Abstract
Purpose
Despite proven accuracy of US for the evaluation of rotator cuff integrity, there is no US-based classification for this purpose. This study aimed to assess US for the evaluation of rotator cuff repair integrity in accordance with a well-established MRI classification.
Methods
The authors retrospectively reviewed 257 patients who underwent arthroscopic double-row suture anchor repair for rotator cuff tears. Post-operative function was rated using the Constant score, the UCLA rating and the SSV, whereas repair integrity was assessed using US as described in the MRI classification of Sugaya et al.
Results
A total of 212 patients aged 55.6 ± 9.8 years had complete functional and radiographic assessments at a mean follow-up of 36.8 ± 11.6 months. Using all three ratings, repairs of Type I had highest scores, repairs of Type II had discernibly lower scores, whereas repairs of Types III, IV and V had similar intermediate scores.
Conclusion
Comparison of the UCLA scores with those of Sugaya et al. revealed similar scores for repairs of Type I and of Type V. The scores are less comparable for repairs of Types II, III and IV, because US does not allow identification of partial tears if shielded by bony structures and because partial tears correspond to minimal impairment. The study reveals that US is an adequate imaging modality to classify rotator cuff repair integrity, which could reduce economic and practical burdens of CTA, MRI or MRA. The results also confirm that post-operative repair integrity and functional outcome depend on pre-operative tear size and fatty infiltration, which provides clinicians with reasoning for early surgical repair and warning of the risks of strenuous activity for patients with larger tears.
Level of evidence
Prognostic study, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arthroscopic repair of rotator cuff tears gained increased popularity over open or mini-open procedures because it reduces incision size, post-operative pain and length of hospital stay [9, 12, 29, 31, 37, 43]. The post-operative integrity of the rotator cuff is influenced—regardless of operative method used—by the pre-operative tear size and the tissue quality [1, 11, 40]. Furthermore, post-operative evaluation of repair integrity seems to have good prognostic value of patient functional outcomes, which are better for patients with intact rotator cuffs following repair [1, 21].
The post-operative integrity of the rotator cuff can be evaluated by ultrasonography (US) [11, 13, 21], computed tomography (CT) arthrography [14], magnetic resonance imaging (MRI) [15, 24, 26, 42] or magnetic resonance arthrography (MRA) [28, 45]. Although recent review articles confirmed the superior accuracy of MRA and CT arthrography over both MRI and US [7, 14, 27], numerous authors demonstrated substantial improvements over the past decade in reliability of US for the assessment of rotator cuff integrity [7, 27, 35, 36, 38], and considerable interest grew in this economic and practical imaging modality [14, 32, 35].
In 2007, Sugaya et al. [41] introduced an MRI-based classification system which gained wide acceptance for the evaluation of post-operative rotator cuff integrity [2, 19, 20, 23, 25, 44] and correlated it with patient functional outcomes. Despite the proven sensitivity and specificity of US for the evaluation of post-operative rotator cuff integrity [7, 14, 27, 32], there is no published US-based classification system for this purpose. The aim of this study was to assess an US-based method for the evaluation of post-operative repair integrity following arthroscopic double-row repair of the rotator cuff, in accordance with the MRI-based classification of Sugaya et al. [41]. The use of US to evaluate rotator cuff repair integrity could reduce economic and practical burdens of CTA, MRI or MRA which deter patients and clinicians from completing necessary post-operative assessments [25].
Materials and methods
Between January 2007 and June 2010, arthroscopic double-row suture anchor repair was performed on 257 patients by the senior author (JB), as a treatment for rotator cuff tear. The aetiology was one tendon tear in 83 patients (14 %), two tendon tears in 138 patients (54 %) and three tendon tears in 36 patients (32 %). The operative technique was consistent throughout this 3-year period; there was no ‘learning curve’ nor new equipment or approaches introduced. All patients had initially received conservative treatment prior to surgery, which proved unsuccessful, including rehabilitation or corticoid infiltration, depending on whether the injury was acute or degenerative. All patients gave informed consent for their participation in the retrospective case-series study. The study was approved by the institutional review board (IRB) at our centre.
All patients were examined pre-operatively, and their rotator cuff muscle quality was assessed on CT or MRI images for fatty infiltration using the modified Goutallier classification [10, 17, 18]. The use of two different imaging modalities for pre-operative assessment could introduce bias, but recent articles indicate that equivalent assessment of fatty infiltration could be achieved using either CT or MRI [3, 10, 22, 30, 33]. Fatty infiltration in stages 0 and 1 was present in 67 patients (26 %), in stage 2 in 156 patients (61 %), in stage 3 in 33 patients (13 %) and in stage 4 in one patient (0.4 %). The case notes for each patient were retrospectively reviewed. The inclusion criteria were: availability of plain radiographs of the affected shoulder, availability of a pre-operative MRI scan or computed tomography (CT) arthrogram, diagnosis of full-thickness rotator cuff tear confirmed intra-operatively and availability of a post-operative US evaluation of the affected shoulder at the latest follow-up. The exclusion criteria were: shoulder joint stiffness, Hamada stage 2 or more (acromiohumeral distance <6 mm) on plain X-rays, concomitant shoulder pathology (such as arthritis, rheumatologic disorders) discovered pre-operatively or arthroscopically, other concomitant severe musculoskeletal pathologies or failure of the patient to be present at the scheduled follow-up visits.
Surgical technique
All patients were operated under general anaesthesia in the beach-chair position. An inter-scalene block was typically performed before surgery, and continuous 3-kg traction of the arm (at the side) was used using a simple traction system fixed on the ipsilateral caudal corner of the table. Four to five arthroscopic portals (on demand) were typically required: posterior soft point and posterolateral portal as viewing portals (scope), and anterior (rotator interval), lateral, posterior and posterolateral as working portals.
We used BioCorkscrew FT bioabsorbable anchors (Arthrex Inc., Naples, FL) with four 5.5 mm × 15 mm NeedlePunch needles and two #2 FiberWires to perform our double-row technique (Fig. 1). All sutures were passed through the tendon using the NeedlePunch suture passer (Arthrex Inc., Naples, FL).
Scope inserted in the posterolateral portal; a biceps tenodesis using a suture anchor high in the groove; b medial row with sutures passed through the supraspinatus using two medial suture anchors; c lateral row is first tightened; d once the lateral row allows perfect reduction, the medial row sutures are tightened; e final construct
First, a biceps tenodesis was performed high in the bicipital groove, if the biceps were still present, just next to the cartilage using the suture anchor with a lasso-loop technique. Subscapularis repair was performed if needed prior to posterior cuff while the scope was in the gleno-humeral joint. The scope was then moved to the subacromial space, which was cleared of adhesions, bursal tissue and reactive synovitis. A subacromial decompression with acromioplasty was performed in the presence of a prominent anterior inferior edge of the acromion, in conjunction with a bony spur on the undersurface of the acromioclavicular joint and the coracoacromial ligament [34]. Acromioclavicular co-planning or distal clavical excision was performed if necessary.
In each shoulder, the pre-operative tear size was assessed during arthroscopic surgery according the Cofield classification [4]: 18 were small (<1 cm in length), 142 were medium (1–3 cm), 40 were large (3–5 cm), and 11 were massive (>5 cm). The tear pattern (U-shaped, L-shaped and C-shaped) and presence of delamination were arthroscopically assessed by means of a tendon grasper, and the repair was based on the tear pattern. Tendon mobility was improved by releasing superficial adhesions between the cuff and the acromial arch. A superior capsular release and rotator interval coracohumeral ligament release were performed when needed to allow a low-tension reduction in the supraspinatus tendon to its anatomical position. A shaver was used for limited debridement of degenerated tendon margins.
After adequate visualization, assessment of the type and mobility of the lesion, preparation and release of the tendon, the upper surface of the greater tuberosity was abraded with caution with a burr, removing all soft tissue and a part of cortical bone, to create a bleeding cancellous bone bed.
Side-to-side sutures were used prior to tendon-to-bone sutures in order to convert L-shaped or U-shaped tears to C-shaped tears. The remaining sutures from the biceps tenodesis were passed through the supraspinatus tendon using a NeedlePunch suturepasser device (Arthrex Inc., Naples, FL). An additional medial anchor was used in case of large tear extending posteriorly just lateral to the cartilage margin. All the sutures from the medial row were passed but tightened at the end of the procedure. The anterolateral portal was used to drill the anchor holes approximately 10 mm distal to the tip of the greater tuberosity. The lateral row was first tightened to reduce the cuff and finally the medial row to increase the coverage of the footprint. Footprint coverage of the rotator cuff was achieved in all cases and confirmed arthroscopically by observing the construct at both subacromial and intra-articular spaces at the end of the procedure. All repairs were ‘watertight’ except for large subscapularis tears which required release including rotator interval debridement.
Evaluation
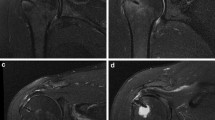
All patients were recalled for physical and radiographic examination at least 1 year post-operatively. The physical examination and collection of functional scores were carried out by a different surgeon (EF) than the one who performed the surgery. The functional scores collected were the Constant score (CS) [5, 6], the University of California at Los Angeles (UCLA) score [8] and the subjective shoulder value (SSV) [15, 16]. The radiographic evaluation was performed using US by an experienced musculoskeletal radiologist (RB) using a 14- to 18-MHz linear transducer and a Xario SSA 660A and SSA probe with precision 660 LG (Toshiba Medical Systems, Otawara, Japan). During the US assessment, the patients were seated with the affected arm maintained free at the side of the trunk. The rotator cuff repair was examined in the three planes (axial, sagittal and coronal). The tendons of the supraspinatus and infraspinatus were examined with the arm in adduction and internal rotation, while the subscapularis was evaluated in external rotation. The integrity of the repaired rotator cuff was classified into five types, as described by Sugaya et al. [40, 41], based on frontal, sagittal and transverse US images only (Fig. 2):
Integrity of the repaired rotator cuff classified into five types using ultrasonography; a Type I indicated a repaired cuff with sufficient thickness (>2 mm) and normal echostructure as normal tendon hyperechoic and fibrillar on each image; b Type II indicated a repaired cuff that had sufficient thickness (>2 mm) associated with a partial hypo-echogenicity or heterogenicity; c Type III indicated a repaired cuff that had insufficient thickness (<2 mm) without discontinuity; d Type IV indicated the presence of a minor full-thickness discontinuity of which border are well visible, suggesting to a small tear; e Type V indicated the presence of a major discontinuity of which the medial border is not visible under the acromial arch, suggesting a medium or large tear
-
Type I indicated a repaired cuff that had sufficient thickness (>2 mm) with normal echostructure as normal tendon hyperechoic and fibrillar on each image;
-
Type II indicated a repaired cuff that had sufficient thickness (>2 mm) associated with a partial hypo-echogenicity or heterogenicity;
-
Type III indicated a repaired cuff that had insufficient thickness (<2 mm) without discontinuity;
-
Type IV indicated the presence of a minor full-thickness discontinuity of which border are well visible, suggesting to a small tear;
-
Type V indicated the presence of a major discontinuity of which the medial border is not visible under the acromial arch, suggesting a medium or large tear.
The use of patient data for this study was approved by the institutional review board (IRB) at our centre (Centre Osteo-Articulaire des Cèdres, Ref: Study 2007-01).
Statistical analysis
Statistical analyses were performed using SAS/STAT (SAS Institute Inc., North Carolina, USA). The Mann–Whitney U test was used to compare the difference between the pre-operative and post-operative functional outcomes (Constant score, UCLA and SSV). One-factor analysis of variance was used to compare the repair integrity and the functional scores. To enable calculation of a p value for each repair type (using Type I as the reference), we used a nonparametric one-way analysis of rank scores (generalized linear model on ranked data, including Bonferroni multiple comparisons). The level of statistical significance was therefore set at p = 0.0125 (0.05/4).
Results
Of the initial 257 patients, 41 failed to be present for follow-up at 12 or more months, three patients were excluded because they had subsequent surgery on another joint (knee, hip or spine) and one patient died before the end of the follow-up period from unrelated causes. The remaining 212 patients (82.5 %) (113 men and 99 women) were available for evaluation at a mean follow-up of 36.8 (range 16–61) months. The mean age at surgery was 55.6 (range 16–83) years, and arthroscopy revealed one tendon tear in 71 patients (37 %), two tendon tears in 114 patients (54 %), and three tendon tears in 27 patients (13 %). Forty-one (19 %) of the patients were smokers, and six (3 %) were diabetic.
Functional outcomes
All three rating systems reflected a significant improvement in the status of the shoulders when the pre-operative scores were compared with the post-operative scores (p < 0.01) (Table 1). The mean Constant score had increased from 56.3 points (median 57; range 8–92) pre-operatively to 80.0 points (median 83; range 42–100) post-operatively. The mean UCLA score had increased from 14.4 points (median 14; range 2–26) pre-operatively to 31.1 points (median 32; range 11–35) post-operatively. The SSV score was not available pre-operatively, but the mean was 79.7 (median 85; range 0–100) post-operatively.
Repair integrity
Ultrasound imaging revealed 75 shoulders (35 %) with a Type I repair, 99 shoulders (47 %) with a Type II repair, 11 shoulders (5 %) with a Type III repair, 12 shoulders (6 %) with a Type IV repair and 15 (7 %) with a Type V repair. The overall rate of re-tears (Types IV and V) was 13 % (27 shoulders) (Table 2). Using all three rating systems (Table 2), Type I repairs had the highest scores (p < 0.01), and Type II repairs had discernibly lower scores. Neither diabetes nor smoking had any effect on functional outcomes or repair integrity.
Pre-operative fatty infiltration and tear size
The functional scores declined significantly with the increase in pre-operative fatty infiltration, but were not related to pre-operative tear size (Fig. 3). Shoulders with little or no fatty infiltration (stages 0 and 1) had significantly higher functional scores than shoulders with moderate to high fatty infiltration (stages 2–4), using all three rating systems (Table 3). Post-operatively, poor repairs (Types IV and V) were more frequent for large and massive pre-operative tears (25.5 %) than for small and medium pre-operative tears (8.8 %) (Table 4).
Discussion
The most important finding of the present study was that US is a valid imaging modality for post-operative evaluation of rotator cuff repair integrity following the MRI-based classification of Sugaya et al. [41]. The repair integrity in this study compared favourably with that reported for open or mini-open [15, 21] and arthroscopic single-row repair [1, 11, 40]. Comparison of UCLA ratings from this study with those of Sugaya et al. [41] reveals equivalent improvement in post-operative scores compared to pre-operative scores (Table 5).
The three rating systems used in this study (Constant score, UCLA and SSV) indicated significantly higher functional outcomes for repairs of Type I than for all other repair types; the scoring system that correlated best with repair type was the Constant score, which indicated notably poor functional outcomes for repairs of Type V (68.7) than for repairs of Types II, III and IV (80.2, 71.1 and 71.0, respectively). Our observations are in contrast with those of Sugaya et al. [41] who found that the three rating systems used (JOA, UCLA and ASES) indicated significantly lower functional outcomes for repairs of Type V than for all other repair types; the scoring system that correlated best with repair type was the Japanese Orthopaedic Association (JOA) rating, which indicated somewhat higher functional outcomes for repairs of Types I and II (96.5 and 96.4, respectively) than for repairs of Types III and IV (94.3 and 94.8, respectively). Overall, post-operative US classification of rotator cuff integrity has some prognostic value, as asserted in recent studies [23, 25], which enables the clinician to predict post-operative shoulder function and thus inform the patient (especially in heavy workers or demanding individuals) of what subjective function to expect, based on objective radiographic examination (Fig. 4).
Post-operative repair integrity as a function of pre-operative tear size (Cofield [4])
Direct comparison of UCLA scores from this study with those of Sugaya et al. (Table 6) reveals nearly identical UCLA scores for repairs of Type I in both studies and for repairs of Type V in both studies. The scores are less comparable for ‘imperfect’ repairs of Types II, III and IV, and this could have two explanations. First, US does not allow perfect distinction between those three repairs types—despite the superior spatial resolution of US over MRI for small ruptures—because partial tears (Type IV) may not be visible if they are shielded by bony structures. Second, the borders between a pathologic tendon (e.g. tendinopathy or Type II) versus partial tear (e.g. weak tendon or Type III) versus tiny tears (e.g. minor discontinuity or Type IV) are clinically and functionally not discernible. Pain relief in those cases is mostly incomplete compared to Type I, whereas strength recovery is still better achieved compared to Type V (extended discontinuity or larger re-tear).
Direct comparison of diagnostic data with clinical outcomes reveals that (1) post-operative functional scores are influenced by pre-operative fatty infiltration and (2) post-operative repair integrity could be related to pre-operative tear size. Shoulders with little or no fatty infiltration (stages 0 and 1) had considerably higher functional scores than shoulders with moderate to high fatty infiltration (stages 2–4), and this difference was statistically significant, using all three rating systems (Table 3). Post-operatively, poor repairs (Types IV and V) were more frequent for large and massive pre-operative tears (25.5 %), than for small and medium pre-operative tears (8.8 %) (Table 4). These observations could have two implications in clinical practice: First, they advocate the benefits of repairing torn rotator cuffs sooner rather than later, to prevent fatty infiltration which could worsen surgical and functional outcomes; second, they help manage the expectations of demanding patients, by informing them that larger tears are more predisposed to re-tear. Surgeons should therefore advise demanding patients to avoid strenuous physical activity (sports or labour) post-operatively in case of large or massive tears pre-operatively. Surgeons could also warn patients that their shoulder function post-operatively may be compromised if they had high levels of fatty infiltration pre-operatively (Table 7).
A number of recent studies reported little or no improvement in repair integrity with enhanced surgical techniques, implant materials or biologic agents: Gumina et al. [19] reported that the use of platelet–leucocyte membranes in the treatment of rotator cuff tears improved repair integrity but had little effect on functional outcomes. Boyer et al. [2] observed a slight decrease in re-tear rate using a knotless tape-bridging construct versus a standard tied suture-bridging technique. Werthel et al. [44] found no improvement in repair integrity nor functional outcomes using adjuvant intra-tendinous injections of autologous conditioned plasma. This study also confirms previous findings that both tendon and fatty infiltration of the muscle may influence on functional outcome and repair integrity following rotator cuff repair [10, 17, 18, 23, 25, 30].
The main strengths of this study are (1) its relatively large sample size (212 patients) and (2) long follow-up (36.6 months) that enabled robust statistical analyses and rendered some conclusions. The study has several limitations typical of a retrospective analysis, including (1) the wide variability of follow-up (16–61 months) which could alter clinical and functional observations, (2) the inclusion of patients with various sizes of subscapularis tears which may have impact on the prognosis of repair integrity, (3) the use of two different imaging modalities (CT and MRI) to assess muscle quality and fatty infiltration, (4) the inability to analyse the inter- and intra-observer accuracy because US is a dynamic imaging modality and its interpretation must be done in the presence of the patient [14] and (5) the lack of post-operative MRI scans that would permit much more direct evaluation of sensitivity and specificity of the US evaluations. It would not have been feasible to retain or recall the patients for additional radiographic examinations by the same observer or by a different radiologist. To compensate for this limitation, we performed the study on a large cohort and followed the well-established classification of Sugaya et al. [41]. In comparison with the studies in the literature that evaluated US for tendon healing assessment, this study is the most detailed and the closest to the classification of Sugaya et al. [41]. Indeed, most articles that used US to assess tendon healing previously evaluated grossly the repair such as ‘torn’ or ‘healed’ [7, 14]. The drawbacks of US compared to the other imaging still remains in fatty infiltration evaluation or cartilage wear [39] and it thus insufficient to explain all causes of pain in cases of post-operative failures, which are well addressed by the other imaging system.
Conclusions
The present study reveals similar findings to those of Sugaya et al. [41] and confirms that US is a valid imaging modality as MRI [7, 14], for the evaluation of post-operative repair integrity following arthroscopic double-row repair of the rotator cuff. The use of US to evaluate rotator cuff repair integrity could reduce the economic and practical burdens of post-operative radiographic evaluation which deter patients and clinicians from completing necessary post-operative assessments [21] as they require more expensive equipment and involve longer waiting lists and examination times. The study also confirms that post-operative repair integrity and function depend on pre-operative tear size and fatty infiltration, which provides patients and clinicians with reasoning for early surgical repair and warning of the risks of strenuous activity for patients with larger tears. Further studies are required to evaluate the sensitivity and specificity of US for this purpose.
References
Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG (2005) Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J Bone Joint Surg Am 87(6):1229–1240
Boyer P, Bouthors C, Delcourt T, Stewart O, Hamida F, Mylle G, Massin P (2013) Arthroscopic double-row cuff repair with suture-bridging: a structural and functional comparison of two techniques. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2401-7
Charousset C, Bellaiche L, Duranthon LD, Grimberg J (2005) Accuracy of CT arthrography in the assessment of tears of the rotator cuff. J Bone Joint Surg Br 87(6):824–828
Cofield RH (1982) Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet 154(5):667–672
Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F, Boileau P (2008) A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg 17(2):355–361
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214(214):160–164
de Jesus JO, Parker L, Frangos AJ, Nazarian LN (2009) Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. Am J Roentgenol 192(6):1701–1707
Ellman H, Hanker G, Bayer M (1986) Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am 68(8):1136–1144
Fealy S, Kingham TP, Altchek DW (2002) Mini-open rotator cuff repair using a two-row fixation technique: outcomes analysis in patients with small, moderate, and large rotator cuff tears. Arthroscopy 18(6):665–670
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 8(6):599–605
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K (2004) The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 86(2):219–224
Gartsman GM (2001) Arthroscopic rotator cuff repair. Clin Orthop Relat Res 390(390):95–106
Gazielly DF, Gleyze P, Montagnon C (1994) Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res 304:43–53
Gazzola S, Bleakney RR (2011) Current imaging of the rotator cuff. Sports Med Arthrosc Rev 19(3):300–309
Gerber C, Fuchs B, Hodler J (2000) The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 82(4):505–515
Gilbart MK, Gerber C (2007) Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg 16(6):717–721
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 304(304):78–83
Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S (2003) Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 12(6):550–554
Gumina S, Campagna V, Ferrazza G, Giannicola G, Fratalocchi F, Milani A, Postacchini F (2012) Use of platelet–leukocyte membrane in arthroscopic repair of large rotator cuff tears: a prospective randomized study. J Bone Joint Surg Am 94(15):1345–1352
Haneveld H, Hug K, Diederichs G, Scheibel M, Gerhardt C (2013) Arthroscopic double-row repair of the rotator cuff: a comparison of bio-absorbable and non-resorbable anchors regarding osseous reaction. Knee Surg Sports Traumatol Arthrosc 21(7):1647–1654
Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA (1991) Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 73(7):982–989
Imhoff AB, Hodler J (1996) Correlation of MR imaging, CT arthrography, and arthroscopy of the shoulder. Bull Hosp Joint Dis 54(3):146–152
Jo CH, Shin JS (2013) Cross-sectional area of the supraspinatus muscle after rotator cuff repair: an anatomic measure of outcome. J Bone Joint Surg Am 95(19):1785–1791
Jost B, Pfirrmann CW, Gerber C, Switzerland Z (2000) Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am 82(3):304–314
Kim JH, Hong IT, Ryu KJ, Bong ST, Lee YS, Kim JH (2014) Retear rate in the late postoperative period after arthroscopic rotator cuff repair. Am J Sports Med 42(11):2606–2613
Knudsen HB, Gelineck J, Sojbjerg JO, Olsen BS, Johannsen HV, Sneppen O (1999) Functional and magnetic resonance imaging evaluation after single-tendon rotator cuff reconstruction. J Shoulder Elbow Surg 8(3):242–246
Lenza M, Buchbinder R, Takwoingi Y, Johnston R, Hanchard N, Faloppa F (2013) Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev 9:1–139
Liu SH, Baker CL (1994) Arthroscopically assisted rotator cuff repair: correlation of functional results with integrity of the cuff. Arthroscopy 10(1):54–60
Lo IKY, Burkhart SS (2003) Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy 19(9):1035–1042
Melis B, DeFranco MJ, Chuinard C, Walch G (2010) Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Clin Orthop Relat Res 468(6):1498–1505
Millstein ES, Snyder SJ (2003) Arthroscopic evaluation and management of rotator cuff tears. Orthop Clin N Am 34(4):507–520
Murphy RJ, Daines MT, Carr AJ, Rees JL (2013) An independent learning method for orthopaedic surgeons performing shoulder ultrasound to identify full-thickness tears of the rotator cuff. J Bone Joint Surg Am 95(3):266–272
Oh JH, Kim JY, Choi JA, Kim WS (2010) Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: comparison with magnetic resonance imaging with arthroscopic correlation. J Shoulder Elbow Surg 19(1):14–20
Park TS, Park DW, Kim SI, Kweon TH (2001) Roentgenographic assessment of acromial morphology using supraspinatus outlet radiographs. Arthroscopy 17(5):496–501
Pavic R, Margetic P, Bensic M, Brnadic RL (2013) Diagnostic value of US, MR and MR arthrography in shoulder instability. Injury 44(Suppl 3):S26–S32
Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K (2003) Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am 85(6):1084–1089
Severud EL, Ruotolo C, Abbott DD, Nottage WM (2003) All-arthroscopic versus mini-open rotator cuff repair: a long-term retrospective outcome comparison. Arthroscopy 19(3):234–238
Smith TO, Back T, Toms AP, Hing CB (2011) Diagnostic accuracy of ultrasound for rotator cuff tears in adults: a systematic review and meta-analysis. Clin Radiol 66(11):1036–1048
Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M (2005) Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology 237(2):584–589
Sugaya H, Maeda K, Matsuki K, Moriishi J (2005) Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy 21(11):1307–1316
Sugaya H, Maeda K, Matsuki K, Moriishi J (2007) Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 89(5):953–960
Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F (1997) Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res 344:275–283
Waltrip RL, Zheng N, Dugas JR, Andrews JR (2003) Rotator cuff repair. A biomechanical comparison of three techniques. Am J Sports Med 31(4):493–497
Werthel JD, Pelissier A, Massin P, Boyer P, Valenti P (2014) Arthroscopic double row cuff repair with suture-bridging and autologous conditioned plasma injection: functional and structural results. Int J Shoulder Surg 8(4):101–106
Worland RL, Arredondo J, Angles F, Lopez-Jimenez F (1999) Repair of massive rotator cuff tears in patients older than 70 years. J Shoulder Elbow Surg 8(1):26–30
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barth, J., Fotiadis, E., Barthelemy, R. et al. Ultrasonic evaluation of the repair integrity can predict functional outcomes after arthroscopic double-row rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 23, 376–385 (2015). https://doi.org/10.1007/s00167-015-3505-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3505-z