Abstract
Purpose
To investigate the biomechanical properties of the load shifting following opening-wedge distal femoral varus osteotomies (DFVOs) and determine the osteotomy correction needed to unload the lateral compartment.
Methods
Five human cadaveric knees were tested with a load of 500 N of axial compression. Medial and lateral tibiofemoral compartment contact area and pressure were assessed utilizing a modified F-scan pressure-sensitive sensor. The knees were tested in their baseline anatomic alignment, 10° valgus malalignment and following corrective DFVOs of 5°, 10° and 15°. The load shifting effect of the various DFVO correction angles was analysed using a one-way ANOVA to determine the correction angle necessary to unload the lateral compartment.
Results
Gradually shifting the loading vector medially with increasing DFVO angles resulted in a decrease in the mean contact area and mean contact pressures in the lateral compartment with progressive increases in the medial compartment. The largest reduction in lateral compartment pressure and contact area was seen with the 15° osteotomy with a 25 % decrease in mean contact pressure and 20 % decrease in mean maximum contact pressure and mean contact area when compared to the 10° valgus-malaligned knee. For the 10° valgus knee, a 15° correction resulted in near-normal contact pressures and areas compared with the knee in normal anatomic alignment.
Conclusion
Progressive unloading of the lateral tibiofemoral compartment occurred with increasing DFVO correction angles. Clinically, when performing a DFVO for valgus malalignment, surgeons should consider overcorrecting the osteotomy by 5° to restore near-normal contact pressures and contact areas in the lateral compartment rather than the traditional teaching of correcting to neutral alignment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The young patient with symptomatic unicompartmental arthritis is the ideal candidate for a realignment osteotomy procedure [8, 14–16, 21]. Although less frequent than isolated medial arthritis due to varus deformities [10], lateral compartment arthritis coupled with valgus malalignment is a challenging problem. The altered limb alignment leads to increased load being distributed to the cartilage of the lateral compartment [3, 10–12, 16]. As a result, the lateral half of the tibial plateau supports a significant amount of body weight, and the valgus malalignment accentuates the stress on damaged articular cartilage, causing further degenerative changes and more angular deformity.
Multiple tibial and femoral osteotomy techniques have been developed to transfer abnormal mechanical loads from the lateral compartment to a more medial position [24]. Unfortunately, most varus-producing high tibial osteotomies (HTO) have led to unsatisfactory results as shown by Shoji and Insall [18]. A distal femoral varus osteotomy (DFVO) is typically utilized in patients with moderate to large valgus deformities [11, 14–16] with the anteroposterior joint line typically deviated from the horizontal by 10 or more degrees [3]. Recent long-term case series report a 10-year survivorship following DFVO ranging from 82 to 87 % using conversion to TKA as an endpoint [2, 8, 27]. Opening-wedge DFVO has several advantages over medial closing-wedge DFVO and medial closing-wedge HTO, including technical ease and the ability to correct large deformities [7, 14, 15]. Intended tibiofemoral correction angles in the literature have ranged from the more typical 0° [2, 6, 26, 27] to correction goals from 3° of valgus [4] to 3° of varus [20].
Apart from a few clinical outcome studies, there is a lack of experimental data on the biomechanical effect of the load redistribution produced by the DFVO in the orthopaedic surgery literature [2, 6, 13, 17]. The purpose of the current study was to investigate the biomechanical properties of load shifting in DFVOs and determine the osteotomy correction needed to effectively unload the lateral compartment. The hypotheses of the study were that increasing the degree of correction would shift the contact area and pressures from the lateral compartment to a more medial location and that normalization of the contact areas and pressures would occur with a correction that was equivalent to the initial deformity.
Materials and methods
Specimen preparation
Five fresh-frozen human cadaveric knees, cut midway on the shafts of both the femur and the tibia, were utilized. The median age of the donors was 59 years (range 55–66); all donors were male. The joints were examined to ensure they had not been injured and had not been operated on previously. Plain radiographs were taken before biomechanical testing to exclude joints with advanced osteoarthritis. The anatomic lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA) were measured to ensure that all specimens were within the normal range (median mLDFA 88°, range 85°–90°; median mMPTA 87°, range 85°–90°).
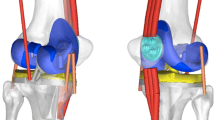
After the specimens were thawed overnight, the joints were dissected with the removal of the skin and all subcutaneous tissue. The joints were opened through a medial parapatellar arthrotomy, and the quadriceps muscles and the patella were removed. The medial and lateral collateral ligaments as well as the cruciate ligaments were left intact, as were the posterior joint capsule and the popliteus. There were no ligament instabilities and no meniscal lesions present in our group of specimens. Evaluation of the cartilage revealed very minor patellofemoral degenerative changes, but no lesions on the tibiofemoral surfaces. Ten centimetres of the proximal femur and 10 cm of the distal tibia were freed from all soft tissues, and the bone ends were embedded into steel pipe sections using Bondo acrylic cement (Maplewood, Minnesota, USA). The pipe on the femur was attached to a proximal composite femur (Sawbones Generation 3, Vashon, WA) and adjusted so all specimens had the same length. The femoral head was held in a custom-made jig that allowed rotation but no translation. The custom-made jig for the tibia was held in an angle vise that was used to simulate a valgus malalignment of 10°.
Each specimen was attached to the MTS machine (MTS, Eden Prairie, MN) and aligned at an anatomic position by positioning the vise before fixing to the base so that the centre of the femoral head lay over the centre of the knee (Fig. 1). The specimens were then loaded by axial compression to 500 N. Pressure measurements were taken after 1 min of loading to allow the soft tissues, cartilage and meniscus to equilibrate. Five different testing configurations were utilized, with the first configuration being the control specimens in which the knees were tested in their normal anatomic position with the knee in full extension. This was followed by testing with the knee placed in the 10° simulated valgus malalignment and then repeat testing. The testing concluded with each 10° valgus-malaligned knee undergoing sequential corrective distal femoral lateral opening-wedge osteotomies of 5°, 10° and 15°, respectively, followed by testing after each correction [1, 26].
Experimental set-up. A custom-made fixture was used to simulate different loading situations of the lower leg by varying the mechanical alignment angle of the distal tibia. A proximal femur prosthetic fixture was attached to the proximal femur bone stump, and loads were directly applied to the femoral head to mimic mechanical alignment. The F-scan system was used to measure the changes in the pressures in the medial and lateral compartments
Surgical technique
The distal femoral osteotomy was made with an oscillating saw under fluoroscopic guidance in a lateral to medial direction, from a proximal point on the lateral cortex, 3 cm above the lateral epicondyle to the medial side just proximal to the medial epicondyle perpendicular to the femoral axis leaving a 1-cm hinge of bone medially [26]. Alignment correction was performed using one of three different cut wedges of varying degrees (5°, 10° and 15°) made from solid urethane foam (density of 0.80 g/cm3, Sawbones, Vashon, WA) inserted into the osteotomy site and secured with a lateral plate and screws (Synthes LCP 5 Hole Distal Femoral Plate; West Chester, PA).
Tibiofemoral cartilage pressure assessment
A modified F-scan pressure-sensitive sensor (F-Scan; Tekscan, Boston, MA) was used for contact pressure analysis. The F-scan sensors were 0.18 mm thick and were cut to a width of 22 mm for insertion into the medial and lateral tibiofemoral compartments. The sensors were preconditioned and calibrated according to the standardized protocol as suggested by the manufacturer. The F-scan system has been established for dynamic force and contract pressure analysis, measuring pressures at a range of 0.10–17.20 MPa with a resolution of 0.07 MPa and contact areas with an accuracy of 0.05 cm2 [1]. The F-scan sensors were inserted into the medial and lateral tibiofemoral compartments from anterior to posterior, being carefully pulled into the joint space on top of the cartilage and menisci using number 1 silk sutures passed in inside-out fashion through the posterior and medial and lateral joint capsule. Care was taken to ensure that the sensors were well seated on the cartilage surface without wrinkles and completely covered the tibial plateau articular surfaces and menisci [1]. Contact area (CA; measured in cm2), contact pressure (CP; measured in MPa) and maximum contact pressure (MCP; measured in MPa) were extrapolated from the software. Two measurements were taken for each condition with the mean reported for each measurement.
Statistical analysis
One-way ANOVA with alpha set at 0.05 was undertaken to test for differences amongst the varying valgus–varus positions of the knee. Statistical Analysis Software version 9.3 (SAS Institute Inc., Cary, NC) was used to perform all statistical measures and analyses.
Results
Anatomic knee
Testing of the knees at baseline anatomic alignment demonstrated a mean contact pressure (mCP) of 0.53 MPa in the medial compartment and 0.42 MPa in the lateral compartment. The mean maximum contact pressure (mMCP) in the medial compartment and the lateral compartment was 0.71 and 0.55 Mpa, respectively. The mean contact area in the medial compartment was 7.84 cm2 compared with a mean contact area of 6.76 cm2 in the lateral compartment (Table 1).
Distal femoral lateral opening-wedge osteotomy
Mean contact pressures (mCP)
The mean contact pressures in the medial compartment progressively increased as the knee alignment was corrected from 10° of valgus malalignment with an increasing amount of varus opening (Fig. 2). As expected, the shift towards increased pressures in the medial compartment coincided with decreased mean contact pressures in the lateral compartment of the valgus-aligned knees.
Mean contact pressure. The graph demonstrates clear unloading of the lateral compartment as the valgus-malaligned knee was corrected with increasing distal femoral varus osteotomies. An opening-wedge osteotomy of 15° led to a normalization of the medial and lateral mean contact pressures (0.50 and 0.43 MPa) to near anatomic medial and lateral mean contact pressures (0.53 and 0.42 Mpa, respectively), and this finding was found to be statically significant (p < 0.05)
Mean maximum contact pressures (mMCP)
The mean maximum contact pressures of the medial compartment increased from 0.51 ± 0.07 MPa in the 10° valgus-malaligned knee to a value of 0.70 ± 0.08 MPa following the 15° corrective DFVO (p < 0.05). Similar to the mCP measurements, the lateral compartment demonstrated a gradual decrease in mMCP from the valgus alignment to the increasingly varus alignments (Fig. 3).
Mean maximum contact pressure. The graph demonstrates clear unloading of the lateral compartment as the valgus-malaligned knee was corrected with increasing distal femoral varus osteotomies. An opening-wedge osteotomy of 15° led to a normalization of the medial and lateral mean maximum contact pressures (0.70 and 0.59 MPa; both are significant p < 0.05) to near anatomic medial and lateral mean maximum contact pressures (0.71 and 0.55 Mpa, respectively)
Contact areas
A progressive decrease was noted to be present with respect to the contact area in the lateral compartment of the knee as the corrective lateral opening-wedge osteotomy was increased from 5° to 15° and subsequently shifted the load to the medial compartment. Furthermore, there was an increase in the contact area of the medial compartment of the knee as the knee shifted from valgus alignment to increasingly varus alignments. More specifically, the mean total contact area of the five specimens was found to be 14.52 ± 1.12 cm2 with the majority of the total contact area in the lateral compartment area of the knees in 10° of valgus malalignment (8.43 cm2 lateral vs. 6.24 cm2 medial). As the degree of the corrective DFVO was increased in the valgus-aligned knee, the majority of the contact area reversed to the medial compartment (7.42 cm2 medial vs. 6.92 cm2 lateral) (Fig. 4).
Mean contact areas. The combined medial and lateral compartment mean contact areas remained relatively stable in all alignment simulations. The lateral and medial compartment mean contact area gradually approached anatomic mean contact area as the valgus-malaligned knee was corrected with increasing distal femoral varus osteotomies. The anatomically aligned knee medial and lateral compartment contact areas were 7.84 ± 0.85 and 6.76 ± 0.69 cm2, respectively. The corrective 15° varus opening-wedge osteotomy significantly shifted medial and lateral compartment contact areas closely to anatomic values 7.42 ± 0.8 and 6.92 ± 0.51 cm2, respectively (p < 0.05)
Discussion
The most important finding of the present study was that over-correcting valgus deformity may serve to better unload the lateral compartment and better recapitulate the normal biomechanics of the native joint than correcting to neutral alignment which is the traditional thinking during distal femoral osteotomy. In theory, any shift from a neutral or collinear alignment of the hip, knee and ankle affects the load distribution in the knee joint [22]. The lateral shift of the load-bearing axis in a valgus knee has resultant increases in the moment arm and compartment pressures in the lateral compartment. Numerous animal model and surgical-based studies [3, 12, 22] have demonstrated the critical importance of knee alignment as a predictor of outcomes following surgical procedures of the knee. Varus-producing osteotomies of the distal femur are a good surgical option for the purpose of unloading the affected lateral compartment and correcting underlying valgus malalignment in high-demand active patients with symptomatic unicompartment gonarthrosis [9, 13, 19, 23, 25]. Numerous retrospective studies have shown the value of DFVOs in appropriately selected patients. Survivorship with a primary endpoint of conversion to TKR has been demonstrated to range from 64 to 90 % at 10 years [2, 6, 16, 26, 27] and 45 to 79 % at 15 years [2, 23]. While clinical studies have demonstrated successful outcomes following DFVOs in the treatment of lateral compartment osteoarthritis, to date there have not been any studies investigating the biomechanical effect of the load redistribution produced by the DFVO in the orthopaedic surgery literature.
The current study found that by simulating 10° valgus malalignment, the intra-articular mean contact pressure (mCP) in the lateral compartment exceeded that in the medial compartment by approximately 50 %, a greater than twofold reversal in compartment pressures when compared to normal anatomic alignment controls. Additionally, there was a complete reversal in peak pressures in the 10° vaglus-malaligned knee compared with our controls, with MCmMCP and LCmMCP of 0.71 and 0.55 MPa in our control group, respectively, versus MCmMCP and LCmMCP of 0.51 and 0.73 MPa in our 10° valgus malalignment model, respectively. Similarly, there was a twofold reversal in contact area (CA) distribution in our 10° vaglus malalignment model compared with our normal anatomic controls, with the shift occurring from predominantly medial in the normal model to predominantly lateral in the valgus malalignment model.
Gradually shifting the loading vector medially by performing corrective distal femoral lateral opening-wedge osteotomies of 5°, 10° and 15° resulted in progressive increases in mCP and mCA in the medial compartment with proportional decreases in the lateral compartment. The largest decreases in lateral compartment pressure and area measurements were seen following a 15° corrective DFVO, whereby there was a 25 % decrease in mCP, a 20 % decrease in mMCP and a 20 % decrease in CA when compared to measurements from the knee in the setting of 10° valgus malalignment. Similarly, there was an approximate 66 % increase in medial compartment mCP, with an approximate 40 % increase in mMCP and an approximate 20 % increase in CA.
Interestingly, it was only with the 15° corrective distal femroal varus osteotomy (where MCmCP exceeding LCmCP by 14 %) that equalization of compartment pressures and mean contact areas was obtained that was most consistent with measurements obtained in normal anatomic alignment (where MCmCP exceeded LCmCP by approximately 20 %). This is further supported when comparing measurements between the 10° and 15° corrective DFVOs. The increase from 10° to 15° resulted in a shift from greater mCP and mCA in the lateral compartment relative to medial compartment following the 10° corrective DFVO, to greater pressures and contact areas in the medial compartment relative to the lateral compartment following the 15° corrective DFVO. These data suggest that a 15° correction into varus is ideal for decompression of the lateral compartment in the setting of 10° valgus malalignment, assuming that the pressure distribution after an osteotomy is identical to these experiments. One may extrapolate from these data that over-correcting valgus deformity may serve to better unload the joint and better recapitulate the normal biomechanics of the native joint. These data contribute to the paucity of information regarding correction goals in the context of DFVO; current clinical studies [2, 4–6, 11, 15, 20, 27] vary with regard to their recommended correction of valgus malalignment with no uniform trend towards any particular correction goal being definitive [17].
However, it is important to note that the present study has several limitations. Given the nature of this cadaveric biomechanical study, the model is not physiologic and the assessment was based on a single static application of load. There are no dynamic muscular and soft tissue forces incorporated into the model which likely play a role in joint loading. Additionally, as there are no prior biomechanical studies investigating the impact a distal femoral osteotomy has on the contact pressures and areas in the tibiofemoral compartment, the experimental model is based on prior studies looking at high tibial osteotomies. In these studies, the axial load applied ranged from 450 to 1000 N without much rationale for the applied load utilized. The current study utilized a single 500 N axial load to replicate the forces seen during the initial stance phase of gait. Future studies will attempt to improve the model by incorporating dynamic and rotational forces to the experimental set-up in addition to investigating cyclic loading and its impact on contact pressures and areas.
Conclusion
Increasing the correction angle of lateral opening-wedge DFVO leads to decreased contact pressure and area in the lateral compartment of knees in valgus malalignment. These results suggest that patients with early lateral compartment osteoarthritis in the setting of valgus malalignment who are not good candidates for joint replacement surgery may benefit from a corrective opening-wedge distal femoral osteotomy. Clinically, when performing a DFVO for valgus malalignment, surgeons should consider over-correcting the osteotomy by 5° to restore near-normal contact pressures and contact areas in the lateral compartment rather than the traditional teaching of correcting to neutral alignment.
References
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23:852–861
Backstein D, Morag G, Hanna S, Safir O, Gross A (2007) Long-term follow-up of distal femoral varus osteotomy of the knee. J Arthroplasty 22:2–6
Bruns J, Volkmer M, Luessenhop S (1994) Pressure distribution in the knee joint. Influence of flexion with and without ligament dissection. Arch Orthop Trauma Surg 113:204–209
Das DST, Hoekstra H, vanLeeuwen W (2008) Distal femoral opening-wedge osteotomy for lateral compartment osteoarthritis of the knee. Open Access Surg 1:25–29
Dewilde TR, Dauw J, Vandenneucker H, Bellemans J (2013) Opening wedge distal femoral varus osteotomy using the Puddu plate and calcium phosphate bone cement. Knee Surg Sports Traumatol Arthrosc 21:249–254
Finkelstein JA, Gross AE, Davis A (1996) Varus osteotomy of the distal part of the femur. A survivorship analysis. J Bone Joint Surg Am 78:1348–1352
Franco V, Cipolla M, Gerullo G, Gianni E, Puddu G (2004) Open wedge osteotomy of the distal femur in the valgus knee. Der Orthopade 33:185–192
Haviv B, Bronak S, Thein R, Thein R (2013) The results of corrective osteotomy for valgus arthritic knees. Knee Surg Sports Traumatol Arthrosc 21:49–56
Insall JN, Joseph DM, Msika C (1984) High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Joint Surg Am 66:1040–1048
Johnson EW Jr, Bodell LS (1981) Corrective supracondylar osteotomy for painful genu valgum. Mayo Clin Proc 56:87–92
McDermott AG, Finklestein JA, Farine I, Boynton EL, MacIntosh DL, Gross A (1988) Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am 70:110–116
McKellop HA, Llinas A, Sarmiento A (1994) Effects of tibial malalignment on the knee and ankle. Orthop Clin N Am 25:415–423
Omidi-Kashani F, Hasankhani IG, Mazlumi M, Ebrahimzadeh MH (2009) Varus distal femoral osteotomy in young adults with valgus knee. J Orthop Surg Res 4:15
Puddu G, Cipolla M, Cerullo G, Franco V, Gianni E (2007) Osteotomies: the surgical treatment of the valgus knee. Sports Med Arthrosc 15:15–22
Puddu G, Cipolla M, Cerullo G, Franco V, Gianni E (2010) Which osteotomy for a valgus knee? Int Orthop 34:239–247
Rosso F, Margheritini F (2014) Distal femoral osteotomy. Curr Rev Musculoskelet Med 7:302–311
Saithna A, Kundra R, Getgood A, Spalding T (2014) Opening wedge distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. Knee 21:172–175
Shoji H, Insall J (1973) High tibial osteotomy for osteoarthritis of the knee with valgus deformity. J Bone Joint Surg Am 55:963–973
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Joint Surg Am 85-A:469–474
Stahelin T, Hardegger F, Ward JC (2008) Supracondylar osteotomy of the femur with use of compression. Osteosynthesis with a malleable implant. J Bone Joint Surg Am 82:712–722
Sternheim A, Garbedian S, Backstein D (2011) Distal femoral varus osteotomy: unloading the lateral compartment: long-term follow-up of 45 medial closing wedge osteotomies. Orthopedics 34:e488–e490
Tetsworth K, Paley D (1994) Malalignment and degenerative arthropathy. Orthop Clin N Am 25:367–377
Tjornstrand BA, Egund N, Hagstedt BV (1981) High tibial osteotomy: a seven-year clinical and radiographic follow-up. Clin Orthop Relat Res 160:124–136
Uquillas C, Rossy W, Nathasingh CK, Strauss E, Jazrawi L, Gonzalez-Lomas G (2014) Osteotomies about the knee: AAOS exhibit selection. J Bone Joint Surg Am 96:e199
Vainionpaa S, Laike E, Kirves P, Tiusanen P (1981) Tibial osteotomy for osteoarthritis of the knee. A five to ten-year follow-up study. J Bone Joint Surg Am 63:938–946
Wachtl SW, Gautier E, Jacob RP (2000) Supracondylar femoral osteotomy for osteoarthritis of the knee. Surg Techn Orthop Traumatol 55:520-E-10
Wang JW, Hsu CC (2005) Distal femoral varus osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am 87:127–133
Conflict of interest
No conflicts of interest exist for any authors related to the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quirno, M., Campbell, K.A., Singh, B. et al. Distal femoral varus osteotomy for unloading valgus knee malalignment: a biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 25, 863–868 (2017). https://doi.org/10.1007/s00167-015-3602-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3602-z