Abstract
Purpose
The purpose was to measure the effect of flexion and additional rotation of the femur relative to the tibia on the tuberosity–trochlear groove distance (TT–TG) in the same subject in 20 cadaveric knees joint.
Methods
In 20 human adult cadavers, formal fixed knees (age: 81.9 years, SD 12.3; 10 female) CT scans were performed in extension and 30° of flexion as well as in neutral, maximal possible internal (IR), and external rotation (ER). On superimposed CT scan images, TT–TG was measured in each position. TT–TG measurements were correlated in all knee positions.
Results
TT–TG in full extension/neutral rotation was 7.8 mm (SD 3.4, range, 2.4–15.3). TT–TG in full extension and IR was significantly lower, and TT–TG in full extension and ER was significantly higher than in neutral rotation (5.4 ± 2.3 vs. 10.9 ± 4.8 mm; P < 0.001). IR and ER varied between 1.0°–7.6° and 0.2°–9.2°, respectively. TT–TG in 30° flexion/neutral rotation was 3.9 mm (SD 1.8, range, 1.3–7.8), which was significantly lower than in full extension and neutral rotation (P < 0.001). TT–TG in 30° flexion and IR was significantly lower, and TT–TG in 30° flexion and ER was significantly higher than values obtained in neutral rotation (2.7 ± 1.2 vs. 6.5 ± 3.4 mm; P < 0.001). IR and ER in 30° flexion varied between 0.6°–10.7° and 1.9°–13.0°, respectively.
Conclusion
Flexion as well as rotation of the knee joint significantly alters the TT–TG. These results may have wider clinical relevance in assessing TT–TG and further decisions based on it.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The tibial tuberosity–trochlear groove distance (TT–TG) quantifies the distance between the anterior tibial tuberosity and the deepest point of the trochlear groove in the coronal plane on the millimetre scale. High values are a factor in operative decision making to stabilize the patella in order to medialize the tibial tuberosity [5, 11].
The measurement of TT–TG is not standardized. In the original description, the knee is flexed to 30°, but now many papers describe this measure in full extension [8, 25]. However, measuring TT–TG in a flexed or an extended knee will lead to different values. The screw-home mechanism, i.e., an outward tibial rotation in full extension, is responsible for this discrepancy [10].
Beside this discussion, an effect of additional rotation of the tibia relative to the femur has never been raised as an issue in previous literature on the TT–TG. Rotational laxity can be unpredictable in normal knees and vary between 9.4° to 14.5° of internal or 13° of external rotation in full extension [6, 16, 23]. In 30° of flexion, internal rotation can be 8.6° and external rotation up to 30° [6, 16]. In 90° of flexion, an external rotation of more than 35° and internal rotation of about 25° are described. [31] Additional rotational ligament instabilities of the knee joint are often undiagnosed, but can increase rotation significantly [30, 31].
From this point of view, the question is whether a rotational instability or an increased knee ligamentous laxity beside screw-home mechanism would alter the TT–TG.
Therefore, the purpose of this study was to measure the effect of flexion and additional external or internal rotation of the femur relative to the tibia on the TT–TG distance in cadaveric knee joints.
The hypothesis was therefore that flexion and/or rotation will significantly change the TT–TG.
To our knowledge, this is the first study that sheds light on rotational issues influencing the TT–TG measurement. This question and hypothesis are relevant for the clinical assessment of patients with patello-femoral instability. An inconsistent measurement of TT–TG due to ligamentous laxity or instability might influence decision making regarding realignment procedures.
Materials and methods
This study was designed as a human cadaver study, approved by the responsible ethical committee (University of Basel Nr. 32/11) with 20 human, adult, cadaveric, formal fixed knees (age: 81.9 years, SD 12.3; 10 females). These cadavers were also part of a study conducted by Nowakowski [24].
Inclusion criteria: cadaver knees with intact ligamentous stabilizers and menisci but without muscles, subcutaneous fat, and skin were included. The extensor apparatus with the patella remained in situ.
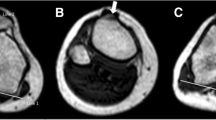
Exclusion criteria: cadavers with scars indicating a former history of operation, i.e., for trauma, patella-femoral dislocations, rotatory, or ligamentous instabilities (fig. 1).
Tuberosity–trochlear groove distance (TT–TG) measured on superimposed CT scans (double yellow arrow between two red lines). This quantifies the distance between the most anterior part of the tibial tuberosity and the deepest point of the trochlear groove in the coronal plane on the millimetre scale. The green oval lines define both condyles according to a protocol described by Nowakowski et al. [24]. These condyles were adjusted to a standardized coordinate system. The axial slices were aligned perpendicular to the sagittal axis (green vertical line). This permitted a constant and comparable measurement
The specimens were mounted in a manufactured custom-made device (Fig. 2a, b). This device fixed both femur and tibia, but allowed controlled flexion and rotation of the femur relative to the tibia [24].
In full extension and 30° of flexion, the bones were positioned in neutral, maximal possible internal and external rotation relative to one another. In each of these six positions, a CT scan was performed, and TT–TG distance was measured. Imaging was performed with a helical GE Lightspeed 16 row CT scanner (General Electric Healthcare Corporation Waukesha. W1): 120 kV, slice thickness 0.625 mm, Voxel depth 0.5 mm, Voxel height 0.296875 mm, and Voxel width 0.296875 mm.
3D-VRT (rendering technique) models were created out of these CT scans and imported to visualization software (VGStudio Max 2.1.1) (Fig. 2c). According to a protocol described by Nowakowski et al. [24], CT scans were oriented to a standardized coordinate system and the axial slices perpendicular to the sagittal axis. This permitted a constant and comparable measurement of the TT–TG in extension and in 30° of flexion, independently of how the plane was set up initially during the scan. Likewise, the rotation of both bones relative to each other was constantly measurable.
Superimposed images were created for each position containing the most anterior portion of the tibial tuberosity and the deepest part of the trochlear groove as measure points of TT–TG [28].
The TT–TG was measured on the millimetre scale in all positions and then compared for all.
The applied maximal internal and external rotation in full extension and 30° of flexion were quantified in degrees. This strict measurement procedure enabled to collect the TT–TG distance reproducible with a high accuracy.
Statistical analysis
Statistical analysis was performed using a standard statistical software package (JMP version 10, SAS Institute, Cary, USA). A Kolmogorov–Smirnov normality test was performed to verify whether the data met the assumption of a parametric test. The Kolmogorov–Smirnov distance was calculated. Normally and not normally distributed data were compared using paired samples t test and Wilcoxon signed-rank test, respectively.
The measured TT–TG and amount of rotation were correlated. To measure the correlation (linear dependence) between these variables, we used the Pearson correlation coefficient for normally distributed data and Spearman’s rho coefficient for not normally distributed data. A P value of <0.05 was considered to be statistically significant.
Based on the published data [18] on TT–TG, an a priori power calculation was performed (α = 0.05, β = 0.95) which suggested a minimum sample size of 14 individuals.
Results
Knee in extension
The mean TT–TG measured in full extension and neutral rotation was 7.8 mm (Table 1). The mean TT–TG was comparable in both male and female specimens with 7.9 mm (SD 2.3) and 7.7 mm (SD 4.4), respectively (not significant). The correlation between the measured TT–TG and the age of specimens was weak and statistically insignificant.
The mean applied rotation (internal and external together) in full extension was 8.4° (SD 3.3° range 3.0–15.4°), which was statistically significantly lower than values obtained in 30° of flexion (11.8°; SD 4.6° range 4.6–21.6°).
Knee in extension and internal/external rotation
The TT–TG measured in full extension and maximal internal rotation was statistically significantly lower than values obtained in neutral rotation (P < 0.001) (Table 1). The correlation between the amount of internal rotation and decrease in TT–TG distance was very strong and statistically significant (Spearman´s rho 0.940; P < 0.001). The TT–TG measured in specimen in full extension and maximal external rotation was statistically significantly higher than values obtained in neutral rotation (P < 0.001) (Table 1). The correlation between the amount of external rotation and increase in TT–TG was very strong and statistically significant (Pearson correlation r = 0.992; P < 0.001).
Knee in flexion
The mean TT–TG measured in 30° flexion and neutral rotation was 3.9 mm (Table 1), which was statistically significantly lower than values obtained in full extension and neutral rotation (P < 0.001).
Knee in flexion and internal/external rotation
The TT–TG measured in specimen in 30° flexion and maximal internal rotation was statistically significantly lower than values obtained in neutral rotation (P < 0.001) (Table 1). The correlation between the amount of internal rotation and decrease in TT–TG distance was very strong and statistically significant (Pearson correlation r = 0.948; P < 0.001). The TT–TG measured in 30° flexion and maximal external rotation was statistically significantly higher than values obtained in neutral rotation (P < 0.001) (Table. 1). The correlation between the amount of external rotation and increase in the TT–TG was strong and statistically significant (Pearson correlation r = 0.861; P < 0.001).
The mean difference in TT–TG between the highest value in full extension/ER and lowest value in 30° flexion/IR in the same subject was 8.2 mm (SD 3.8, range, 2.1–15.4) (Fig. 3).
Discussion
The most important findings of the present study were:
-
First, flexion decreases the TT–TG distance significantly compared to knee extension.
-
Second, rotation of the femur in relation to the tibia alters the TT–TG significantly.
Patellar instability is a common entity with many different radiographic measures used to assess its severity. In 1978, Goutallier [14] described the TT–TG on normal axial X-rays at 30° of flexion. This is originally based on knee radiographs but is now more commonly measured using computed tomographic (CT) images by superimposing two axial CT slices or scrolling through them (Fig. 1) [22]. A high TT–TG value is thought to indicate lateralization of the tibial tuberosity and is associated with patellar instability [2, 3, 8, 11].
Several studies discuss the excellent reliability and reproducibility of this measurement, but a large variation of norm values is reported [32]. A distance of 20 mm or more is considered to be pathological, and realignment procedures are proposed [8, 32]. The outcome can also be measured postoperatively [5, 11, 19].
However, several papers raise concerns regarding the reliability of the TT–TG measurement and whether patellar instability should be managed based on it [4, 9, 12, 18, 21, 27]. In a healthy study population, a mean TT–TG of 13.6 ± 8.8 mm is considered to be normal [1, 10]. Koëter et al. [19] and Balcarek et al. [2] suggest a threshold distance of 15 mm. Even so, this distance still can be associated with femoro-patellar problems [28]. In Schoettle’s [28] study, 10 out of 12 patients have a history of patellar instability and two an anterior knee pain syndrome with a TT–TG of 14.4 ± 5.4 mm in the CT scan or 13.9 ± 4.5 mm in the MRI. This makes the TT–TG an inconsistent value.
Nevertheless, an unreliable TT–TG measurement caused by different knee angles or internal or external rotation of the tibia during imaging could be responsible for the wide range of inter-individual values and different thresholds in the literature.
Therefore, we hypothesized that different positions of the same knee will deliver different TT–TG measurements.
The tibia is not a cylindrical structure, and screw-home mechanism is well described as the final internal rotation of the femur in extension [15, 20]. Although this mechanism might not play a too important role during walking [17, 26], in passive motion of the knee, it is highly likely to affect the measurement of TT–TG [10, 18]. CT scans for the measurement of the TT–TG are not fully standardized in terms of lower leg positioning, thus making studies difficult to compare. In our study, the TT–TG increased significantly in extension compared to a flexed knee. In some cases, this would imply relevant therapeutic consequences.
The knees rotation increases during flexion up to more than 35° in external and about 25° of internal rotation at 90° of flexion [31]. In presence of a postero-lateral lesion, i.e., hypermobile meniscus, this laxity can increase even more to an instability of 39° in external rotation and/or 40° in internal rotation. [31] However, laxity of the knee is also assumed to decrease with age, i.e., ap-translation in children and adolescent. [13] Therefore, knee rotation can be unpredictable without a concise examination and lead to a false TT–TG result. Our study shows hereby a clear correlation between additional rotation and TT–TG.
Whilst studies clearly show that inter- and intra-reliability of the TT–TG measurement is acceptable, we suggest another variable, namely, the position of the knee whilst scans are taken. This is largely under the control of the patient and thus can dramatically affect the value of the TT–TG measurement obtained. A patient who is having a routine CT scan of the knee and who is fully relaxed may lie with the knee slightly flexed and with an externally rotated tibia relative to the femur due to laxity. The presence of an undiagnosed rotational instability can increase and mimic a pathological TT–TG. On the other hand, a patient who is anxious about having the scan may keep the leg fully extended, engaging screw-home mechanism and thereby also affecting the relative rotation. Positioning of patients for their CT scan is as well probably to vary widely both within, and between different radiology departments and few will have strict guidelines for the knee position in the scanner, tending likely to let the patient lie in as comfortable position for them as possible. Depending on the positioning of knee, differences of up to 15.4 mm in the TT–TG were measured in the same subject in our specimens. As a consequence, a normal TT–TG could be interpreted as pathological and vice versa.
Therefore, a TT–TG measurement without a standardized protocol during image acquisition to control lower leg rotation will not produce reliable and reproducible results.
Most patellar dislocations occur in around 20° of knee flexion and not in fully extended knees [29]. TT–TG is less in 30° of flexion compared to full extension. Therefore, Goutallier [14] proposes that a standardized measurement should probably be done in 30° of knee flexion. Nevertheless, Dejour notes that a measurement in full extension will provide more reliable results than in flexion [7, 8, 25]. In our study, rotation varied more in 30° flexion than in extension. At first sight, this makes a measurement in extension more reliable. In an extended knee, rotation varied less in internal than in external rotation. Therefore, rotation is best controlled in extension an internal rotation. On the other hand, TT–TG varies greater in extension than in flexion. Consequently, our data allow no concise suggestion how to measure TT–TG. However, we believe that controlling rotation is the most important factor thus making the measurement in extension and internal rotation the most reliable one.
Based on these assumptions, a concise standard operating protocol for patient positioning, including foot, is needed for a reliable image acquisition for TT–TG, considering and controlling all possible determining factors. Based on this protocol, new norm values have to be elaborated for further assessments.
This study has limitations. It was performed with formalin-fixed cadavers. The tissues in these tend to be hard and immobile. Despite formalin fixation and restricted guidance, these cadavers showed at least almost a physiological kinematic as described in a previous study [24].
The degree of rotation was not standardized and varied widely amongst the cadavers. Rotational issues are not part of any TT–TG measurement protocol in previous studies. It can be assumed that rotation also varies widely in normal patients.
Creating 3D models out of CT scans and importing them to a visualization software is not a standard procedure for measuring TT–TG. However, this step allowed us to always have comparable variables.
Conclusion
Flexion as well as rotation of the knee joint significantly alters the TT–TG.
These results may have wider clinical relevance in assessing TT–TG and further decisions based on it. Since testing the knee’s ligamentous laxity or instability is part of the clinical evaluation, this information should be taken into account when assessing the TT–TG distance. It may influence decision making regarding realignment procedures.
References
Alemparte J, Ekdahl M, Burnier L, Hernández R, Cardemil A, Cielo R, Danilla S (2007) Patellofemoral evaluation with radiographs and computed tomography scans in 60 knees of asymptomatic subjects. Arthroscopy 23:170–177
Balcarek P, Jung K, Ammon J, Walde TA, Frosch S, Schüttrumpf JP, Stürmer KM, Frosch K-H (2010) Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle–trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med 38:2320–2327
Beaconsfield T, Pintore E, Maffulli N, Petri GJ (1994) Radiological measurements in patellofemoral disorders. A review. Clin Orthop Relat Res 308:18–28
Caplan N, Lees D, Newby M, Ewen A, Jackson R, Gibson ASC, Kader D (2014) Is tibial tuberosity–trochlear groove distance an appropriate measure for the identification of knees with patellar instability? Knee Surg Sports Traumatol Arthrosc 22:2377–2381
Caton JH, Dejour D (2010) Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop 34:305–309
Chouteau J, Testa R, Viste A, Moyen B (2012) Knee rotational laxity and proprioceptive function 2 years after partial ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 20:762–766
Dejour H, Walch G, Neyret P, Adeleine P (1990) Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 76:45–54
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Delgado-Martínez AD, Rodríguez-Merchán EC, Ballesteros R, Luna JD (2000) Reproducibility of patellofemoral CT scan measurements. Int Orthop 24:5–8
Dietrich TJ, Betz M, Pfirrmann CWA, Koch PP, Fucentese SF (2014) End-stage extension of the knee and its influence on tibial tuberosity-trochlear groove distance (TTTG) in asymptomatic volunteers. Knee Surg Sports Traumatol Arthrosc 22:214–218
Diks MJF, Wymenga AB, Anderson PG (2003) Patients with lateral tracking patella have better pain relief following CT-guided tuberosity transfer than patients with unstable patella. Knee Surg Sports Traumatol Arthrosc 11:384–388
Dornacher D, Reichel H, Lippacher S (2014) Measurement of tibial tuberosity-trochlear groove distance: evaluation of inter- and intraobserver correlation dependent on the severity of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:2382–2387
Flynn JM, Mackenzie W, Kolstad K, Sandifer E, Jawad AF, Galinat B (2000) Objective evaluation of knee laxity in children. J Pediatr Orthop 20:259–263
Goutallier D, Bernageau J, Lecudonnec B (1978) The measurement of the tibial tuberosity. Patella groove distanced technique and results (author’s transl). Rev Chir Orthop Reparatrice Appar Mot 64:423–428
Hallen LG, Lindahl O (1966) The “screw-home” movement in the knee-joint. Acta Orthop Scand 37:97–106
Haughom BD, Souza R, Schairer WW, Li X, Ma CB (2012) Evaluating rotational kinematics of the knee in ACL-ruptured and healthy patients using 3.0 Tesla magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 20:663–670
Ishii Y, Terajima K, Terashima S, Koga Y (1997) Three-dimensional kinematics of the human knee with intracortical pin fixation. Clin Orthop Relat Res 343:144–150
Izadpanah K, Weitzel E, Vicari M, Hennig J, Weigel M, Südkamp NP, Niemeyer P (2014) Influence of knee flexion angle and weight bearing on the Tibial Tuberosity-Trochlear Groove (TTTG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc 22:2655–2661
Koëter S, Diks MJF, Anderson PG, Wymenga AB (2007) A modified tibial tubercle osteotomy for patellar maltracking: results at two years. J Bone Joint Surg Br 89:180–185
Last RJ (1950) The popliteus muscle and the lateral meniscus. J Bone Joint Surg Br 32:93–99
Lustig S, Servien E, Selmi TAS, Neyret P (2006) Factors affecting reliability of TT–TG measurements before and after medialization: a CT-scan study. Rev Chir Orthop Reparatrice Appar Mot 92:429–436
Muneta T, Yamamoto H, Ishibashi T, Asahina S, Furuya K (1994) Computerized tomographic analysis of tibial tubercle position in the painful female patellofemoral joint. Am J Sports Med 22:67–71
Myers CA, Torry MR, Shelburne KB, Giphart JE, LaPrade RF, Woo SL-Y, Steadman JR (2012) In vivo tibiofemoral kinematics during 4 functional tasks of increasing demand using biplane fluoroscopy. Am J Sports Med 40:170–178
Nowakowski AM, Kamphausen M, Pagenstert G, Valderrabano V, Müller-Gerbl M (2014) Influence of tibial slope on extension and flexion gaps in total knee arthroplasty: increasing the tibial slope affects both gaps. Int Orthop 38:2071–2077
Pandit S, Frampton C, Stoddart J, Lynskey T (2011) Magnetic resonance imaging assessment of tibial tuberosity–trochlear groove distance: normal values for males and females. Int Orthop 35:1799–1803
Piazza SJ, Cavanagh PR (2000) Measurement of the screw-home motion of the knee is sensitive to errors in axis alignment. J Biomech 33:1029–1034
Saudan M, Fritschy D (2000) AT-TG (anterior tuberosity-trochlear groove): interobserver variability in CT measurements in subjects with patellar instability. Rev Chir Orthop Reparatrice Appar Mot 86:250–255
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CWA, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13:26–31
Senavongse W, Amis AA (2005) The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. J Bone Joint Surg Br 87:577–582
Stäubli HU, Birrer S (1990) The popliteus tendon and its fascicles at the popliteal hiatus: gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy 6:209–220
Suganuma J, Ohkoshi T (2011) Association of internal rotation of the knee joint with recurrent subluxation of the lateral meniscus. Arthroscopy 27:1071–1078
Wilcox JJ, Snow BJ, Aoki SK, Hung M, Burks RT (2012) Does landmark selection affect the reliability of tibial tubercle–trochlear groove measurements using MRI? Clin Orthop Relat Res 470:2253–2260
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Camathias, C., Pagenstert, G., Stutz, U. et al. The effect of knee flexion and rotation on the tibial tuberosity–trochlear groove distance. Knee Surg Sports Traumatol Arthrosc 24, 2811–2817 (2016). https://doi.org/10.1007/s00167-015-3508-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3508-9