 0.81 to 0.98, whereas retest reliability at the item level ranges from 0.00 to 0.85 [2].
NRS scale is a unidimensional measure of pain intensity in which respondents select an integer number (from 0 to 10) that best reflects the intensity of their pain. For construct validity, the NRS was shown to be highly correlated with the visual analogue score in patients with rheumatic and other chronic pain conditions (correlations range from 0.86 to 0.95) with test–retest reliability coefficient above 0.9 [14].
Results
In this group of patients undergoing unilateral primary TKA, there was a significant number of patients who unknowingly had signs and symptoms of depression. Using the HDRS as a screening tool, 23 patients (34 %) had symptoms consistent with mild depression and comprised the study group (Group D). The remaining 44 patients (66 %) had HDRS scores less than 8 points and comprised the control group (Group ND). The two groups were similar in terms of patient demographics and patient characteristics (Table 1). During the first 12 months following TKA, there were no significant changes in HDRS compared to preoperatively (Fig. 1). Two patients refused to complete the study (one from each group).
The presence of signs of depression prior to surgery was associated with higher levels of patient-reported pain (NRS) following TKA. Patients who had depressive symptoms prior to TKA (HDRS > 8 points) were more likely to have more pain at 3, 6, and 12 months compared to patients with low HDRS (Table 2). Preoperatively, there was no difference in the NRS score between the two groups (n.s.), and although both groups showed improvements following surgery, patients in Group D had significantly higher NRS pain scores compared to patients in Group ND at all the standardized post-operative intervals (p < 0.001) (Fig. 2). When considering the effects of time, age, depression, and sex on NRS scores, only time from surgery and depression correlated with a patient’s perception of pain.
Trend of numeric rating scale (NRS) score for pain over time as predicted by the generalized least-square model stratified by group of patients and adjusted by age, sex, and NRS score at baseline. Grey areas represent 95 % confidence interval bands. Dotted line moderate depressed patients (Group D); continuous line absent depression patients (Group ND)
Patients exhibiting signs and symptoms of depression have lower knee scores compared to nondepressed patients even up to 1 year following TKA. Prior to surgery, the median HSS knee score was 76.5 points (IQR 68.8–86) in Group ND compared to 65 points (IQR 57.5–77) in the Group D (p = 0.02). While similar improvements were seen following TKA, at 12 months, the median HSS knee score was 94 (IQR 88.7–96) in Group ND and 85 (IQR 79.5–92.5) in Group D, respectively (p < 0.001). There was no difference in the delta between the two groups (n.s.). Analysis of the potential contributing factors for these differences showed that the pain, ability to walk, and stair-climbing components of the HHS knee score were among the main factors contributing to this disparity (Table 2).
Discussion
The most important finding of this study is the direct correlation between depressive symptoms at a subclinical level (HDRS between 8 and 19 points) prior to TKA and higher levels of patient-reported pain (NRS) at all intervals up to 12 months post-operatively. Additionally, a significant number of patients in this group (33 %) undergoing TKA can exhibit signs and symptoms of depression without a prior diagnosis of the psychological condition. This prevalence is consistent with other previously published reports. Perez-Prieto et al. [24] reported that in a cohort of 716 patients undergoing TKA, 200 (28 %) patients had depression. However, these findings on the influence depression on TKA are also different from other prior published studies. While Duivenvoorden et al. [11] reported improvements in depressive symptoms following THA/TKA, in this study, the patient’s HDRS score remained relatively constant throughout the first year following arthroplasty. This suggests that the symptoms of depression may not be affected by knee replacement. A potential explanation is that these authors used another psychometric tool (Hospital Anxiety and Depression Scale) to quantify severity of depression compared to the HDRS. This illustrates the complexity of quantifying psychological conditions but also emphasizes the ability of a patient’s psyche to change and influence clinical rating scores following surgery. Consequently, a HDRS is an easy-to-use psychometric screening tool to determine the presence of signs and symptoms of depression prior to TKA. Patients with high HDRS scores should be counselled for the possibility of residual pain following primary TKA. This study also highlights the influence of mental well-being on the somatic manifestation of pain. The results show that patients with HDRS scores greater than 8 points were more likely to report higher NRS scores even at 1 year following TKA compared to controls. Riddle et al. [26] used the Patient Health Questionnaire 8 and concluded that there was an association between depression, pain, and function. Another study using the pain catastrophizing scale found that pain was the only consistent psychological predictor of poor outcome [27]. Additionally, Edwards et al. [12] suggested that catastrophizing and depression promoted enhanced levels of night-time pain and daily pain, respectively. Therefore, consistent with prior published reports, patients with depression and anxiety can affect a patient’s perception and characterization of pain.
In this study, patients with preoperative symptoms of depression had lower preoperative HSS knee scores and also lower HSS knee scores at 12 months compared to controls. Analysis of the individual components that comprise this score revealed that pain, walking distance, and stair-climbing components were consistently lower in the study group (Group D). Interestingly, both groups had similar improvements (i.e. delta) following TKA. These results are also consistent with previously published reports. Hirschmann et al. [19] reported lower KSS scores in depressed patients prior and after TKA. Similarly, Perez-Prieto et al. [24] showed that while depressed patients had lower post-operative scores compared to nondepressed patients, their 1-year improvement was similar if not better compared to controls. Finally, Utrillas-Compaired et al. [30] reported that the presence of preoperative psychological distress did not preclude patients from achieving pain relief but was associated with poorer function and quality of life after TKA. Thus, while patients with depression can benefit from TKA, they can be at risk for residual pain. These results also demonstrate that the presence of depressive symptoms without formal clinical diagnosis of depression is sufficient to affect a patient’s perception of pain and clinical ratings even at 1 year post-operatively. Therefore, preoperative psychometric testing to identify these patients for proper counselling is equally as important as testing and optimization of physical comorbidities to minimize complications and dissatisfaction following TKA.
Symptoms of depression can commonly be found in patients presenting with musculoskeletal complaints [16]. A patient’s psychological well-being has been shown to affect a patient’s perception of pain and can, in turn, affect patient satisfaction following TKA [25]. With several authors reporting inferior results of TKA in patients with depression [9, 12], it is therefore important to identify the causes of dissatisfaction in this patient population (Table 3). A question to which this study cannot provide an answer to is whether or not preoperative intervention in patients with depressive symptoms or clinical depression can ultimately affect subsequent clinical perception of pain and outcome. Future prospective, randomized, multicentre studies will be necessary to determine which preoperative interventions (if any) can prepare and optimize a patient’s psyche for the process of TKA.
This study has several limitations. First, the sample size is relatively small, nonconsecutive, and highly selected, thus introducing the possibility of bias and type 1 error. However, the study was designed to eliminate confounding variables which could affect pain perception, and our power analysis showed our sample size to be sufficiently sensitive to detect small changes and therefore lessens the likelihood of error and allows for identification of certain trends. Second, while the HDRS is a validated screening tool for depression, it is not specific to determining the various subsets of anxiety and depressive disorders. As a result, care must be used when interpreting these data and generalizing these conclusions to all patients with depressive symptoms. Nevertheless, the HDRS can be used as a tool to allow the identification of the “at risk” patient for pain and potential dissatisfaction in order to allow for proper counselling and management of realistic expectations. Finally, the final psychometric and clinical evaluations for this cohort of patients were performed at 12 months following TKA, and thus, it is unclear whether future improvements were made beyond this point. Though studies have shown that HSS knee scores do not significantly change beyond 1 year [4], some have reported functional improvements up to 24 months following primary TKA [29]. Consequently, larger, longer term, prospective studies with more specific psychometric tests are needed to define this complex patient variable.
Conclusions
This study shows that mild depressive symptoms without a clinical diagnosis of depression prior to surgery can influence post-operative pain perception (higher NRS scores) even 1 year following surgery. This work is clinically relevant in daily practice because proper patient selection and appropriate management of patient expectations prior to total knee arthroplasty is critical to maximizing patient satisfaction. Therefore, addition of psychometric tests to traditional physical examination can provide a more complete patient profile and will help identify and counsel patients at risk of dissatisfaction following surgery.
References
Ali A, Sundberg M, Robertsson O, Dahlberg LE, Thorstensson CA, Redlund-Johnell I et al (2014) Dissatisfied patients after total knee arthroplasty. Acta Orthop 85(3):229–233
Bagby RM, Ryder AG, Schuller DR, Marshall MB (2004) The Hamilton depression rating scale: has the gold standard become a lead weight? Am J Psychiatry 161(12):2163–2177
Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P (2012) What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open 2:e000435
Bistolfi A, Lee GC, Deledda D, Rosso F, Berchialla P, Crova M, Massazza G (2014) NexGen® LPS mobile bearing total knee arthroplasty: 10-year results. Knee Surg Sports Traumatol Arthrosc 22(8):1786–1792
Bistolfi A, Massazza G, Rosso F, Deledda D, Gaito V, Lagalla F et al (2011) Cemented fixed-bearing PFC total knee arthroplasty: survival and failure analysis at 12–17 years. J Orthop Traumatol 12(3):131–136
Blackburn J, Qureshi A, Amirfeyz R, Bannister G (2012) Does preoperative anxiety and depression predict satisfaction after total knee replacement? Knee 19(5):522–524
Bonnin MP, Basiglini L (2011) What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc 19:1411–1417
Bourne RB, Chesworth BM, Davis A, Mahomed N, Charron K (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Brander V, Gondek S, Martin E, Stulberg D (2007) Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res 464:21–26
Buechel FF Sr (2002) Long-term follow up after mobile-bearing total knee replacement. Clin Orthop Relat Res 404:40–50
Duivenvoorden T, Vissers MM, Verhaar JA, Busschbach JJ, Gosens T, Bloem RM et al (2013) Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage 21(12):1834–1840
Edwards RR, Hayhornthwaite JA, Smith MT, Klick B, Katz JN (2009) Catastrophizing and depressive symptoms as prospective predictors of outcomes following total knee replacement. Pain Res Manage 14:307–311
Escobar A, Quintana JM, Bilbao A, Aróstegui I, Lafuente I, Vidaurreta I (2007) Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage 15:273–280
Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH (1990) Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol 17:1022–1024
Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D et al (1999) Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum 42:1722–1728
Gerber PD, Barrett JE, Barrett JA, Oxman TE, Manheimer E, Smith R et al (1992) The relationship of presenting physical complaints to depressive symptoms in primary care patients. J Gen Intern Med 7(2):170–173
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23(1):56–62
Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R et al (1998) Health-related quality of life after knee replacement. J Bone Joint Surg Am 80-A:163–173
Hirschmann MT, Testa E, Amsler F, Friederich NF (2013) The unhappy total knee arthroplasty (TKA) patient: higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc 21(10):2405–2411
Khatib Y, Madan A, Naylor JM, Harris IA (2015) Do psychological factors predict poor outcome in patients undergoing TKA? A systematic review. Clin Orthop Relat Res. doi:10.1007/s11999-015-4234-9
Mont MA, Serna FK, Krackow KA, Hungerford DS (1996) Exploration of radiographically normal total knee replacements for unexplained pain. Clin Orthop Relat Res 331:216–220
Murray DW, Frost SJ (1998) Pain in the assessment of total knee replacement. J Bone Joint Surg Br 80B:426–431
Parsch D, Krüger M, Moser MT, Geiger F (2009) Follow-up of 11–16 years after modular fixed-bearing TKA. Int Orthop 33(2):431–435
Pérez-Prieto D, Gil-González S, Pelfort X, Leal-Blanquet J, Puig-Verdié L, Hinarejos P (2014) Influence of depression on total knee arthroplasty outcomes. J Arthroplasty 29(1):44–47
Pressman SD, Cohen S (2005) Does positive affect influence health? Psychol Bull 131(6):925–971
Riddle DL, Wade JB, Jiranek WA (2010) Major depression, generalized anxiety disorder and panic disorder in patient scheduled for knee arthroplasty. J Arthroplasty 25(4):581–588
Riddle DL, Wade JB, Jiranek WA, Kong X (2010) Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res 468:798–806
Singh JA, Lewallen DG (2014) Depression in primary TKA and higher medical comorbidities in revision TKA are associated with suboptimal subjective improvement in knee function. BMC Musculoskelet Disord 11(15):127
Singh JA, Lewallen DG (2014) Patient level improvements in pain and activities of daily living after total knee arthroplasty. Rheumatology 53(2):313–320
Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martínez AJ, Asúnsolo-Del Barco Á (2014) Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res 472(8):2457–2465
Vince KG (2003) Why knees fail. J Arthroplasty 18(3 Suppl 1):39–44
Wylde V, Dieppe P, Hewlett S, Learmonth ID (2007) Total knee replacement: is it an effective procedure for all? Knee 14:417–423
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bistolfi, A., Bettoni, E., Aprato, A. et al. The presence and influence of mild depressive symptoms on post-operative pain perception following primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 2792–2800 (2017). https://doi.org/10.1007/s00167-015-3737-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3737-y