Abstract
Purpose
To assess clinical outcomes and return to sport in an athletic population treated with autologous osteochondral transplantation (AOT) for osteochondral lesions of the talus.
Methods
A total of 36 patients were included in this retrospective study including 21 professional athletes and 15 amateur athletes who participated in regular moderate- or high-impact athletic activity. All patients underwent autologous osteochondral transplantation of the talus under the care of a single surgeon. At a mean follow-up of 5.9 years, patients were assessed using the American Orthopaedic Foot and Ankle Society (AOFAS) scoring system. All patients also received pre-operative MRI with the follow-up MRI performed at 1 year and underwent assessment of return to athletic activity.
Results
The overall AOFAS score improved from 65.5 (SD ± 11.1) to 89.4 (SD ± 14.4) (p = 0.01). At a final follow-up, 90 % of professional athletes (19 of 21) were still competing in athletic activity or still able to participate in unrestricted activity. Of the recreational athletes, 87 % (13 of 15) had full return to pre-injury activity levels, while two (13 %) returned to activity with restrictions or reduced intensity. MRI showed cystic change in 33 % of patients post-operatively; however, this did not appear to affect outcomes (n.s.). Donor site symptoms were seen in 11 % of the cohort at final follow-up, despite high function at donor knee.
Conclusion
The results of our study indicate that AOT procedure is able to achieve good outcomes in an athletic population at a midterm follow-up.
Level of evidence
Retrospective case series, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ankle sprains are a common joint injury with around 27,000 occurring every day in the USA alone [25, 32]. Inversion injuries account for 25 % of all musculoskeletal system injuries and are sports related in 50 % of cases [7, 8]. At the 2010 FIFA World Cup and 2008 Summer Olympic Games, ankle sprains were among the most commonly sustained injury, causing significant time lost from play [8, 24]. Imaging and arthroscopic studies show the incidence of talar osteochondral lesions (OCLs) to be upwards of 50 % in patients with chronic ankle instability and as high as 70 % with concurrent ankle fractures [3, 23, 31].
OCLs pose a significant challenge to orthopaedic surgeons as left untreated they have the potential to lead to increased pain and morbidity and may precipitate ankle joint arthritis [2, 15, 44].
Cartilage replacement strategies are indicated for patients with large or cystic OCLs or failed prior surgical treatment [4–6, 48]. Autologous osteochondral transplantation (AOT) has been recommended as a viable treatment option in lesions up to 4 cm2 [19]. In a recent systematic review, clinical outcomes for AOT in talar OCLs were good or excellent in 87 % of studies [48]. Despite this, there is a dearth of the literature reporting on return-to-sport outcomes following AOT of the talus in an athletic patient population [26, 39]. As talar OCLs are not uncommon in professional and recreational athletes, an understanding of clinical and return-to-sport outcomes in this cohort is important when selecting optimal treatment strategies. A systematic review by Mithoefer et al. [35] found that among the literature reporting on return to sports after surgical treatment for knee OCLs, 91 % of patients who underwent AOT returned to play compared to mean 73 % for all other procedures combine. Given the vastly differing biologic and mechanical properties of the knee and ankle joint, it is difficult to extrapolate these findings to ankle OCLs. Currently, rates of return to sport after AOT have been reported to range from 19 to 92 % [18, 45], and as such evidence to support the use of AOT in an athletic population is still inconclusive.
In this retrospective case series, we report the midterm clinical and return-to-sport outcomes of 36 athletic patients who underwent AOT procedure for OCLs of the talus.
Materials and methods
This study was approved by the ethics committee at Sociedade Beneficente Israelita Brasileira Hospital Albert Einstein, Sao Paulo, Brazil. A retrospective case series was undertaken and included thirty-six patients who underwent AOT procedure for OCL of the talus between August 2000 and December 2008 under the care of a single surgeon (M.P.). Inclusion criteria were an age of 18–65 years at time of surgery, magnetic resonance imaging (MRI) confirmed diagnosis of symptomatic talar OCL, no signs of degenerative joint changes on pre-operative imaging and patients who underwent moderate or intense activity on four or more days each week. Patients with inflammatory arthropathy or history of joint infection were excluded.
Patient variables and demographic information were collected including age at surgery, gender, history of trauma, type and level of pre-injury activity, location of lesion, containment of lesion and any previous ankle procedures, including microfracture (Table 1). Lesion location was recorded and categorized using the anatomical talar grid scheme described by Elias et al. [9]. Lesions covering more than one defined grid zone area were defined large and location recorded (Fig. 1), and further surface area measurements (mm2) were taken at time of operation.
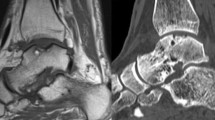
At the last office visit prior to surgery and at their final follow-up appointment, all patients were assessed with full history and physical examination and clinical outcomes were scored utilizing the American Orthopaedic Foot and Ankle (hindfoot) Score (AOFAS) [28]. At a final follow-up, outcomes were graded based on the AOFAS score with a score of 90–100 considered excellent; 81–90 good; 70–79 fair; and <70 poor. Pre-operative MRI was performed in all patients, and a routine follow-up MRI was done at the 12 months post-operative visit. All post-operative images were assessed by musculoskeletal radiologist for qualitative assessment of graft site integration, cartilage congruence, cyst formation and malleolar osteotomy union.
Return to sport was assessed at routine clinical follow-up visits and again at final follow-up, with a grade being assigned for the level of return to sport for each patient at 12-month follow-up, 24-month follow-up and final follow-up. Where possible, this included a consensus between athlete and team trainers and was defined as full return, restricted return or no return to sport. Full return described return to a functional performance at pre-injury level. Symptoms during play did not preclude a grade of full return provided symptoms did not interfere with performance. Restricted return included patients who returned to a lower level of athletic function or changed to a lower-impact sport. No return included any patients unable or unwilling to return to athletic activities. If full return to sport was not achieved, the cause for this was documented. Further subjective questioning was undertaken at the final follow-up, including requirement for pain relief, post-activity pain or swelling or other symptoms occurring during or following activity. Mean time to return to sporting activity was assessed in all patients.
Surgical technique
AOT procedures were performed using the OATS system© (Arthrex®, North Naples, FL, USA). Medial malleolar osteotomy was used when adequate access to medial talar dome was required and utilized a step-cut osteotomy in the frontal plane. Anterolateral lesions were accessed by plantar flexing the ankle without the need for an osteotomy; however, central or posterior lesions required either a fibular or tibial osteotomy as previously described [11, 32]. Lesion size was measured intra-operatively after the removal of any unstable cartilage at the lesion rim.
In all cases, the donor osteochondral graft was harvested from the lateral femoral condyle, distal to the sulcus terminalis, representing an area of minimal weight-bearing, with cartilage characteristics most similar to ankle cartilage [33, 34]. Donor plugs were diameters of 6, 8 or 10 mm. The femoral condyle was accessed by means of a mini-arthrotomy allowing visualization of the cartilage surface and matching of the topography to that of the talar region being replaced [26].
Graft placement was achieved using a press-fit technique and seated flush with native cartilage. The osteotomy was reduced and fixed with three titanium screws with attention paid to the tibial plafond articular surface alignment.
Rehabilitation
A standard rehabilitation protocol was instituted for all patients included in the study. For the first 2 weeks, patients were non-weight-bearing to allow initial graft integration. During this time, patients wore an orthosis except during physical therapy sessions where they underwent passive ankle and knee mobilization, isometric ankle strengthening and non-weight-bearing proprioceptive exercises.
From post-operative weeks two to six, physical therapy sessions were increased to incorporate hydrotherapy with the commencement of partial weight-bearing at one-third of the patient’s body weight. Active ankle mobilization with the addition of isotonic and proprioceptive exercises was employed, and walking exercises were allowed. From the sixth to twelfth post-operative week, progression to full weight-bearing was achieved. Running was still restricted at this time; however, aerobic activity on a stationary bike was allowed without restriction. Isotonic ankle exercises were continued during this period, and ice was used to prevent swelling following all physical therapy sessions. By 3 months post-surgery, a sport-specific rehabilitation programme was commenced. Decision regarding the timing of return to full sporting activity was made following consultation between physical therapist, team trainer, senior surgeon and athlete, with an aim for full return by 6 months post-operatively. Additionally, all donor knees were clinically assessed at follow-up for signs of chondromalacia patellae and, if present, vastus medialis strengthening and closed-chain short-arc quadriceps exercises were incorporated into the physical therapy routine.
Complications
At final follow-up, patients were assessed for donor site morbidity, and reports of knee pain, discomfort or other symptoms were documented. If a fibular or tibial osteotomy was required, then MRI signs of union were documented as were any complaints of persistent pain or other adverse outcomes at routine post-operative follow-up periods at the final follow-up visit.
Statistical analysis
Statistical analysis was carried out using SAS Software version 9.2 (SAS Institute, Inc., Cary, NC, USA). To assess statistical significance, an alpha value of 0.05 was used. Spearman rank correlations were used to assess the significance and strength of relationship between independent variables and clinical outcomes. Wilcoxon signed-rank tests were performed in order to compare scores for functional outcomes taken both pre- and post-operatively (AOFAS).
Results
Patient demographics
The patient cohort was a mean age of 31 ± 7.6 (range 16–43) years, with a 2:1 male to female ratio. Mean follow-up was 5.9 ± 2.5 (range 1–12) years. Lesion size was a mean of 133 ± 57 mm2 (range 56–380 mm2), and a mean of 1.4 ± 0.6 (range 1–3) grafts was used. Lesions were found to be uncontained in twenty-two patients, while 14 patients had contained talar dome lesions. Six patients (17 %) had previously undergone microfracture surgery which had subsequently failed. Concomitant procedures were required in 10 cases (28 %), and reoperation rates were required in three patients (8 %) at final follow-up (Table 1).
Clinical and radiological outcomes
Overall, the AOFAS score improved from a mean pre-operative score of 65.5 ± 11.1 to 89.4 ± 14.4 (p = 0.01) post-operatively, resulting in AOFAS outcomes being ‘excellent’ in 67 % of patients, ‘good’ in 19 %, fair in 11 % and poor in 3 %. There was no significant difference in AOFAS scores according to patient age, gender, lesion size, number of grafts, containment or whether prior microfracture or concomitant procedures were performed (n.s.) (Table 2). Correlation coefficients revealed no correlation between pre-operative, post-operative or change in AOFAS and lesion size or patient age (Table 3).
Patients who underwent concomitant procedures at time of AOT were found to have a significantly lower pre-operative AOFAS score than patients who had AOT procedure alone (p = 0.01); however, outcomes were similar in both groups at final follow-up. Additionally, patients who required a subsequent procedure after AOT surgery showed no significant difference in AOFAS scores at final follow-up compared to those with no requirement for subsequent surgery (n.s.) (Table 2).
Post-operative MRI revealed subchondral cystic change in 12 of the 36 (33 %) patients in our study. In these patients, AOFAS score was a mean 84.3 ± 16.1 compared to 93.2 ± 13.8 for patients with no cystic change (n.s.). MRI at 12 months post-operative revealed that two patients (6 %) had developed signs of early degenerative arthritis in their ankle. Mean post-operative AOFAS score for these patients was 66.5 ± 9.1 compared to 89.4 ± 11.7 for the entire cohort. One of these patients had a history of open ankle fracture which had been treated with open reduction, internal fixation 12 months prior to AOT. In addition, one patient showed poor graft–host cartilage integration with a cartilage surface ‘step-off’ deformity requiring revision AOT. All other patients had congruence of the graft–host cartilage interface. Malleolar osteotomy union was achieved in all patients by 12 months.
Return to sport
Of the 36 included patients, 21 were professional athletes (58 %) including 13 professional footballers, five volleyball players and three track and field athletes. The remaining 15 (42 %) patients were amateur athletes all of whom participated in moderate- to high-impact athletic activities 4 or more days each week. Overall, mean time to return to full activity was 6.1 ± 1.7 months (range 3.8–12). Return to pre-injury level of sport was achieved in 86 % of the patient cohort overall by 12 months and was maintained at final follow-up. A 10 % higher rate of full return to activity was noted in the professional cohort compared to the amateur cohort (90 vs. 80 %). Overall at 12- and 24-month follow-up, 5.5 % of patients were no longer participating in athletic activity, and at final follow-up, this number had increased to 8.3 % (Fig. 2).
Restricted return was seen in two of the professional athletes (10 %) at 12-month follow-up. One of these patients, however, required revision AOT at 12 months due to ongoing pain and poor graft integration on MRI and despite symptom resolution by 24 months did not resume sports due to concern for further injury and at final follow-up was graded as no return. The other professional athlete who did not achieve full return reported lack of confidence in the ankle with cutting movements and did not cite pain as the causative factor for not returning at full capacity. The remaining professional athletes (90 %) returned to play at pre-injury level, and at final follow-up, no patient had discontinued sport or restricted their activity due to concerns with the operative ankle.
In the amateur cohort, activity generally included competitive level running or football In this group, 80 % had returned to pre-injury activity level by 12 month with no attrition in rates of full return at final follow-up. One patient (7 %) in this cohort was unable to return to sport at 12 months, and by final follow-up, two patients (13 %) were graded as ‘no return’. Cause for restriction in activity was reported as ankle discomfort in both cases. Subjective questioning at final follow-up of those patients with full-return athletic activity revealed that three patients (10 %) experienced intermittent symptoms during or following activity. All three patients reported the occasional use of analgesia during activity; however, no restriction in functional performance was established.
Lesion location
A total of 23 lesions (64 %) occurred on the medial talar dome, and twelve (33 %) on the lateral. Additionally, of all lesions recorded, 72 % occurred on either the centromedial or centrolateral talar dome (Fig. 2). Larger lesions were found most commonly on the posteromedial talar dome followed by the anterolateral talar dome. Pre-operative AOFAS scores were similar, irrespective of lesion location or size and, despite larger lesions showing a smaller mean improvement in AOFAS of 19.4 ± 4.1 compared to 25 ± 3.7 for all other lesions, there was no significant difference between groups (n.s.). Similarly, lesion surface area did not appear to affect clinical outcomes at final follow-up.
Complications and donor site morbidity
There were no reported intra-operative complications. Superficial wound infection was noted in one patient and was successfully treated with a course of oral antibiotics. There were no cases of osteotomy non-union and only one patient with symptomatic hardware which resolved with hardware removal following union. Donor site morbidity was encountered in 11 % (4 of 36) of patients at mean of 5.9-year follow-up. Of these patients, three described discomfort in the knee with activity such as stair climbing and/or squatting and certain sport-specific movements and one patient described some discomfort with running. No patients had functional limitations of the donor knee, and there were no reports of knee instability, locking, swelling or need for walking aid.
Discussion
The most important finding in our study was that AOT for talar OCL in athletes resulted in good clinical outcomes and high rates of return to competitive and professional athletic disciplines. Return to sport following focal cartilage repair in the knee has been reported to be a mean of 73 % overall for all cartilage repair and replacement strategies, while taken alone AOT had mean rates of 91 % with the fastest return to sport compared to other cartilage repair techniques including chondrocyte implantation and bone marrow stimulation techniques (mean 7 months) [35]. Despite these promising results, clinical and return-to-sport outcomes following talar AOT are seldom reported in an athletic population [16, 39], and extrapolation of results in the knee for the application in the ankle is problematic. Paul et al. [39] reported on outcomes of AOT in the ankle and found that although sport was often resumed at some level, high-impact sports were often discontinued. Hangody et al. [16] reported that on a large series of athletes treated with mosaicplasty for OCLs in a range of joints, finding in knee to ankle mosaicplasty, 63 % of patients returned to full-level activity, 28 % returned to reduced level and 9 % were unable to return. In their study, fewer autograft plugs were associated with improved outcomes, which the authors proposed may be a result of the inherently better structural properties of larger osteochondral plugs, including higher pull-out strength, improved congruency and restoration of more normal contact pressures. In the current study, the majority of lesions were treated with single plug transplantation with the use of mini-arthrotomy, allowing visualization and topographical matching of donor and recipient site to ensure graft–host cartilage congruency. Recent evidence suggests that correct seating of osteochondral grafts can restore joint loading within an acceptable 6 % of normal [10]. Consequently, based on the current evidence, this graft site may be advantageous in allowing improved outcomes and likely contributed to the 86 % good or excellent results seen in the current study. In addition, all patients in the current study were involved in structured physical therapy regimen following surgery. In a recent review of rehabilitation techniques after cartilage repair, it was noted that an individually tailored approach to post-operative care resulted in improved return to sport [35]. Harris et al. [22] also demonstrated that competitive athletes had higher return to sports than recreational or non-active patients after cartilage repair, concluding that patient factors, including motivation and access to comprehensive rehabilitation programmes, were likely to be the cause for the difference.
In addition to encouraging rates of return to activity, good clinical outcomes were also achieved in the current study demonstrated by significant improvements in AOFAS scores at post-operative follow-up (p = 0.01). Our findings agree with those of previous AOT and mosaicplasty studies [1, 12, 13, 16, 17, 20, 26, 36] and highlight that at midterm follow-up AOT procedure is able to achieve good clinical outcomes in an entirely athletic cohort.
Predictors of outcome following AOT are of particular importance when treating professional athletes as a determination of the likelihood, and immediacy of returning to sport is of particular concern. Kim et al. [27] assessed predictors of outcomes in talar AOT procedures, finding that post-operative soft tissue impingement, uncovered lesion areas and arthroscopic findings such as cartilage surface incongruence resulted in significantly poorer outcomes. Conversely, they found no correlation with age, BMI, lesion size or lesion location and outcomes. These findings have been supported by a recent study by Woelfe et al. [47]; however, lesion size has been shown to affect outcomes in studies by Al-Shaikh et al. [1] and Kruez et al. [29]. Patient age, gender, containment of lesion, prior microfracture or lesion size or location did not correlate with clinical outcomes in our study (n.s.). These results may have been affected by our sample size or the relatively homogenous patient cohort as all patients were active and motivated to return to activity. In our study, lesion size and location had no significant effect on outcomes. Despite this, it was appreciated that the larger lesions in our study had lower mean AOFAS scores post-operatively. Based on the previous evidence [27, 47], it is possible that within our reported range of 80–380 mm2, lesion size does not have significant influence on outcomes, and it is still not clear from current evidence whether there is a critical lesion size that equates with poor outcomes in AOT for talar OCLs.
Cystic change was found in two-thirds of our cohort post-operatively and has been cited in the literature as a cause for concern following AOT surgery with rates as high as 75 % reported [13, 45]. Cystic change may compromise the integrity of the subchondral bone and potentiate loss of the overlying cartilage. Additionally, subchondral cysts may cause pain by stimulating the highly innervated subchondral bone and in turn lead to poorer clinical outcomes [37, 46]. It is thought that cystic change following AOT is a result of joint pressure under load causing ingress of synovial fluid into subchondral bone before graft–host integration has occurred [29, 37, 42]. Poor subchondral bony architecture has been shown to be one of the main reasons for the failure of cartilage repair [14, 21, 34, 40, 41, 43]. Our study, however, showed no effect of post-operative cyst formation on clinical outcomes at midterm follow-up (n.s.), which agrees with current evidence from talar AOT studies [27, 45]. Unfortunately, long-term data reporting the effect of subchondral cysts on patient outcomes are not available, meaning further studies assessing the prevalence, progression and long-term outcomes of cysts in post-operative AOT patients are needed.
Donor site morbidity (DSM) associated with knee to ankle AOT has been the focus of much debate. Reported incidence in the literature of donor site morbidity varies from 0 to 50 % [16, 18, 38, 39, 42, 45] with an overall incidence of 12 % reported in a recent systematic review [48]. In the current study, DSM was encountered in 11 % (4/36) of patients, suggesting that lateral knee arthrotomy and donor graft harvest do increase the risk of ongoing donor site symptoms. Although functional results were excellent at the donor knee in our cohort, it is important that athletes are counselled as to the risks of post-operative symptoms at the donor site.
Osteotomy non-union did not occur in our series, and only one case of discomfort around the medial malleolus was reported which was relieved by the removal of hardware after radiological union was achieved. Lamb et al. [30] reported on 62 patients who underwent medial malleolar osteotomy for talar AOT and found that 6 % of patients had pain following surgery at the osteotomy site, while almost all had satisfactory healing with encouraging cartilage morphology on quantitative T2 mapping of cartilage surface at the osteotomy site.
The authors acknowledge the limitation of the current study being the retrospective nature of the study design and use of only one outcome score pre- and post-operatively for patient assessment. However, the use of AOFAS is useful, given that the majority of previous AOT outcome studies have utilized it when assessing clinical outcomes. Additionally, subjective assessment of return to sport is likely to introduce bias in reporting. We attempted to mitigate this bias by including athletes trainers in the assessment of functional return to activity whenever possible. Unfortunately, the lack of a validated assessment of return to sports after cartilage surgery in the ankle limits the comparative value of results obtained from a case series. Similarly, although the current study reports on a relatively large athletic patient population, sample size limitations exist in terms of being able to find correlation between patient and lesion factors and outcomes.
Conclusion
In conclusion, the results of our study indicate that AOT procedure is able to achieve good clinical outcomes in an athletic population while allowing high rates of return to sports in the medium term. This is clinically relevant as many of OCLs occur as a result of trauma during athletic activities. Long-term follow-up studies are required to assess whether rates of athletic participation and clinical outcomes are maintained, and a standardized assessment of return to sport may be useful in comparing surgical option for talar OCL and their use in athletes.
References
Al-Shaikh RA, Chou LB, Mann JA, Dreeben SM, Prieskorn D (2002) Autologous osteochondral grafting for talar cartilage defects. Foot Ankle Int 23(5):381–389
Buckwalter JA, Mankin HJ (1998) Articular cartilage: degeneration and osteoarthritis, repair, regeneration, and transplantation. Instr Course Lect 47:487–504
Cha SD, Kim HS, Chung ST, Yoo JH, Park JH, Kim JH, Hyung JW (2012) Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg 20124(4):293–299
Choi WJ, Park KK, Kim BS, Lee JW (2009) Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med 37(10):1974–1980
Choi WJ, Kim BS, Lee JW (2012) Osteochondral lesion of the talus: could age be an indication for arthroscopic treatment? Am J Sports Med 40:419–424
Chuckpaiwong B, Berkson EM, Theodore GH (2008) Microfracture for osteochondral lesions of the ankle: outcome analysis and outcome predictors of 105 cases. Arthroscopy 24:106–112
Czajka CM, Tran E, Cai AN, DiPreta JA (2014) Ankle sprains and instability. Med Clin North Am 98(2):313–329
Dvorak J, Junge A, Derman W, Schwellnus M (2011) Injuries and illnesses of football players during the 2010 FIFA World Cup. Br J Sports Med 45(8):626–630
Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM (2007) Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int 28(2):154–161
Fansa AM, Murawski CD, Imhauser CW, Nguyen JT, Kennedy JG (2011) Autologous osteochondral transplantation of the talus partially restores contact mechanics of the ankle joint. Am J Sports Med 39(11):2457–2465
Garras DN, Santangelo JA, Wang DW, Easley ME (2008) A quantitative comparison of surgical approaches for posterolateral osteochondral lesions of the talus. Foot Ankle Int 29(4):415–420
Gautier E, Kolker D, Jakob RP (2002) Treatment of cartilage defects of the talus by autologous osteochondral grafts. J Bone Joint Surg Br 84(2):237–244
Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G (2006) Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation. Arthroscopy 22:1085–1092
Gomoll AH, Madry H, Knutsen G, van Dijk N, Seil R, Brittberg M, Kon E (2010) The subchondral bone in articular cartilage repair: current problems in the surgical management. Knee Surg Sports Traumatol Arthrosc 18(4):434–447
Grunfeld R, Ayodogan U, Juliano P (2014) Ankle arthritis review of diagnosis and operative management. Med Clin North Am 98(2):267–289. doi:10.1016/j.mcna.2013.10.005
Hangody L, Dobos J, Baló E, Pánics G, Hangody LR, Berkes I (2010) Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med 38(6):1125–1133
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85-A(Suppl 2):25–32
Hangody L, Rathonyi GK (2004) Mosaicplasty in active sportsmen. Sportorthopadie Sporttraumatologie 20:159–164
Hangody L, Rathonyi GK, Duska Z (2004) Autologous osteochondral mosaicplasty. Surgical technique. J Bone Joint Surg 86-A:65–72
Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L (2008) Autologous osteochondral grafting: technique and long-term results. Injury 39(Suppl 1):S32–S39
Hannon CP, Smyth NA, Savage-Elliot I, Deyer TW, Calder JDF, Kennedy JG (2014) Osteochondral lesions of the talus: aspects of current management. Bone Joint J 96-B:164–171
Harris JD, Brophy RH, Siston RA, Flanigan DC (2010) Treatment of chondral defects in the athlete’s knee. Arthroscopy 26:841–852
Hintermann B, Regazzoni P, Lampert C, Stutz G, Gächter A (2000) Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg [Br] 82-B:345–351
Junge A, Engebretsen L, Mountjoy ML, Alonso JM, Renström PA, Aubry MJ, Dvorak J (2009) Sports injuries during the Summer Olympic Games 2008. Am J Sports Med 37(11):2165–2172
Karlsson J, Sancone M (2006) Management of acute ligament injuries of the ankle. Foot Ankle Clin 11(3):521–530
Kennedy JG, Murawski CD (2011) The treatment of osteochondral lesions of the talus with autologous osteochondral transplantation and bone marrow aspirate concentrate: surgical technique. Cartilage 2(4):327–336
Kim YS, Park EH, Kim YC, Koh YG, Lee JW (2012) Factors associated with the clinical outcomes of the osteochondral autograft transfer system in osteochondral lesions of the talus: second-look arthroscopic evaluation. Am J Sports Med 40(12):2709–2719
Kitaoka HB, Alexander IJ, Adelaar RS et al (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15(7):349–353
Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Henle P, Niemeyer P (2006) Mosaicplasty with autogenous talar autograft for osteochondral lesions of the talus after failed primary arthroscopic management. Am J Sports Med 34(1):55–663
Lamb J, Murawski CD, Deyer TW, Kennedy JG (2013) Chevron-type medial malleolar osteotomy: a functional, radiographic and quantitative T2-mapping MRI analysis. Knee Surg Sports Traumatol Arthrosc 21:1283–1288
Leontaritis N, Hinojosa L, Panchbhavi VK (2009) Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am 91(2):333–339
Lynch SA, Renström PA (1999) Treatment of acute lateral ankle ligament rupture in the athlete conservative versus surgical treatment. Sports Med 27(1):61–71
Marymont JV, Shute G, Zhu H, Varner KE, Paravic V, Haddad JL, Noble PC (2005) Computerized matching of autologous femoral grafts for the treatment of medial talar osteochondral defects. Foot Ankle Int 26:708–712
Messner K (1993) Hydroxylapatite supported Dacron plugs for repair of isolated full-thickness osteochondral defects of the rabbit femoral condyle: mechanical and histological evaluations from 6 to 48 weeks. J Biomed Mater Res 27:1527–1532
Mithoefer K, Hambly K, Della Villa S, Silvers H, Mandelbaum BR (2009) Return to sports participation after articular cartilage repair in the knee: scientific evidence. Am J Sports Med 37(1):167S–176S
Nakagawa Y, Suzuki T, Matsusue Y, Kuroki H, Mizuno Y, Nakamura T (2005) Bony lesion recurrence after mosaicplasty for osteochondritis dissecans of the talus. Arthroscopy 21(5):630
Nosewicz TL, Reilingh ML, Wolny M, van Dijk CN, Duda GN, Schell H (2013) Influence of basal support and early loading on bone cartilage healing in press-fitted osteochondral autografts. Knee Surg Sports Traumatol Arthrosc 22(6):1445–1451
Paul J, Sagstetter A, Kriner M, Imhoff AB, Spang J, Hinterwimmer S (2009) Donor-site morbidity after osteochondral autologous transplantation for lesions of the talus. J Bone Joint Surg Am 91(7):1683–1688
Paul J, Sagstetter M, Lämmle L, Spang J, El-Azab H, Imhoff AB, Hinterwimmer S (2012) Sports activity after osteochondral transplantation of the talus. Am J Sports Med 40(4):870–874
Qiu YS, Shahgaldi BF, Revell WJ, Heatley FW (2003) Observations of subchondral plate advancement during osteochondral repair: a histomorphometric and mechanical study in the rabbit femoral condyle. Osteoarthritis Cartilage 11:810–820
Radin EL, Rose RM (1986) Role of subchondral bone in the initiation and progression of cartilage damage. Clin Orthop Relat Res 213:34–40
Sammarco GJ, Makwana NK (2002) Treatment of talar osteochondral lesions using local osteochondral graft. Foot Ankle Int 23:693–698
Scranton PE Jr, Frey CC, Feder KS (2006) Outcome of osteochondral autograft transplantation for type-V cystic osteochondral lesions of the talus. J Bone Joint Surg Br 88(5):614–619
Thomas RH, Daniels TR (2003) Ankle arthritis. J Bone Joint Surg Am 85-A(5):923–936
Valderrabano V, Leumann A, Rasch H, Egelhof T, Hintermann B, Pagenstert G (2009) Knee-to-ankle mosaicplasty for the treatment of osteochondral lesions of the ankle joint. Am J Sports Med 37(Suppl):105S–111S
van Dijk NC, Zengerink RM, van Bergen CJ (2010) Osteochondral defects in the ankle: why painful? Knee Surg Sports Traumatol Arthrosc 18:570–580
Woelfle JV, Reichel H, Nelitz M (2013) Indications and limitations of osteochondral autologous transplantation in osteochondritis dissecans of the talus. Knee Surg Sports Traumatol Arthrosc 21(8):1925–1930
Zengerink M, Struijs PA, Tol JL, van Dijk CN (2010) Treatment of osteochondral lesions of the talus: a systematic review. Knee Surg Sports Traumatol Arthrosc 18(2):238–246
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fraser, E.J., Harris, M.C., Prado, M.P. et al. Autologous osteochondral transplantation for osteochondral lesions of the talus in an athletic population. Knee Surg Sports Traumatol Arthrosc 24, 1272–1279 (2016). https://doi.org/10.1007/s00167-015-3606-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3606-8