Abstract
Purpose
Advanced knee arthritis in young patients is a challenging problem that may necessitate surgical treatment. There are few published studies of mobile-bearing unicompartmental knee arthroplasty (UKA) in young patients, while indications have expanded to its use in this demanding patient group.
Methods
The clinical and radiographic results of the first 118 consecutive Oxford medial UKAs (OUKA) using a minimally invasive technique (phase 3) in 101 patients 60 years of age or younger at the time of surgery were evaluated. Median age at surgery was 57 (25–60) years. Kaplan–Meier survivorship analysis was used to estimate implant survival.
Results
Mean time of follow-up evaluation was five (SD 1.6) years. At final follow-up, three patients (three knees) had died, and two patients (three knees) were lost to follow-up. Five knees were revised: three for unexplained pain, one for early infection and one for bearing fracture. There was one impending revision for progression of osteoarthritis in the lateral compartment. The radiographic review demonstrated that 5 % of the knees had progressive arthritis in the lateral knee compartment, of those 2 % with full joint space loss and pain. The Kaplan–Meier survival analysis, using revision for any reason as the endpoint, estimated the five-year survival rate at 97 % (95 % CI 91–99). Ninety-six per cent of the non-revised patients were satisfied with the outcome, and 4 % were dissatisfied. The mean Oxford knee score was 41 (SD 7), with 6 % of the knees having a poor result. The mean AKSS was 89 (SD 14), mean flexion was 129° (SD 13) and the mean UCLA score was 6.8 (SD 1.5).
Conclusion
Minimally invasive Oxford medial UKA was reliable and effective in this young and active patient cohort providing high patient satisfaction at mid-term follow-up. Progressive arthritis in the lateral knee compartment was a relevant failure mode in this age group. Most revisions were performed for unexplained pain, while we did not find loosening or wear in any patient.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee arthroplasty surgery is expected to increase by as much as 673 % from 2005 to 2030 [33]. In recent decades, the incidence of knee arthroplasty in younger patients (below 60 years of age) has been increasing disproportionately high and will continue to increase [38, 39]. Unicompartmental arthritis of the knee in young and active patients is a challenging therapeutic problem [18, 61]. There is continuing debate regarding the appropriate treatment in this patient cohort. Non-operative treatment often provides only limited pain relief and functional improvement in advanced knee arthritis [7, 14, 28, 47, 56]. Surgical options include high tibial osteotomy (HTO) [1, 11, 18, 19], total knee arthroplasty (TKA) [29] and UKA [48]. Survivorship after HTO, defined as time to arthroplasty, is reported variably in the literature, but the average survivorship is approximately 70–80 % at 10 years [21, 25, 44, 57, 63, 66]. Expectations regarding the functional outcome after knee arthroplasty surgery of younger patients are expected to differ importantly from those of older patients. A recent multicenter study revealed that about one-third of young patients reported residual symptoms and limitations after modern TKA even when performed by experienced surgeons in high-volume centres [49]. Minimally invasive UKA in patients in whom only one knee compartment is affected may provide some advantages over TKA such as more natural knee kinematic, quicker recovery, lower postoperative morbidity and mortality and preservation of bone stock [12, 26, 37]. Patients after UKA tend to achieve a better range of motion and more “normal feeling” of the replaced joint. Fully congruent mobile-bearing UKA has the potential to reduce long-term failure because of wear [55], which is a major concern affecting the survival of unicompartmental knee arthroplasty in young and active patients [48]. Despite the growing interest of surgeons in UKA and the broadening of its indication to younger and more active patients, there are only few studies on UKA in this patient cohort [17, 31, 48, 52, 53, 58, 65] and only one independent report on mobile-bearing Oxford medial UKA in this age group [31].
The purpose of the present study was to evaluate the clinical and radiological mid-term results of a large and independent series of the mobile-bearing Oxford medial UKA in young patients (≤60 years old at the time of surgery). In clinical practice, these data would be useful to inform younger knee osteoarthritis patients about the potential adverse effects and the clinical outcome of this treatment.
Materials and methods
This clinical and radiological study comprises our first 118 consecutive cemented Oxford medial UKAs (Biomet UK Limited, Swindon, UK) using a minimally invasive technique (phase 3) in 101 patients 60 years of age or younger at the time of surgery. Median age at surgery was 57 (25–60) years. All operations were performed at the same institution in a multisurgeon series (12 surgeons) between September 2001 and December 2007. The surgeons had absolved the instructional courses for this implant before their first surgery. On average, each surgeon performed 10 UKAs (range 4–22). Patient demographics are listed in Table 1. The patients were evaluated prospectively, and the data were reviewed retrospectively at a minimum of 2 years postoperatively.
The primary indication in 116 knees was medial compartment osteoarthritis with exposed bone; two knees were treated for avascular necrosis of the medial femoral condyle. The anterior cruciate ligament was functionally intact, and there was full thickness cartilage in the lateral compartment. The varus deformity was correctable at 20° flexion in all patients. Patello-femoral OA was not considered to be a contraindication unless there was deep eburnation and grooving. Furthermore, the presence of a chondral ulcer on the medial side of the lateral femoral condyle, age, weight, level of activity and presence of chondrocalcinosis were not considered as contraindication. Previous osteotomy and a varus or flexion deformity >15° were considered as a contraindication.
The surgical approach was a minimally invasive medial parapatellar incision without patella dislocation. The incision was made from the medial pole of the patella to the medial side of the tibial tuberosity. The details of the operative technique are given in the operative manual [20]. Care was taken to ensure that accurate ligament balance was achieved and that the bearing did not impinge on the retained bone or cement. All components were fixed with cement (Refobacin Bone Cement R; Biomet, Berlin, Germany).
Intravenous third-generation cephalosporin (single-shot 1.5 g cefuroxime) was administered perioperatively. Full weight bearing was allowed postoperatively. Anticoagulation therapy consisted of low molecular weight heparin (enoxaparin) administered subcutaneously the day before surgery and continued for 5 weeks postoperatively.
Patients were prospectively assessed clinically and radiologically preoperatively, at 3 and 12 months postoperatively, at 3 years and every 5 years thereafter using the functional and objective American Knee Society scores (AKSS-F and AKSS-O) [27] and the Oxford knee score (OKS) [15]. We used this score with a minimum of 0 (worst outcome) and maximum of 48 (best outcome) [40]. If for any reason the patients were unable to attend the follow-up, they were contacted by phone and relevant clinical information was obtained. For patients who had died, information was gathered from relatives and hospital/general practitioner records to establish whether the patient had undergone any further surgery on the knee under investigation. Pain was assessed using a visual analogue scale (VAS) ranging from 0 to 10 (0 = no pain to 10 = worst pain ever). Pre- and postoperative values of the University of California, Los Angeles (UCLA) activity scale [67] were obtained retrospectively at the last follow-up. The range of movement was measured using a long-arm goniometer, and any complications were recorded.
All the postoperative radiographs were aligned with fluoroscopic control. The anteroposterior film was aligned to obtain a view parallel to the tibial tray to standardise the view of the tibial bone–implant interface. The lateral view was aligned with the femoral condyles. Follow-up radiographs were assessed and compared with the postoperative radiographs, looking for the presence and extent of radiolucent lines under the tibial tray, the evidence of component subsidence and progression of osteoarthritis in the lateral compartment and patello-femoral joint. For assessment of progression of arthritis, the method described by Pandit et al. [45] was used. A subset of 50 radiographs was analysed by a single observer (MRS) twice, with a 6-month interval, to assess intraobserver reliability and was reviewed by a second observer (JS) to assess interobserver reliability. Intraobserver (κ = 0.88, p < 0.001) and interobserver agreement (κ = 1.00, p < 0.001) were high [35].
Informed consent was obtained from all patients. Procedures followed were approved by the institutional review board of the University of Heidelberg (S-065/2011), and the study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Statistical analysis
Kaplan–Meier survivorship analysis was performed with the use of the endpoint revision for any reason (defined as operations in which at least one of the components or the mobile bearing was changed). The 95 % confidence intervals were calculated using the exponential Greenwood formula. Pre- and postoperative scores were compared with the use of the Wilcoxon signed-rank test. p values of <0.05 were considered to be statistically significant. SPSS® version 20 (SPSS Inc., Chicago, IL) and Graphpad Prism® version 6.01 (Graphpad Software, San Diego, CA) were used to record and analyse the collected data.
Results
At final follow-up, three patients (three knees) had died during the study period for causes unrelated to their knee surgery, and two patients (three knees) were lost to follow-up; all lived abroad and were lost in the first year. The patients who died did not have revision surgery on the knee under investigation prior to death. A total of five patients had revision surgery, and one knee was scheduled for revision. The remaining 107 knees were available for review at a mean follow-up time of five (SD 1.6) years, and the median follow-up was four (2–9) years. Most knees (n = 92) had both clinical and radiological evaluations; 15 knees had only a clinical evaluation as the patients were unwilling or unable to have radiographs taken. In all those cases, we were able to obtain complete information about any reoperation on the knee under investigation, clinical scores, grade of satisfaction and pain on VAS. The distribution of knees at final follow-up is shown in Fig. 1.
Survival and complications
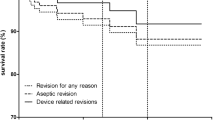
Kaplan–Meier survival analysis with revision for any reason as the endpoint estimated the cumulative 5-year survival at 97 % (95 % CI 91–99; 34 knees at risk; Fig. 2). Five knees were revised, one for suspected early infection, one for bearing fracture and three for unexplained pain (Table 2).
There were four additional knees requiring further interventions which were not counted as revisions as in none of these was the prosthesis or the bearing removed. One patient was revised for a tear of the knee capsule at the medial parapatellar approach after 2 months. The patient did well at final follow-up (OKS 37). Arthroscopy was undertaken in three knees for persistent pain. In two knees, synovitis was found at 2 and 17 months, respectively. A partial synovectomy was performed, and the patients did well thereafter (OKS 46 and 42 at final follow-up, respectively). In the third patient, a lateral menical tear was found, and the meniscus was partially resected at 56 months in this case, and the patient did well thereafter (OKS 41).
Clinical and radiographic outcome
The mean OKS, AKSS-O, UCLA Score, knee flexion angle and pain on VAS of the non-revised knees preoperatively and at the last follow-up are summarised in Table 3 and Fig. 3. All scores showed a significant improvement (p < 0.001). Table 4 shows the spread of patients with different grades of the OKS and AKSS score.
Box and whisker plots showing the outcome scores, UCLA activity scale, knee flexion angle and visual analogue scale (VAS) for pain preoperatively (preop) and at final follow-up (postop). ***p < 0.001 (OKS Oxford knee score, AKSS-O Objective American Knee Society score, UCLA University of California, Los Angeles)
Sixty-six patients (74 knees, 69 %) were very pleased, 26 (27 knees, 25 %) were pleased, one (2 knees, 2 %) was fairly pleased and four (4 knees, 4 %) were disappointed.
The radiographic review demonstrated that at final follow-up, 5 of 92 knees (5 %) evaluated had definitely progressive arthritis in the lateral knee compartment. Of those, two patients (two knees, 2 %) had full lateral joint space loss and complained of progressive pain while walking. One of those two was subsequently planned for revision to TKA.
Radiolucent lines under the tibial tray were found in 54 % (50) of the 92 knees. Of 50, 43 (86 %) of the radiolucent lines were partial, and seven (14 %) were complete. In all cases, the radiolucency had a sclerotic margin, and there was no evidence of either subsidence or loosening of either the femoral or tibial component in any patient. In one case, the radiolucencies were visible in the early postoperative radiographs; in all other knees, they became evident at follow-up.
Discussion
The most important finding of this study was a high implant survival and patient satisfaction at 5 years, suggesting that the Oxford mobile-bearing medial UKA is a reliable treatment option also in young patients in the mid-term. Our survival rate in this young patient cohort is comparable to the rate reported by the Oxford group at 7 years [45]. It is important to notice that these results were achieved in a multisurgeon series with relevant differences in surgical experience among the surgeons involved as seven of the twelve surgeons had performed <10 UKAs. To our knowledge, the present study reports on the largest series of Oxford UKA in patients aged 60 years or younger reported in the literature (Table 5).
The treatment of young patients with symptomatic anteromedial osteoarthritis of the knee is challenging, and the number of those patients is increasing [33, 65]. While cartilage repair procedures like microfracture, osteochondral autologous transfer or autologous chondrocyte implantation are important options in the treatment of isolated articular cartilage lesions in young patients and exciting treatment prospects for the future, today there is little evidence to support their use in more widespread OA of the knee [62]. The main surgical options for advanced OA with full thickness cartilage loss include HTO, UKA and TKA. Which option is most suitable depends upon patient characteristics and expectations. HTO is often considered as a potentially attractive option for younger patients who retains the desire to and wish to maximise the potential for returning to the highest level of function after surgery. Survivorship, defined as time to arthroplasty, is reported variably in the literature, but may be as high 98 at 10 and 90 % at 15 years [1]. However, reviewing the literature as a whole, the average survivorship is approximately 70–80 % at 10 years [21, 25, 44, 57, 63, 66]. The risk of failure after HTO increases with increasing age [21, 44, 66] and BMI > 25 [25] and seems to be higher in women than in men [44, 66]. Further, there is some evidence that the outcome and survival after HTO is better in patients with lower Ahlbäck grade of arthritis [9, 18] and higher preoperative functional outcome scores [24]. UKA has several advantages over TKA, including retention of the cruciate ligaments, preservation of bone stock, higher range of movement, lower morbidity and mortality and lower rates of infection [2, 3, 8, 12, 22, 26, 37, 46], which are of particular importance in young patients. On the other hand, data from national joint registries showed a higher revision/reoperation rate of UKA compared to TKA [37], and survival rates after Oxford UKA reported by registry data might be lower than those reported by the developing institution [34]. A recent study found a lower risk of revision in hospitals performing more than 40 UKA procedures a year than in those with fewer than 10 UKAs a year [6]. However, there are only few data on the outcome and survival of UKA in young patients [17, 31, 48, 52, 53, 58, 65] and only one independent report on mobile-bearing Oxford medial UKA in this age group [31].
Fully congruent mobile-bearing UKA appears to be an attractive alternative to fixed-bearing UKA in young and active patients as polyethylene wear remains the predominant failure mechanism of fixed-bearing UKA in this age group [4, 16, 48, 52]. In our series, wear was not a reason for failure, and we do not expect wear to become an issue in the longer term, as very low long-term wear rates (0.02 mm/year) have been reported for the Oxford medial UKA [55]. This might be a particular advantage in young and active patients and could be a main factor towards improving the long-term results of a UKA in this age group.
Unexplained pain was the most important reason for revision in the present study and is an important complication of both UKA and TKA [60]. The reason for this is still not fully understood, and outcomes after revision surgery might be worse when compared to patients with a defined cause of pain [30]. Our findings confirm previous reports as we found a relatively low mean OKS of 35 points and two of three patients were not satisfied with the outcome after revision for unexplained pain.
Progression of arthritis in the lateral knee compartment has been reported by the developers to be the most common reason for further surgical intervention after an medial Oxford UKA occurring in 0.9 % after 5.6 years [46]. In the literature, varying rates have been reported for other devices [32, 36, 42, 43]. We found definitely progressive lateral arthritis in 5 % of the knees evaluated radiographically, of those 2 % with lateral full thickness cartilage loss and progressive pain. Our rate of knees with definitely progressive arthritis in the radiographic evaluation is slightly higher than that reported by the developers after 5 years (3 %) [45]. These results suggest that, in the long-term, progression of arthritis in the lateral knee compartment might be the most important mode of failure also in younger patients. Further studies should focus on risk factors for this failure mode.
While cemented TKA in young patient cohorts has well-documented high survivorship in the mid-term [29], several trials report a high percentage of unsure or dissatisfied patients up to 20 %, most of them with seemingly well-fixed and well-positioned components [10, 59]. This might be a particular problem in the high-demanding young patients [29, 49]. Keenan et al. [29, 49] reported a poor result in 18 % of patients younger than 55 years of age at 5 years graded using the OKS as per the criteria of Pearse et al. [50] after cemented TKA. Further, Parvizi et al. [49] recently reported that one-third of young patients report residual symptoms and did not feel their prosthetic knee was normal even when the surgery was performed by experienced surgeons in high-volume centres [49]. The exact reason as to why such a high number of patients after TKA are dissatisfied remains unclear. Some believe that sacrifice of the ACL (and PCL), which are important proprioceptors in the knee, may cause the “abnormal” feeling that many patients with TKA report. Using a mobile-bearing UKA, we found that 62 % of the patients had an excellent outcome and 6 % had a poor result in the OKS graded as per the criteria of Pearse et al. [50]. These results compare favourably to those reported by Keenan et al. [29] using a TKA in patients 55 years or younger (32 % excellent and 18 % poor at 5 years). This finding should be considered when young patients with advanced anteromedial OA are counselled regarding the treatment options TKA and UKA.
In our series, most revisions were performed in the first two years postoperatively. This confirms the findings of previous studies [13, 41, 54, 64]. Further, previous long-term studies of cemented medial OUKA have shown that if the survival is good in the mid-term, it is likely to be good in the long term [54]. In our series, late failure occurred in one patient only at 8 years postoperatively and was related to breakage of a 3-mm bearing. In accordance with the manufacturer, we strongly recommend avoiding the use of a 3-mm bearing whenever possible, as the risk of breakage has shown to be much higher than using bearings 4 mm and thicker [51].
Main limitations of the present study are a relatively short minimum follow-up, the lack of control group (e.g. HTO or TKA) and that the data were analysed retrospectively. A further limitation is the fact that 15 % of the patients had no radiographs at all or no radiographs aligned with fluoroscopic control at final follow-up. This might introduce a possible bias in the radiographic results as early signs of failure (pathological radiolucencies or progressive lateral arthritis) might be visible only on fluoroscopic aligned X-rays. The main strength is that only 2 % of the patients were lost to follow-up.
Conclusion
Excellent clinical results in young patients with advanced arthritis were provided by the Oxford mobile-bearing UKA, and the results were comparable to TKA in terms of medium-term survivorship for patients 60 years of age or younger who maintain an active lifestyle. Our results suggest that the percentage of dissatisfied patients might be lower after an OUKA when compared to TKA. However, this finding could only be established in a prospective randomised controlled trial.
References
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy: a 10- to 20-year follow-up. J Bone Joint Surg Br 90:592–596
Argenson JN, Flecher X (2004) Minimally invasive unicompartmental knee arthroplasty. Knee 11:341–347
Argenson JN, Komistek RD, Aubaniac JM, Dennis DA, Northcut EJ, Anderson DT, Agostini S (2002) In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplast 17:1049–1054
Argenson JN, Parratte S (2006) The unicompartmental knee: design and technical considerations in minimizing wear. Clin Orthop Relat Res 452:137–142
Asif S, Choon DS (2005) Midterm results of cemented press fit condylar sigma total knee arthroplasty system. J Orthop Surg (Hong Kong) 13:280–284
Badawy M, Espehaug B, Indrekvam K, Havelin LI, Furnes O (2014) Higher revision risk for unicompartmental knee arthroplasty in low-volume hospitals. Acta Orthop 85:342–347
Bennell KL, Bowles KA, Payne C, Cicuttini F, Williamson E, Forbes A, Hanna F, Davies-Tuck M, Harris A, Hinman RS (2011) Lateral wedge insoles for medial knee osteoarthritis: 12 month randomised controlled trial. BMJ 342:d2912
Berger R, Della Valle C, Jacobs JJ, Sheinkop MB, Rosenberg AG, Galante JO (2006) The progression of patellofemoral arthrosis after medial unicompartmental replacement: results at 11–15 years. Clin Orthop Relat Res 452:285–286
Bonasia DE, Dettoni F, Sito G, Blonna D, Marmotti A, Bruzzone M, Castoldi F, Rossi R (2014) Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med 42:690–698
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ (2008) Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 90:1548–1557
Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ (2012) Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplast 27:86–90
Clement ND, Duckworth AD, MacKenzie SP, Nie YX, Tiemessen CH (2012) Medium-term results of Oxford phase-3 medial unicompartmental knee arthroplasty. J Orthop Surg (Hong Kong) 20:157–161
Crawford DC, Miller LE, Block JE (2013) Conservative management of symptomatic knee osteoarthritis: a flawed strategy? Orthop Rev (Pavia) 5:e2
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Deshmukh RV, Scott RD (2002) Unicompartmental knee arthroplasty for younger patients: an alternative view. Clin Orthop Relat Res 404:108–112
Felts E, Parratte S, Pauly V, Aubaniac JM, Argenson JN (2010) Function and quality of life following medial unicompartmental knee arthroplasty in patients 60 years of age or younger. Orthop Traumatol Surg Res 96:861–867
Flecher X, Parratte S, Aubaniac JM, Argenson JN (2006) A 12-28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 452:91–96
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2013) Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 21:170–180
Goodfellow J (2006) Unicompartmental arthroplasty with the Oxford knee. Oxford medical publications. Oxford University Press, Oxford, New York
Gstottner M, Pedross F, Liebensteiner M, Bach C (2008) Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg 128:111–115
Hanssen AD, Stuart MJ, Scott RD, Scuderi GR (2001) Surgical options for the middle-aged patient with osteoarthritis of the knee joint. Instr Course Lect 50:499–511
Heyse TJ, Khefacha A, Peersman G, Cartier P (2012) Survivorship of UKA in the middle-aged. Knee 19:585–591
Howells NR, Salmon L, Waller A, Scanelli J, Pinczewski LA (2014) The outcome at ten years of lateral closing-wedge high tibial osteotomy: determinants of survival and functional outcome. Bone Joint J 96:1491–1497
Hui C, Salmon LJ, Kok A, Williams HA, Hockers N, van der Tempel WM, Chana R, Pinczewski LA (2011) Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med 39:64–70
Hunt LP, Ben-Shlomo Y, Clark EM, Dieppe P, Judge A, MacGregor AJ, Tobias JH, Vernon K, Blom AW (2014) 45-day mortality after 467,779 knee replacements for osteoarthritis from the National Joint Registry for England and Wales: an observational study. Lancet 384:1429–1436
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jones RK, Nester CJ, Richards JD, Kim WY, Johnson DS, Jari S, Laxton P, Tyson SF (2013) A comparison of the biomechanical effects of valgus knee braces and lateral wedged insoles in patients with knee osteoarthritis. Gait Posture 37:368–372
Keenan AC, Wood AM, Arthur CA, Jenkins PJ, Brenkel IJ, Walmsley PJ (2012) Ten-year survival of cemented total knee replacement in patients aged less than 55 years. J Bone Joint Surg Br 94:928–931
Kerens B, Boonen B, Schotanus MG, Lacroix H, Emans PJ, Kort NP (2013) Revision from unicompartmental to total knee replacement: the clinical outcome depends on reason for revision. Bone Joint J 95:1204–1208
Kort NP, van Raay JJ, van Horn JJ (2007) The Oxford phase III unicompartmental knee replacement in patients less than 60 years of age. Knee Surg Sports Traumatol Arthrosc 15:356–360
Kozinn SC, Scott R (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71:145–150
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785
Labek G, Sekyra K, Pawelka W, Janda W, Stockl B (2011) Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop 82:131–135
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Laskin RS (1978) Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg Am 60:182–185
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445
Losina E, Thornhill TS, Rome BN, Wright J, Katz JN (2012) The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 94:201–207
Lutzner J, Hubel U, Kirschner S, Gunther KP, Krummenauer F (2011) Long-term results in total knee arthroplasty. A meta-analysis of revision rates and functional outcome. Chirurg 82:618–624
Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J (2007) The use of the Oxford hip and knee scores. J Bone Joint Surg Br 89:1010–1014
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80:983–989
Newman J, Pydisetty RV, Ackroyd C (2009) Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br 91:52–57
Newman JH, Ackroyd CE, Shah NA (1998) Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br 80:862–865
Niinimaki TT, Eskelinen A, Mann BS, Junnila M, Ohtonen P, Leppilahti J (2012) Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee: finnish registry-based study of 3195 knees. J Bone Joint Surg Br 94:1517–1521
Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW (2006) The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br 88:54–60
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br 93:198–204
Parkes MJ, Maricar N, Lunt M, LaValley MP, Jones RK, Segal NA, Takahashi-Narita K, Felson DT (2013) Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis. JAMA 310:722–730
Parratte S, Argenson JN, Pearce O, Pauly V, Auquier P, Aubaniac JM (2009) Medial unicompartmental knee replacement in the under-50s. J Bone Joint Surg Br 91:351–356
Parvizi J, Nunley RM, Berend KR, Lombardi AV Jr, Ruh EL, Clohisy JC, Hamilton WG, Della Valle CJ, Barrack RL (2014) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472:133–137
Pearse AJ, Hooper GJ, Rothwell A, Frampton C (2010) Survival and functional outcome after revision of a unicompartmental to a total knee replacement: the New Zealand National Joint Registry. J Bone Joint Surg Br 92:508–512
Pegg E, Pandit H, Gill HS, Keys GW, Svard UG, O’Connor JJ, Murray DW (2011) Examination of ten fractured Oxford unicompartmental knee bearings. J Bone Joint Surg Br 93:1610–1616
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2003) Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am 85:1968–1973
Price AJ, Dodd CA, Svard UG, Murray DW (2005) Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br 87:1488–1492
Price AJ, Webb J, Topf H, Dodd CAF, Goodfellow JW, Murray DW (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplast 16:970–976
Psychoyios V, Crawford RW, O’Connor JJ, Murray DW (1998) Wear of congruent meniscal bearings in unicompartmental knee arthroplasty: a retrieval study of 16 specimens. J Bone Joint Surg Br 80:976–982
Richards JD, Sanchez-Ballester J, Jones RK, Darke N, Livingstone BN (2005) A comparison of knee braces during walking for the treatment of osteoarthritis of the medial compartment of the knee. J Bone Joint Surg Br 87:937–939
Saragaglia D, Blaysat M, Inman D, Mercier N (2011) Outcome of opening wedge high tibial osteotomy augmented with a Biosorb(R) wedge and fixed with a plate and screws in 124 patients with a mean of ten years follow-up. Int Orthop 35:1151–1156
Schai PA, Suh JT, Thornhill TS, Scott RD (1998) Unicompartmental knee arthroplasty in middle-aged patients: a 2- to 6-year follow-up evaluation. J Arthroplast 13:365–372
Scott CE, Howie CR, MacDonald D, Biant LC (2010) Predicting dissatisfaction following total knee replacement: a prospective study of 1217 patients. J Bone Joint Surg Br 92:1253–1258
Simpson DJ, Price AJ, Gulati A, Murray DW, Gill HS (2009) Elevated proximal tibial strains following unicompartmental knee replacement–a possible cause of pain. Med Eng Phys 31:752–757
Springer BD, Scott RD, Sah AP, Carrington R (2006) McKeever hemiarthroplasty of the knee in patients less than 60 years old. J Bone Joint Surg Am 88:366–371
Sutton PM, Holloway ES (2013) The young osteoarthritic knee: dilemmas in management. BMC Med 11:14
Tang WC, Henderson IJ (2005) High tibial osteotomy: long term survival analysis and patients’ perspective. Knee 12:410–413
Ten Brinke B, de Haan LJ, Koenraadt KL, van Geenen RC (2014) Medial femoral condyle fracture as an intraoperative complication of Oxford unicompartmental knee replacement. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3459-6
W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S (2010) Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop 81:90–94
W-Dahl A, Robertsson O, Lohmander LS (2012) High tibial osteotomy in Sweden, 1998–2007: a population-based study of the use and rate of revision to knee arthroplasty. Acta Orthop 83:244–248
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplast 13:890–895
Acknowledgments
MRS. was supported by the non-commercial research fund of Deutsche Arthrose-Hilfe e.V. The study was supported by Biomet Inc.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Marcus R. Streit and Julia Streit have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Streit, M.R., Streit, J., Walker, T. et al. Minimally invasive Oxford medial unicompartmental knee arthroplasty in young patients. Knee Surg Sports Traumatol Arthrosc 25, 660–668 (2017). https://doi.org/10.1007/s00167-015-3620-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3620-x