Abstract
This paper describes anteromedial rotatory laxity of the knee joint. Combined instability of the superficial MCL and the structures of the posteromedial corner is the pathological background anteromedial rotatory laxity. Anteromedial rotatory instability is clinically characterized by anteromedial tibial plateau subluxation anterior to the corresponding femoral condyle. The anatomical and biomechanical background for anteromedial laxity is presented and related to the clinical evaluation, and treatment decision strategies are mentioned. A review of the clinical studies that address surgical treatment of anteromedial rotatory instability including surgical techniques and clinical outcomes is presented.
Level of evidence V.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well accepted that the superficial medial collateral ligament is a primary static stabilizer preventing anteromedial rotatory instability (AMRI), valgus translation, external rotation and internal rotation about the knee [11, 35]. It has also been reported that the posterior oblique ligament (POL) is an important primary restraint to internal rotation and a secondary restraint to valgus translation and external rotation [10, 28]. A high frequency of combined superficial medial collateral ligament (sMCL) and POL injuries has been reported in knees with acute or chronic valgus laxity, signifying the important role of the POL in providing static stabilization to the medial knee [13]. Furthermore, untreated acute isolated or combined superficial medial collateral ligament and POL injuries have been reported to result in functional limitations and osteoarthritis [17]. Therefore, intensive rehabilitation of these common injuries may be necessary in some circumstances to prevent the pathologies associated with chronic medial knee instability.
Slocum and Larson [31] first described the term AMRI. This instability was described as excessive valgus motion coupled with external rotation of the knee. This occurs when the anteromedial tibial plateau subluxates anterior to the corresponding femoral condyle. The posteromedial corner has been shown to serve as an important restraint to AMRI throughout the normal range of motion [29].
Historic treatment of acute medial collateral ligament injuries has focused on non-operative therapies with early controlled motion with relatively good reported patient outcomes [5, 15, 24]. However, more severe acute and symptomatic chronic medial knee injuries may require operative management. Injuries that involve all medial and posteromedial structures, the superficial MCL, the deep MCL, the (POL) and the posterior capsule are characterized as a grade III injury and have a greater risk of developing chronic medial and rotatory instability requiring surgical treatment [33, 37]. Currently described surgical techniques for medial collateral stabilization include direct repair of the medial structures [14], primary repair with augmentation [7], advancement of the sMCL tibial insertion site [26], pes anserinus transfer [30], advancement with pes anserinus transfer [26] and non-biomechanically validated reconstruction techniques [2, 8, 38].
Few biomechanically validated anatomical reconstruction techniques using quantitatively described anatomical data [22, 37] to design reconstruction techniques of the sMCL and POL injuries have been reported. An anatomical reconstruction technique is preferable because it has been demonstrated that anatomical ligament reconstructions better approximate normal knee biomechanics [3, 6].
The purpose of this review is to present anatomical and biomechanical background for anteromedial rotatory instability including surgical management strategies and clinical outcomes of different surgical techniques.
Anatomical and biomechanical background for anteromedial rotatory instability
Anatomy
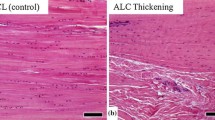
The primary structures involved in medial knee stabilization are the sMCL, the POL and the deep medial collateral ligament [19] (Fig. 1).
Illustration of the superficial medial collateral ligament (sMCL) (medial aspect, left knee) and posterior oblique ligament (POL). Reprinted with permission from [4, figure 1]
The sMCL, also named the tibial collateral ligament, is the largest structure of the medial aspect of the knee. This structure has one femoral and two tibial attachments. The femoral attachment is oval and is on average 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. Distally the sMCL has two tibial attachments. The proximal tibial attachment is a soft tissue attachment over the termination of the anterior arm of the semimembranosus tendon located 12 mm distal to the tibial joint line. The distal tibial attachment is a broad attachment directly to bone at an average of 61 mm distal to the tibial joint line located just anterior to the posteromedial crest of the tibia. The POL is a fibrous extension off the distal aspect of the semimembranosus, which blends with and reinforces the posteromedial joint capsule (Fig. 1). It consists of three facial attachments at the knee joint, with the most important portion being the central arm. On average, the central arm of the POL attaches on the femur 7.7 mm distal and 2.9 mm anterior to the gastrocnemius tubercle. The sMCL and the POL are separate structures [19].
The deep medial collateral ligament is comprised of the thickened medial joint capsule, which is deep to the sMCL. It is divided into meniscofemoral and meniscotibial components. The meniscofemoral ligament portion has an attachment 12 mm distal and deep to the sMCL’s femoral attachment. The meniscotibial ligament, much shorter and thicker than the meniscofemoral ligament portion, attaches just distal to the edge of the articular cartilage of the medial tibial plateau, which is 3 mm distal to the medial joint line and 9 mm proximal to the proximal tibial attachment of the sMCL [19].
Injury classifications
The grading of medial knee ligament injuries can be performed by physical examination and imaging. For the standard MCL examination, a valgus load at between 20° and 30° of knee flexion is applied with the patient in prone or supine position. The medial joint opening (joint line gapping) is estimated or measured, and the non-injured contralateral side is used as a baseline for comparison. In patients with acute injuries or who have sustained pain leading to guarding, performance of a valgus stress test or valgus stress radiograph may underestimate the amount of medial knee laxity.
The most widely utilized medial knee injury grading scale is the American Medical Association Standard Nomenclature of Athletic Injuries in which medial collateral injuries are graded from I to III [37]. Grade I or first-degree tear presents with localized tenderness and no laxity. Grade II or second-degree tear presents with broadened tenderness and an increased joint gapping. This represents partially torn medial collateral and posterior oblique fibres. Grade III or third-degree tear presents with a clear laxity without any resistance to an applied valgus stress. This represents a complete disruption of all medial structures.
Isolated medial knee injuries have also been classified in accordance with the amount of laxity observed at 30° of knee flexion with a valgus applied moment. These are grades 1+, 2+ and 3+, which have been reported to correspond to 3–5 mm, 6–10 mm and greater than 10 mm of subjective medial joint line gapping laxity when compared to the non-injured contralateral side [12]. There is no consensus of which clinical grading system is the best. Research is needed to determine which clinical grading system optimally detects MCL tissue injury and biomechanics.
Biomechanical properties of the medial ligamentous structures
The posteromedial corner (PMC) has been shown to serve as a restraint to AMRI throughout the normal range of motion [29]. The PMC is functionally composed of five anatomical structures: the posterior horn of the medial meniscus, the posterior oblique ligament (POL), the semimembranosus expansions, the meniscotibial (coronary) ligaments and the oblique popliteal ligament [29].
A biomechanical study has evaluated the impact of anatomical reconstruction of the MCL and posteromedial corner on valgus and rotatory stability [9]. Ten cadaveric knees were tested in the intact, sMCL and posterior oblique ligament sectioned and anatomically reconstructed states. The anatomical reconstruction technique involved single tendon strand reconstruction of the superficial MCL and POL with interference screw fixation at their anatomical femoral and tibial insertion sites. The reconstruction was supplied with an anchor fixation at the proximal tibial insertion of the superficial MCL (Fig. 2).
Right medial knee reconstruction procedure demonstrating the reconstructed sMCL and POL using two separate reconstruction strands with separate drill holes. Note that the proximal tibial attachment point of the sMCL, which was primarily to soft tissues and located just distal to the joint line, was recreated by anchor suturing the sMCL graft to the anterior arm of the semimembranosus muscle. Reprinted with permission from [4, figure 1]
Each knee was tested at 0°, 20°, 30°, 60° and 90° of knee flexion with a 10 Nm valgus load, 5 Nm external and internal rotation torques and 88 N anterior and posterior drawer loads. A six-degree-of-freedom electromagnetic motion tracking system was used to measure angulation and displacement changes in the tibia with respect to the femur. The study found a significant increase in valgus angulation and external rotation after sectioning the medial knee structures at all tested knee flexion angles. This was recovered following the anatomical medial knee reconstruction. A significant increase in anterior translation was observed after sectioning the medial knee structures at 20°, 30°, 60° and 90° of knee flexion, and this was recovered following MCL reconstruction for 20° and 30° of knee flexion. The study concluded that an anatomical medial knee reconstruction could restore pre-injured stability to a knee with a complete sMCL and posterior oblique ligament injury, while avoiding overconstraining the reconstructed ligament grafts. Another study by Petersen et al. [27] tested the importance of the POL in PCL-deficient knees. In their study, sectioning of the sMCL and deep MCL did not increase posterior instability, whereas sectioning of the POL resulted in significantly increased posterior instability.
Clinical evaluation of anteromedial instability
Examination of the superficial MCL is performed by valgus stress tests, which should be performed at both 0° and 20°–30° of flexion. As mentioned above, numerous injury classification systems exist to characterize different degrees of superficial MCL insufficiency. With the American Medical Association Standard Nomenclature of Athletic Injuries for grades I–III [37]. Grade I injury has no valgus gapping, grade II has clearly increased medial joint gapping but with a clear endpoint, and grade III has clear laxity without any endpoint to an applied valgus stress. Isolated medial knee injuries have also been classified in accordance with the amount of laxity observed at 30° of knee flexion with a valgus applied moment. These are grades 1+, 2+ and 3+, which have been reported to correspond to 3–5, 6–10 mm and >10 mm of subjective medial joint line gapping laxity when compared to the non-injured contralateral side [12].
A finding of valgus laxity at 0° indicates a concomitant cruciate ligament injury [34] but can also represent an injury and laxity of the posteromedial structures including the POL.
Stress radiography
Valgus stress radiographs can be useful for quantitative grading of medial knee instability and to identify the insufficient structures that result in the medial compartment gapping. One study reported that compared to the intact knee, medial joint gapping increases of 1.7 and 3.2 mm were produced at 0° and 20° flexion, respectively, by a clinician-applied load when isolated grade III superficial MCL injury was present. A complete medial knee injury involving sectioning of the superficial and deep MCL and POL resulted in gapping increases of 6.5 and 9.8 mm at 0° and 20°, respectively [18].
Anteromedial instability and posteromedial injury assessment (Table 1)
Anteromedial instability is characterized by combined lesion of the superficial MCL and POL and the posteromedial capsule. The anteromedial drawer test and the dial test can evaluate this combined lesion.
The anteromedial drawer test is performed by flexing the knee to approximately 90° while externally rotating the foot 10°–15° and applying an anteromedial rotational force to the knee. An anteromedial tibial plateau subluxation is a positive test and is indicative of POL and posteromedial capsule injury.
It has also been reported that a complete injury to the medial structures will cause increased external rotation at both 30° and 90° of knee flexion resulting in a positive dial test [32]. However, it is important to palpate the tibial plateau in relation to the femoral condyle while performing the dial test. If the tibial plateau performs an anteromedial subluxation, it is indicative of anteromedial instability, whereas a posterolateral subluxation is a sign of posterolateral instability [23].
Non-operative management of MCL lesions
Treatment for isolated, incomplete injuries grade I and II injuries to the MCL complex is non-operative. Grade I injuries can be managed without any brace with initial RICE treatment and subsequent return to activities within levels of pain. For grade II injuries, rehabilitation protocol is typically 4–6 weeks in a hinged brace with free range of motion. This allows for protection against valgus loading and provides normal biomechanical loading pattern through range of motion, which will stimulate proper alignment of ligament healing tissue [24]. Isolated grade III injuries can also be managed with similar non-operative strategies but in case of combined medial a cruciate ligament injuries acute medial repair can be considered [33]. However, there is sill significant controversy concerning the indications for acute operative repair for MCL complex injuries.
MCL repair techniques
Operative techniques that have been reported for acute direct repair of the superficial medial collateral ligament and posterior oblique ligament are numerous: such as primary repair with augmentation, advancement of the superficial medial collateral ligament tibial insertion site, pes anserinus transfer and advancement of the superficial medial collateral ligament with pes anserinus transfer [33]. As there is very little literature to define the indication for acute repair treatment, it is beyond the scope of the review paper to present all these possible surgical techniques.
However, in the setting of combined grade III MCL and bicruciate injuries, a more aggressive approach with repair or reconstruction of all lax structures can be considered. Another acute setting where repair should be considered is when the superficial MCL is torn from its tibial insertion and become displaced outside the pes anserinus tendons. Here, the ligament is unable to reattach to its insertion on the tibia with insufficient healing and increased risk of chronic instability as a result [24].
Also tibial-sided injuries to the meniscal attachment to the deep MCL and posteromedial capsule can be restored by placing suture anchors along the peripheral rim of the tibia and bringing them through the deep MCL [16].
Anatomical MCL reconstruction techniques
Medial knee ligament reconstruction techniques that address both the superficial MCL and the posterior oblique ligament have only been described in few studies. In this section, the main surgical techniques are described including the clinical data supporting the techniques. These techniques use hamstring tendon autografts. However, other MCL reconstruction techniques have been described using allografts or autografts for typically isolated reconstruction of the superficial MCL [1, 25].
LaPrade–Engebretsen MCL reconstruction technique (Fig. 2)
This anatomical technique consists of a reconstruction of the sMCL and posterior oblique ligament using two separate grafts with four reconstruction tunnels [21]. The approach can be performed with either one large medial knee incision or by using three smaller medial knee incisions to access the anatomical attachment points of the ligaments. The most proximal incision is made vertically along the medial knee and parallel to the long axis of the femur, essentially in line with the distal adductor magnus tendon, and measured a total of six cm in length. The distal end of this incision is located one cm proximal to the joint line, and the incision is placed five cm posteromedial to the medial border of the patella. Then, the femoral anatomical attachment points of the superficial MCL and POL are exposed by blunt dissection. The two distal incisions are also vertical and parallel to the long axis of the leg. With a 5-cm anteromedial incision, the tibial insertion of the sMCL is exposed. The sartorius muscle fascia is then incised, and the gracilis and semitendinosus tendons were exposed. The semitendinosus is then harvested using a hamstring stripper and sectioned into two parts, one measuring 16 cm for subsequent sMCL reconstruction and the other 12 cm for subsequent POL reconstruction. Each portion of the tendon is tubularized on both ends using No. 2 non-absorbable sutures to fit into 7-mm tunnels. Alternatively, allograft tendon may be used.
Attention is turned to the distal tibial attachment of the superficial MCL, approximately six cm distal to the joint line. The third and final incision is placed along the posteromedial border of the proximal tibia and allowed access to the tibial insertion of the POL (Fig. 2). This incision is two cm posterior to the posteromedial crest of the tibia and is five cm long. The most proximal edge of this incision is located one cm proximal to the joint line. Careful dissection is performed to identify the sartorial branch of the saphenous nerve through this incision. To protect the sartorial branch of the saphenous nerve, which usually courses posterior to the sartorius muscle belly and tendon at this level, the fascia anterior to the sartorius muscle tendon is incised, and the sartorius tendon is retracted distally. At this point, the attachment site of the central arm of the POL is identified at the posteromedial tibia near the direct arm of the semimembranosus tendon. After isolating the attachment locations of the superficial medial collateral and posterior oblique ligaments, attention is returned to drilling the reconstruction tunnels. Using an eyelet pin, 7-diameter and 30-mm-deep sockets are drilled at the femoral attachment of the sMCL and the posterior oblique ligament. The 16- and 12-cm sections of semitendinosus tendon that was previously tubularized are recessed 25 mm into the tunnel using an eyelet pin and fixed with 7-mm cannulated bioabsorbable screws.
The tibial tunnels for the distal sMCL and posterior oblique ligament anatomical attachment points are reamed in similar fashion next. The distal superficial MCL tunnel is reamed first through the centre of the distal superficial MCL anatomical attachment point located 6 cm distal to the joint line. Next, an eyelet pin is drilled through the centre of the tibial attachment of the central arm of the POL, which exited just distal and medial to Gerdy’s tubercle. A 7 × 30 mm socket is reamed. The superficial MCL graft is then passed under the fascia to the distal superficial MCL tunnel recessed to a depth of 25 mm. The knee is placed in 30° of knee flexion, in neutral rotation, and a varus force is applied to reduce any gapping of the medial compartment. The superficial MCL reconstruction graft is then tensioned and secured in place with a 7-mm bioabsorbable screw at the distal aperture of the tunnel. The knee is then placed through a full passive range of motion to verify proper positioning of the superficial MCL graft. The proximal tibial attachment point of the superficial MCL, which is primarily to soft tissues and located just distal to the joint line, is recreated by suturing the sMCL graft to the anterior arm of the semimembranosus muscle with a suture anchor. Finally, the POL graft is passed into the tibial tunnel and recessed. The graft is tensioned and secured with a 7-mm bioabsorbable screw
Clinical outcome of LaPrade–Engebretsen technique
A case series of 28 patients (19 male and 9 females) was operated between 2007 and 2009. The average age was 32.4 years (range 16–56 years). There were eight acute and 20 chronic injuries. All patients presented with subjective and objective valgus instability limiting activities of daily living and sports activities. Minimum follow-up was 6 months (average 1.5 years; range 0.5–3 years). It was found that subjective outcome evaluated by International Knee Documentation Committee (IKDC) Scores improved from preoperative 43.5 (range 14–66) to final postoperative values of 76.2 (range 54–88). Preoperative valgus stress radiographs averaged 6.2 mm of medial compartment gapping compared with the contralateral normal knee, whereas postoperative stress radiographs averaged 1.3 mm. [21]
Lind’s MCL reconstruction technique (Fig. 3)
This anatomical MCL reconstruction technique consists of a reconstruction of the sMCL and posterior oblique ligament using the semitendinosus tendon placed in one femoral tunnel and two tibial tunnels [22]. The approach can be performed with either one large medial knee incision or three smaller medial knee incisions to access the anatomical attachment points of the ligaments. The semitendinosus tendon is harvested at the pes anserinus, and the insertion at pes anserinus is kept intact. The medial femoral epicondyle is exposed through a longitudinal incision. The femoral MCL insertion site is identified just posterior to the medial epicondyle and anterior to adductor tubercle. An eyelet pin K-wire is drilled in the proximal centre of femoral MCL insertion. An 8 × 30 mm tunnel is drilled according to the measured diameter of the double-looped tendon. Now the released semitendinosus tendon is pulled along the K-wire and folded to create a tendon loop that will enable the loop to be recessed 25 mm into the femoral drillhole and fitted with No. 2 Fiberwire baseball suture. The semitendinosus tendon is then passed under the fascia to the femoral drill tunnel. The sutured loop is then passed into the tunnel with pull-through technique and fixed with an 8 × 25 interference screw to reconstruct the superficial MCL. The reconstruction is tightened at 10° of flexion and neutral rotation. The non-fixated free end of the tendon is now used for the posterior oblique ligament reconstruction. A tibial tunnel is then drilled at the posterior corner of the medial tibial condyle just proximal to tibial insertion of semimembranosus tendon. Tunnel diameter is the size of semitendinosus graft, which typically was 6 mm. The free end of graft is passed under the fascia from the femoral condyle to the tibial posterior oblique ligament tunnel. The graft is tensioned at 10° of flexion and fixed with an interference screw with the same diameter as the drill tunnel to reconstruct the posteromedial corner. The reconstruction will appear as an inverted V on the medial aspect of the knee (Fig. 2).
Medial knee reconstruction technique with combined sMCL and POL reconstruction using a single femoral fixation point. The semitendinosus tendon is released and the pes anserinus insertion retained. The tendon is looped into a drill hole in the medial femoral condyle. The free strand of the tendon is passed from posterior into a drill hole in the medial tibial condyle. Reprinted with permission from [22, figure 1]
Clinical outcome of Lind technique
In a case series, 61 patients with grade III or IV medial instability were treated with MCL reconstruction. Thirteen patients had isolated MCL reconstructions, 34 were combined with ACL reconstruction, and 14 were multiple ligament reconstructions. All had reconstruction of the medial collateral and the POL with a semitendinosus autograft. Fifty patients were available for follow-up more than 24 months postoperatively and were examined by an independent observer using objective IKDC measures and subjective Knee Osteoarthritis Outcome Score (KOOS). Objective IKDC medial stability at follow-up was in 98 % of patients normal or nearly normal (grade A or B). The overall objective IKDC score patients improved from 5 % grade A or B preoperatively to 74 %. Ninety-one per cent were satisfied or very satisfied with the result, and 88 % would go through surgery again. KOOS improved primarily for sports and quality of life subscales with approximately 10-point improvements. It was concluded that MCL reconstruction with combined collateral and POL reconstruction technique resulted in good clinical outcome in patients suffering from chronic valgus instability [22].
Discussion
Injuries to the medial collateral ligament comprise one of the most commonly injured ligaments of the knee, and combined MCL and POL injuries are frequently found in patients with valgus laxity about the knee joint [14]. All medial knee injuries with objective medial laxity should be managed by initial functional bracing to ensure optimal spontaneous healing. However, patients with grade III medial lesions and/or combined medial and cruciate ligament lesion have increased risk of developing chronic medial instability which may need surgical treatment [20].
Despite the presence of a high frequency of medial knee injuries, only limited literature presents biomechanically validated anatomical reconstruction techniques [4]. The results from a study by Widjicks et al. [36] suggest that an anatomical medial knee reconstruction technique can restore near normal stability to a knee following complete sectioning of the superficial MCL and POL. The anatomical medial knee ligament reconstruction techniques presented in this paper is supported by biomechanical validation and clinical data demonstrating good clinical outcome in a patients with both isolated MCL lesions and combined ligament reconstructions that included MCL reconstruction. This is reflective of the clinical variation of MCL instability patients [21].
Clinical evaluation of medial knee instability is challenging. Particularly, the separation of insufficiency of the individual medial structures can be difficult. Anteromedial rotatory instability is characterized by combined superficial MCL and POL instability.
Insufficiency of the superficial MCL is best evaluated by manual valgus examination. This examination can be supplemented by stress radiography. If the medial gapping of is more than 3 mm, an insufficiency of the superficial MCL is present. If stress radiography demonstrates a medial gapping of more than 6 mm, both superficial MCL and the POL are involved. Insufficiency of the POL can further be identified clinically by a positive anteromedial drawer test and positive dial test.
The clinical decision strategy for performing medial knee ligament reconstruction thus optimally relies on combined clinical and imaging evaluation. If substantial valgus instability can be established by clinical valgus examination, then this finding should be confirmed by stress radiography. If radiographic valgus laxity is confirmed, then good indications for medial ligament reconstruction exist. If in addition clinical signs of POL insufficiency exist in the form of positive anteromedial drawer test and dial test are present, then a surgical reconstruction strategy should include an anatomical reconstruction technique that addresses the superficial MCL and POL.
Such reconstruction techniques have been presented previously in this paper [21, 22].
There are several surgical considerations that can be made when performing medial ligament reconstructions. If isolated MCL reconstructions are performed, minimal invasive strategies can be considered using three small incisions. Alternatively one large medial incision could be used to approach the all the medial knee structures. We recommend the use of one large incision for obese patients or for more complex surgical cases such as multi-ligament procedures. For combined ACL and MCL instability, some surgeons avoid the usage of hamstring tendons for ACL reconstructions with combined MCL instability. The hamstring tendons are dynamic medial stabilizers so in theory preserving the hamstring tendons is beneficial for medial stability. However, no clinical studies have demonstrated that hamstring harvest increased objective or subjective medial stability.
Conclusion
In conclusion, anteromedial knee instability should be established by combined clinical and radiological evaluation. Management of anteromedial instability in chronic patients should involved reconstruction techniques that address both the superficial MCL and the posteromedial structures including the POL.
References
Borden PS, Kantaras AT, Caborn DN (2002) Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy 18(4):E19
Bosworth DM (1952) Transplantation of the semitendinosus for repair of laceration of medial collateral ligament of the knee. J Bone LaPrade Surg Am 34-A(1):196–202
Coobs BR, LaPrade RF, Griffith CJ, Nelson BJ (2007) Biomechanical analysis of an isolated fibular (lateral) collateral ligament reconstruction using an autogenous semitendinosus graft. Am J Sports Med 35(9):1521–1527
Coobs BR, Wijdicks CA, Armitage BM, Spiridonov SI, Westerhaus BD, Johansen S, Engebretsen L, LaPrade RF (2010) An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med 38(2):339–347
Ellsasser JC, Reynolds FC, Omohundro JR (1974) The non-operative treatment of collateral ligament injuries of the knee in professional football players. An analysis of seventy-four injuries treated non-operatively and twenty-four injuries treated surgically. J Bone Joint Surg Am 56(6):1185–1190
Giannotti BF, Fanelli GC, Barrett TA, Edson C (1996) The predictive value of intraoperative KT-1000 arthrometer measurements in single incision anterior cruciate ligament reconstruction. Arthroscopy 12(6):660–666
Gorin S, Paul DD, Wilkinson EJ (2003) An anterior cruciate ligament and medial collateral ligament tear in a skeletally immature patient: a new technique to augment primary repair of the medial collateral ligament and an allograft reconstruction of the anterior cruciate ligament. Arthroscopy 19(10):E21–E26
Grana WA, Gimple K (1981) Reconstruction of traumatic complete loss of the medial collateral ligament: a case report. Clin Orthop Relat Res 160:153–157
Griffith CJ, LaPrade RF, Johansen S, Armitage B, Wijdicks C, Engebretsen L (2009) Medial knee injury: part 1, static function of the individual components of the main medial knee structures. Am J Sports Med 37(9):1762–1770
Griffith CJ, Wijdicks CA, LaPrade RF, Armitage BM, Johansen S, Engebretsen L (2009) Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med 37(1):140–148
Grood ES, Noyes FR, Butler DL, Suntay WJ (1981) Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am 63(8):1257–1269
Hughston JC (1962) Acute knee injuries in athletes. Clin Orthop 23:114–133
Hughston JC (1994) The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament. Results of long-term follow-up. J Bone Joint Surg Am 76(9):1328–1344
Hughston JC, Eilers AF (1973) The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am 55(5):923–940
Indelicato PA, Hermansdorfer J, Huegel M (1990) Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res 256:174–177
Jacobson KE, Chi FS (2006) Evaluation and treatment of medial collateral ligament and medial-sided injuries of the knee. Sports Med Arthrosc 14(2):58–66
Kannus P (1988) Long-term results of conservatively treated medial collateral ligament injuries of the knee joint. Clin Orthop Relat Res 226:103–112
LaPrade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA (2010) Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med 38(2):330–338
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L (2007) The anatomy of the medial part of the knee. J Bone Joint Surg Am 89(9):2000–2010
Laprade RF, Wijdicks CA (2012) The management of injuries to the medial side of the knee. J Orthop Sports Phys Ther 42(3):221–233
LaPrade RF, Wijdicks CA (2012) Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res 470(3):806–814
Lind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE (2009) Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med 37(6):1116–1122
Lubowitz JH, Bernardini BJ, Reid JB 3rd (2008) Current concepts review: comprehensive physical examination for instability of the knee. Am J Sports Med 36(3):577–594
Marchant MH Jr, Tibor LM, Sekiya JK, Hardaker WT Jr, Garrett WE Jr, Taylor DC (2011) Management of medial-sided knee injuries, part 1: medial collateral ligament. Am J Sports Med 39(5):1102–1113
Marx RG, Hetsroni I (2012) Surgical technique: medial collateral ligament reconstruction using Achilles allograft for combined knee ligament injury. Clin Orthop Relat Res 470(3):798–805
O’Donoghue DH (1973) Reconstruction for medial instability of the knee. J Bone Joint Surg Am 55(5):941–954
Petersen W, Loerch S, Schanz S, Raschke M, Zantop T (2008) The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament-deficient knee. Am J Sports Med 36(3):495–501
Robinson JR, Bull AM, Thomas RR, Amis AA (2006) The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am J Sports Med 34(11):1815–1823
Sims WF, Jacobson KE (2004) The posteromedial corner of the knee: medial-sided injury patterns revisited. Am J Sports Med 32(2):337–345
Slocum DB, Larson RL (1968) Pes anserinus transplantation. A surgical procedure for control of rotatory instability of the knee. J Bone Joint Surg Am 50(2):226–242
Slocum DB, Larson RL (1968) Rotatory instability of the knee. Its pathogenesis and a clinical test to demonstrate its presence. J Bone Joint Surg Am 50(2):211–225
Slocum DB, Larson RL (2007) Rotatory instability of the knee: its pathogenesis and a clinical test to demonstrate its presence. 1968. Clin Orthop Relat Res 454:5–13 (discussion 13–14)
Tibor LM, Marchant MH Jr, Taylor DC, Hardaker WT Jr, Garrett WE Jr, Sekiya JK (2011) Management of medial-sided knee injuries, part 2: posteromedial corner. Am J Sports Med 39(6):1332–1340
Torg JS, Conrad W, Kalen V (1976) Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med 4(2):84–93
Warren LA, Marshall JL, Girgis F (1974) The prime static stabilizer of the medical side of the knee. J Bone Joint Surg Am 56(4):665–674
Wijdicks CA, Ewart DT, Nuckley DJ, Johansen S, Engebretsen L, LaPrade RF (2010) Structural properties of the primary medial knee ligaments. Am J Sports Med 38(8):1638–1646
Wijdicks CA, Griffith CJ, Johansen S, Engebretsen L, LaPrade RF (2010) Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am 92(5):1266–1280
Yoshiya S, Kuroda R, Mizuno K, Yamamoto T, Kurosaka M (2005) Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med 33(9):1380–1385
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Engebretsen, L., Lind, M. Anteromedial rotatory laxity. Knee Surg Sports Traumatol Arthrosc 23, 2797–2804 (2015). https://doi.org/10.1007/s00167-015-3675-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3675-8