Abstract
Purpose
The aim of this study was to assess the reliability of preoperative MRI for the staging of osteochondritis dissecans (OCD) lesions of the knee and the talus in juvenile patients, using arthroscopy as the gold standard of diagnosis.
Methods
Sixty-three juvenile patients (range 8–16 years) with an OCD of the knee or the talus underwent arthroscopy after MRI. In 54/9 out of 63 cases, 1.5/3 T MR scanners were used. The OCD stage was classified according the staging criteria of Dipaola et al. Arthroscopic findings were compared with MRI reports in each patient.
Results
From the 63 juvenile patients, MRI/arthroscopy revealed a stage I OCD in 4/19 patients, stage II in 31/22 patients, stage III in 22/9 patients and stage IV in 6/6 patients. No osteochondral pathology was evident in arthroscopy in seven out of 63 patients. The overall accuracy of preoperative MRI in staging an OCD lesion of the knee or the talus was 41.3 %. In 33 out of 63 patients (52.4 %), arthroscopy revealed a lower OCD stage than in the preoperative MRI grading, and in four out of 63 cases (6.4 %), the intraoperative arthroscopic grading was worse than in preoperative MRI prior to surgery. The utilization of the 3 T MRI provided a correct diagnosis with 44.4 %.
Conclusions
Even with today’s modern MRI scanners, it is not possible to predict an accurate OCD stage in children. The children’s orthopaedist should not solely rely on the MRI when it comes to the decision to further conservative or surgical treatment of a juvenile OCD, but rather should take surgical therapy in consideration within persisting symptoms despite a low OCD stage provided by MRI.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The pathogenesis and aetiology of osteochondritis dissecans (OCD) still remain unclear [11]. It can be assumed that repetitive microtraumata may interrupt the already decreased epiphyseal blood flow during child growth and therefore contribute to the development of an OCD [21]. To identify and diagnose an OCD, magnetic resonance imaging (MRI) is preferred for diagnosis [8] as well as for monitoring the progression and/or the healing of the OCD [19]. In particular, MRI is able to evaluate the articular cartilage that covers the osteochondral lesion with a high quality, and it helps to identify patients who would benefit from an arthroscopic treatment [15]. Adults with a stage II OCD or above according to Dipaola et al. [4] mainly receive operative treatment [22]. In contrast to adults, the juvenile OCD (male ≤ 13 years and female ≤ 11 years) will be treated conservatively, even in stage II OCD, rather than surgically. Literature shows that the juvenile OCD has a better prognosis than the adult OCD, with a higher rate of spontaneous healing under conservative therapy [16]. The juvenile OCD is typically stable, and the findings in patients with an intact articular surface have a good potential to heal with conservative treatment in terms of adjustment of the repetitive impact forces [9]. Surgical treatment of juvenile OCD is generally indicated in cases of failure of conservative therapy, in unstable OCD and in findings that are temporally close to the closing of the epiphyseal plate [22]. However, clinical experience shows that in stage I or II OCD according to Dipaola et al. [4], there are several cases that show persistency of pain despite conservative therapy over 6 months. In our department, children with resistance to the conservative therapy after 6 months despite Dipaola stage I or II OCD undergo an arthroscopy of the affected joint to re-evaluate the lesion and eventually perform an invasive therapy if necessary. The question arises if the OCD stages in preoperative MRI in juvenile patients correspond to those in arthroscopy. This is based on the knowledge that the MRI criteria even for an unstable OCD have a high specificity for adults, but not for the juvenile patients [10].
The aim of this study was to assess the reliability of preoperative MRI for staging OCD lesions of the knee and the talus in juvenile patients, using arthroscopy as the gold standard of diagnosis. It can be hypothesized that even with today’s modern MRI scanners, it is not possible to predict an accurate OCD stage in children.
Materials and methods
In a retrospective case series, 63 juvenile patients with an OCD of the knee or the talus underwent arthroscopy in our Department of Orthopaedic Surgery, Physical Medicine and Rehabilitation, University Hospital of Munich (LMU), Campus Grosshadern. Exclusion criteria were the patient age ≥17 years, prior surgery and post-traumatic OCD. The average age of the 63 juvenile patients was 12 years (range 8–16 years). All patients were skeletally immature. The sex ratio was 37 females to 26 males. There was no preference of the affected extremity (33 right legs vs. 30 left legs). All patients had clinical examination at index presentation, plain radiographs and MRI. If Dipaola stage III or IV OCD [4] was found, arthroscopy was performed within the next 2 weeks. If Dipaola stage I or II OCD [4] was revealed, a 6-month period of conservative therapy (pain medication if required, interruption of sports activities, in accordance with Lefort et al. [13]) was utilized. Afterwards, the patients underwent a second follow-up MRI investigation. If Dipaola stage I or II OCD [4] and clinical symptoms persisted, the patients were then admitted to arthroscopy. All patients either received arthroscopic retrograde drilling of OCD or, depending on the extent of a greater damage, a loose body refixation, microfracturing, osteochondral autograft transfer system (OATS) or matrix-induced autologous chondrocyte implantation (MACI). In all cases, a closed MR scanner was used. In 54 cases, MR scanner with a magnetic field strength of 1.5 T was utilized, and in nine patients a 3 T MR scanner was utilized. All MRIs have been assessed by an orthopaedic surgeon and a radiologist with musculoskeletal expertise. Standard imaging sequences included a sagittal and coronal T1-weighted sequence and proton-density turbo spin-echo fat-suppressed (PD-fs) sequences in sagittal, axial and coronal planes. The surgeon assessing the preoperative MRI was the same surgeon who performed the arthroscopy. The preoperative MRI reports were known to the surgeon before surgery.
Classification of MRI and arthroscopic findings
In 1991, Dipaola et al. compared the MRI results of OCD lesions with arthroscopic findings based on the classification that were given by Guhl [5]. For that reason, the OCD classification system of Dipaola et al. [4] was used for the comparison of MRI and arthroscopy. Arthroscopic findings were compared with those of the preoperative MR imaging in each patient after surgery. The study was approved by the ethics committee of the Medical Faculty of the University Hospital of Munich (LMU) in January 2013.
Statistical analysis
The descriptive analyses of the results, including accuracy, overestimation and underestimation of preoperative MRI in comparison with arthroscopic findings, were expressed as a percentage (%). The diagnostic accuracy of preoperative MRI in diagnosing OCD lesions was secured together by an orthopaedic surgeon and a radiologist with musculoskeletal expertise, as mentioned before. Figures were created with Windows Microsoft Excel® 2013 (Microsoft Corporation, Redmond, USA).
Results
In 63 juvenile patients, OCD lesions were found in the following locations: medial femoral condyle (n = 36), lateral femoral condyle (n = 6), retropatellar (n = 4), medial talus (n = 16) and lateral talus (n = 1). The number of patients for each OCD stage in MRI and arthroscopy is shown in Fig. 1. Each OCD stage in MRI was compared with real OCD stage found in arthroscopy (see Fig. 2).
Number of patients for each OCD stage according to Dipaola et al. [4] in MRI and arthroscopy
Number of patients for each single OCD stage according to Dipaola et al. [4] in MRI compared to arthroscopic findings (ASC)
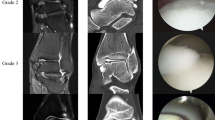
In total, a consistent diagnosis was made in 26 out of 63 cases (41.3 %) by preoperative MRI and intraoperative findings (see Fig. 3). In 13 out of 63 patients (20.6 %), an overestimation of two OCD stages was discovered. For example, in an 8-year-old girl with stage III OCD in preoperative 1.5 T MRI in the right medial femoral condyle, stage I OCD was found in arthroscopy (see Fig. 4).
Eight-year-old girl with stage III OCD according to Dipaola et al. [4] in preoperative 1.5 T MRI (coronal PD-fs and sagittal T1) in right medial femoral condyle (a, b) and stage I OCD in arthroscopy (c)
In total, actual findings have been underestimated in four out of 63 cases (6.4 %). One case was a 13-year-old girl with a retropatellar stage I OCD in MRI in the right knee while a stage III OCD defect revealed in arthroscopy which was fixated in open surgery. A second case was a 14-year-old boy with a stage I OCD in MRI in the right medial femoral condyle, showed a stage III OCD in arthroscopy and underwent microfracturing of the cartilage damage. In another case, a 12-year-old girl with stage II OCD in MRI in the right medial talus showed stage III OCD in arthroscopy and received microfracturing of the cartilage damage as well. In the fourth and final case, a 15-year-old boy with stage III OCD in MRI in the right medial femoral condyle was diagnosed stage IV OCD during arthroscopy and received MACI.
Analysis of the results depending on stage of OCD and localization
Results for juvenile patients with knee OCD
The assessment of femoral OCD patients (n = 42/63) mainly showed stage II (n = 18) or stage III (n = 16) OCD. Arthroscopy verified predominantly stage I (n = 14) and II (n = 13) OCD. Preoperative MRI and arthroscopy correlated in 59.6 % of all patients with an OCD of the femoral condyle.
Four out of 63 patients (6.4 %) were diagnosed with retropatellar OCD. Three out of four cases were diagnosed correctly (75 % congruence with MRI findings) (see Fig. 5).
Assessment of OCD stage according to Dipaola et al. [4] in MRI compared to arthroscopy (ASC) for retropatellar OCD
Results for patients with talus OCD
The analysis of the juvenile patients with an OCD of the talus (n = 17/63), preoperative MRI showed stage II OCD in 12 out of 17 patients and stage III OCD in five out of 17 cases. Arthroscopy revealed stage I OCD in five patients, stage II OCD in eight patients and stage III OCD in three patients. No osteochondral pathology was seen in one case during arthroscopy. In the case of a 12-year-old boy with stage II OCD in the right medial talus and who was admitted to arthroscopic surgery due to persisting of clinical symptoms, a stage III OCD was found intraoperatively (see Fig. 6). In total, MRI and arthroscopic findings of patients suffering from an OCD of the talus correlated in 64.7 % of the cases.
Twelve-year-old boy with stage II OCD according to Dipaola et al. [4] in preoperative 3 T MRI (coronal and sagittal PD-fs) in right medial talus (a, b) and stage III OCD in arthroscopy (c)
Analysis of the results of juvenile patients with 3 T MRI
Four juvenile male patients (aged 11–15 years) and five female patients (aged 12–16 years) were preoperatively diagnosed with 3 T MRI. From these nine patients, out of a total of 63, only four (44.4 %) preoperative cases correlated with arthroscopy. OCD staging was too low in four other patients (44.4 %), which underwent 3 T MRI scans. One child was assessed preoperatively too high by the 3 T MRI.
Discussion
The most important finding of the present study was that the preoperative accuracy of preoperative MRI in staging an OCD lesion of the knee or the talus in juvenile patients is not good enough to correctly diagnose the OCD stage. Using the arthroscopic staging as the gold standard of diagnosis, we found that the overall accuracy of MRI only was 41.3 %. In 33 out of 63 patients (52.4 %), the OCD stage was lower in arthroscopy than in preoperative MRI grading. In 2011, Heywood et al. [7] found similar results. In a study of 23 juvenile patients with a mean age of 12.9 years, they were able to show that with preoperative MRI, OCD was considered unstable in 21 out of 23 patients, but in arthroscopic staging, only 10 out of the 23 OCD lesions were found to be unstable. In their study, in 11 out of 21 cases, that means also 52.4 %, an overestimation of the MRI grading was present. However, their statistical results were calculated with the intention of detection stable or unstable OCD lesions rather than analysing the single stages.
This study shows that the OCD lesion was worse in four out of 63 patients (6.4 %) than assumed in MRI prior to surgery. Surgical intervention was therefore absolutely necessary in all four juvenile patients.
Preoperative MRI, assessing an OCD of the talus and femoral condyle, showed a congruence of 64.7 and 59.5 % between MRI and arthroscopic findings, respectively. This raises the question whether a higher correspondence would have been generated by higher MRI resolution. The data of this study show that preoperative 3 T MRI examinations of juvenile patients (n = 9/63) show a consistent diagnosis with arthroscopy in 44.4 % of the cases.
The correct MRI interpretation in juvenile OCD, hence the recommendation for further conservative or surgical treatment, turns out to be very difficult. Kocher et al. [12] determined 22 juvenile patients in a consecutive study with an OCD of the knee with a mean age of 11.9 years. They stated that selective magnetic resonance imaging would not provide enhanced diagnostic utility over clinical diagnosis on the basis of history, physical examination and standard radiographs. Possibly computed tomography arthrography (CTA) can be considered as a further reasonable option in order to receive an even higher informative value than by MRI in children with an OCD and persisting pain despite conservative treatment. In the past, a few studies have been conducted with good results using CTA in OCD of the talus in adults [20]. Cahill and Berg discovered that a bone scintigraphy might be meaningful in the management of juvenile OCD due to its higher sensitivity to changes in lesion activity [2].
The optimal treatment of juvenile OCD still is discussed controversially [14]. In general, children are more likely to be treated conservatively than adults [18], and of course, conservative treatment should be the first-line treatment for stable OCD in children. The duration of conservative treatment should be at least 3–6 months prior to the decision for surgical treatment if a juvenile patient is truly asymptomatic or has only minor symptoms [16]. An important question arises, when to change to surgical treatment in juvenile patients if pain persists within conservative therapy. In a study conducted by Perumal et al. [17] with 31 juvenile patients with a mean age of 11.9 years and an OCD of the talus, the authors proclaimed that few juvenile OCD lesions would respond to 6 months of conservative therapy and that surgery would be indicated if pain would persist after 6 months of conservative treatment. Aglietti et al. [1] conducted a study including 16 juvenile patients with a mean age of 12.8 years and presented data, showing that in the case of intact cartilage surface, arthroscopic drilling of the juvenile OCD had to be carried out after an unsuccessful conservative therapy for an average time over a year to promote the healing of the OCD.
In 1999, Hefti et al. published a consensus paper on the diagnosis and treatment of OCD [6]. However, analysis of the results of this study reveals that no distinction was made between group A with 276 patients (male < 14 years and female < 13 years) with a mean age of 11.42 and group B with 176 patients with male patients over 14 years and female patients over 13 years of age with respect to eight different criteria, for example the correlation between clinical findings and dissection of the OCD in the imaging method. In addition to that, in this study, a high number of patients were used, but the oldest patient was over 31 years. Furthermore, MRI was only used in 12 % of all patients. In total, 53.8 % of all patients were evaluated with copies of the radiographs for the diagnosis of an OCD. This consensus paper of the European Paediatric Orthopaedic Society (EPOS) was rated very critical in 2012 in a Guideline and Evidence Report of the American Academy of Orthopaedic Surgeons (AAOS) Workgroup for diagnosis and treatment of OCD, published by Chambers et al. [3], because of the discrepancies mentioned above. However, also the AAOS Guidelines unfortunately are considered to stay weak, because there exists no specific recommendation on the diagnosis method of juvenile OCD nor on the lesion-dependent treatment option. Therefore, it is clear that no parameters exist, which define clear decision criteria and which allow a secure orientation for the orthopaedic surgeon when conservative therapy and when surgical therapy are indicated in juvenile patients with an OCD.
There are some limitations associated with the present study. The retrospective design of this study can be considered a limitation. The data collection was extracted only from the existing files. Second, the cohort was a mixed group of patients, including lesions in both the knee and the talus. Furthermore, there were only nine out of 63 patients with 3 T MRI. In addition to that, the study did not perform a direct comparison of 1.5 and 3 T scanners. To compare the accuracy of the two scanners, there would be the need to assess a series of juvenile patients with both scanners. Another limitation is that it was not the operative series of a single surgeon, and moreover, the surgeon who graded the lesions arthroscopically was not blinded to the preoperative MRI grade. Finally, the authors analysed the correlation between preoperative MRI and arthroscopy, but they did not investigate the clinical results and the long-term outcome of the juvenile patients.
Despite these limitations, the clinical relevance of this study from our point of view is that the children’s orthopaedist in day-by-day clinical work should not solely rely on the MRI when it comes to the decision to further conservative or surgical treatment of a juvenile OCD, but rather should take surgical therapy in consideration within persisting symptoms despite a low OCD stage provided by MRI.
Conclusions
Even with today’s modern MRI scanners, it is not possible to predict an accurate OCD stage in children. In this patient population always a relevant proportion can be found, which is often estimated too bad, but also outliers, which are judged to be good by MRI and cartilage damage is actually larger. Therefore, it must be considered that children with persisting pain despite an OCD stage I or II according to Dipaola et al. [4] should then be treated arthroscopically, since an arthroscopic surgery in a child with MRI findings appears justified.
References
Aglietti P, Buzzi R, Bassi PB, Fioriti M (1994) Arthroscopic drilling in juvenile osteochondritis dissecans of the medial femoral condyle. Arthroscopy 10(3):286–291
Cahill BR, Berg BC (1983) 99 m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med 11(5):329–335
Chambers HG, Shea KG, Anderson AF et al (2012) American Academy of Orthopaedic Surgeons clinical practice guideline on: the diagnosis and treatment of osteochondritis dissecans. J Bone Joint Surg Am 94(14):1322–1324
Dipaola JD, Nelson DW, Colville MR (1991) Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 7(1):101–104
Guhl JF (1982) Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res 167:65–74
Hefti F, Beguiristain J, Krauspe R et al (1999) Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B 8(4):231–245
Heywood CS, Benke MT, Brindle K, Fine KM (2011) Correlation of magnetic resonance imaging to arthroscopic findings of stability in juvenile osteochondritis dissecans. Arthroscopy 27(2):194–199
Iwasaki N, Kamishima T, Kato H, Funakoshi T, Minami A (2012) A retrospective evaluation of magnetic resonance imaging effectiveness on capitellar osteochondritis dissecans among overhead athletes. Am J Sports Med 40(3):624–630
Jurgensen I, Bachmann G, Schleicher I, Haas H (2002) Arthroscopic versus conservative treatment of osteochondritis dissecans of the knee: value of magnetic resonance imaging in therapy planning and follow-up. Arthroscopy 18(4):378–386
Kijowski R, Blankenbaker DG, Shinki K, Fine JP, Graf BK, De Smet AA (2008) Juvenile versus adult osteochondritis dissecans of the knee: appropriate MR imaging criteria for instability. Radiology 248(2):571–578
Koch S, Kampen WU, Laprell H (1997) Cartilage and bone morphology in osteochondritis dissecans. Knee Surg Sports Traumatol Arthrosc 5(1):42–45
Kocher MS, DiCanzio J, Zurakowski D, Micheli LJ (2001) Diagnostic performance of clinical examination and selective magnetic resonance imaging in the evaluation of intraarticular knee disorders in children and adolescents. Am J Sports Med 29(3):292–296
Lefort G, Moyen B, Beaufils P et al (2006) Osteochondritis dissecans of the femoral condyles: report of 892 cases. Rev Chir Orthop Reparatrice Appar Mot 92(Suppl 5):2S97-92S141
Makino A, Muscolo DL, Puigdevall M, Costa-Paz M, Ayerza M (2005) Arthroscopic fixation of osteochondritis dissecans of the knee: clinical, magnetic resonance imaging, and arthroscopic follow-up. Am J Sports Med 33(10):1499–1504
Mintz DN, Tashjian GS, Connell DA, Deland JT, O’Malley M, Potter HG (2003) Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation. Arthroscopy 19(4):353–359
Pascual-Garrido C, Moran CJ, Green DW, Cole BJ (2013) Osteochondritis dissecans of the knee in children and adolescents. Curr Opin Pediatr 25(1):46–51
Perumal V, Wall E, Babekir N (2007) Juvenile osteochondritis dissecans of the talus. J Pediatr Orthop 27(7):821–825
Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM (2003) Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop 23(1):102–108
Quatman CE, Quatman-Yates CC, Schmitt LC, Paterno MV (2012) The clinical utility and diagnostic performance of MRI for identification and classification of knee osteochondritis dissecans. J Bone Joint Surg Am 94(11):1036–1044
Ragozzino A, Rossi G, Esposito S, Giovine S, Tuccillo M (1996) Computerized tomography of osteochondral diseases of the talus dome. Radiol Med 92(6):682–686
Robertson W, Kelly BT, Green DW (2003) Osteochondritis dissecans of the knee in children. Curr Opin Pediatr 15(1):38–44
Trinh TQ, Harris JD, Flanigan DC (2012) Surgical management of juvenile osteochondritis dissecans of the knee. Knee Surg Sports Traumatol Arthrosc 20(12):2419–2429
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Roßbach, B.P., Paulus, A.C., Niethammer, T.R. et al. Discrepancy between morphological findings in juvenile osteochondritis dissecans (OCD): a comparison of magnetic resonance imaging (MRI) and arthroscopy. Knee Surg Sports Traumatol Arthrosc 24, 1259–1264 (2016). https://doi.org/10.1007/s00167-015-3724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3724-3