Abstract
Purpose
To determine whether the bathing of an anterior cruciate ligament (ACL) autograft in vancomycin reduces the rate of infection following an ACL reconstruction.
Methods
Retrospective analysis of all ACL reconstructions over an 8-year period in two University Hospitals. In the initial 4-year period, all patients were operated on under classical antibiotic intravenous prophylaxis (group 1). Over the last 4-year period, this prophylaxis was supplemented with presoaking of the autograft (group 2). Presoaking was performed with sterile gauze previously saturated with a vancomycin solution (5 mg/ml).
Results
There were 810 and 734 patients in group 1 and 2, respectively. Fifteen cases of knee joint infections were identified in the series (0.97 %). All of these infections occurred in group 1, representing a rate of infection of 1.85 % in comparison with 0 % in group 2 (p < 0.001).
Conclusions
Autograft presoaking with vancomycin in combination with classical intravenous antibiotic prophylaxis reduced the rate of knee joint infection following an ACLR in comparison with antibiotic prophylaxis alone. This technique could be of relevance in daily clinical practice to prevent infection after ACLR.
Level of evidence
Case control study, retrospective comparative study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Septic arthritis following an anterior cruciate ligament reconstruction (ACLR) is a serious but uncommon complication, with the incidence rate ranging from 0.14 to 1.8 % [6, 14, 16]. A hamstring autograft [4, 12, 15], concomitant open surgical procedures [20], the use of drains [26] or previous surgery on the same knee [3, 12, 19] have been related to a higher risk of suffering a knee joint infection after an ACLR.
Staphylococci are the most important causative agents in up to 90 % of cases. Approximately half of those are due to coagulase-negative staphylococci (CNS) [6, 13, 15, 20, 21, 23, 26]. Other pathogens reported are Propionibacterium acnes and Enterobacter species [6]. Some authors have linked this high percentage of CNS to the graft harvest and its contamination with patients’ skin bacteria [6].
The use of a preoperative prophylactic antibiotic [24] as well as a proper hair removal, in the cases which needed it [22], has demonstrated efficiency in reducing the rate of infection in orthopaedic procedures. Recently, autograft presoaking with vancomycin has been described as showing promising results in decreasing the rate of infection following an ACLR [25], although they only used hamstrings grafts in the study.
In a study published by Torres-Claramunt [23], the rate of infection in the patients operated on for an ACLR was assessed. This rate (1.8 %) was higher than initially expected. Therefore, presoaking of the autograft with vancomycin was introduced as a new prophylactic measure in the ACLR in order to reduce this rate of infection.
The purpose of this study was to find out whether the implementation of prophylactic graft saturation with vancomycin reduces the rate of infection following an ACLR, using either hamstrings or bone–patellar tendon–bone (BPTB) grafts. The initial hypothesis was that prophylactic autograft presoaking in vancomycin along with a prophylactic intravenous (IV) antibiotic reduces the incidence of infection after ACLR.
Materials and methods
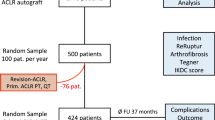
A retrospective review of all the patients that consecutively underwent primary arthroscopic ACLR with an autograft in two University Hospitals was performed. Those patients who needed an extra-articular procedure or those who received an allograft were not included in the study. In the initial 4-year period, the patients received preoperative IV antibiotics (group 1). In the following 4-year period, the patients received preoperative IV antibiotics and, furthermore, the graft was presoaked in a vancomycin solution (group 2).
Surgical technique
All patients were operated on by the same surgical team composed of four senior surgeons. All operations were performed on an outpatient basis. The prophylactic antibiotic protocol consisted in a single dose of 2 g of preoperative IV cefazolin or a single dose of 1 g of preoperative IV vancomycin, if a penicillin allergy was reported [24]. No patient in this series informed of a vancomycin allergy. The types of graft employed were a quadrupled hamstrings and a BPTB. A pretension of 80 N was applied for 5 min before fixation of the hamstrings grafts. BPTB grafts were fixed using a resorbable interference screw in both sides. The hamstring grafts femoral fixation was carried out either with a transversal fixation (Cross-Pin system®, Stryker, Kalamazoo, MI, USA) or with a cortical suspensory fixation system (XO Button Fixation System®, ConMed Linvatec, Largo, FL, USA). Tibial fixation was accomplished with a resorbable interference screw. No drains were left after surgery.
The technique of vancomycin saturation has been performed as previously described by Grayson et al. [10]. A solution of 100 ml of sterile saline was prepared in a tray and mixed with 500 mg of vancomycin powder. When the graft was obtained and prepared, it was immersed in the tray and then it was wrapped in gauze that had been saturated with this vancomycin solution beforehand. The graft was left there for 10–15 min (until it was used for the ACL reconstruction).
Diagnostic criteria for septic arthritis
Diagnosis of septic arthritis was based on patients’ anamnesis and physical examination, laboratory parameters and cultures of synovial fluid and/or joint tissue. Synovial aspiration was performed as soon as the diagnosis was suspected. The liquid obtained was immediately sent for biochemical analysis and cell count analysis in heparin tubes. The remaining synovial fluid was introduced into aerobic and anaerobic blood culture bottles for automatic colorimetric bacterial detection (BacT/ALERT® Culture Media, BioMérieux, France). These bottles contain activated charcoal to neutralise antimicrobials and make for a more accurate diagnosis. They also make it possible to perform an antibiotic sensitivity test.
Statistical analysis
Categorical variables were presented as means and range as percentages. When two related items of data were analysed, the Chi-square or Fisher exact test was used. In all cases, a p value of <0.05 was considered statistically significant. A power analysis was performed to ensure an adequate sample size for the study. Selecting an incidence of infection of 1 %, a significance level (α) of 0.05 and a power (β) of 80 %, the sample size needed was 119 patients in each group. The statistical analysis was done using SPSS 18.0 (SPSS Inc., Chicago, IL) statistical package.
Results
There were 1,544 patients who met the inclusion criteria. The first 810 were included in group 1, and the following 734 were included in group 2. Both groups were similar in terms of age, sex and BMI (n.s.).
Surgical data
The type of graft employed was a quadrupled hamstring in 84 % of the cases and BPTB in 16 % of cases. BPTB grafts were fixed using a resorbable interference screw in both sides, in all cases. The Biosteon® screw (Stryker, Kalamazoo, MI, USA) was used in the first 151 BPTB cases, and the GENESYS™ Matryx® Interference Screw (ConMed Linvatec, Largo, FL, USA) was employed in the last 96 cases. In the first 607 cases of hamstring grafts, the femoral fixation was carried out with the Cross-Pin system® (Stryker) and with a resorbable interference screw (Biosteon®, Stryker Endoscopy, USA) for the tibial fixation. In the succeeding 690 cases of hamstrings graft, the graft was fixed at the femoral side using the XO Button Fixation System® (ConMed Linvatec), while a resorbable GENESYS™ Matryx® Interference Screw (ConMed Linvatec) was used for tibial fixation.
Infection cases analysis
There was an overall infection rate of 0.97 % (15 cases) after ACLR. All cases were acute infections that developed in the early post-operative period (1–5 weeks after surgery).
All 15 infections occurred in group 1 (only IV antibiotic prophylaxis without vancomycin saturation of the graft), which represents a rate of 1.85 % of infection (15 out of 810). Within this group of patients that developed an infection, a partial meniscectomy was performed in two cases and a bucket-handle tear of the medial meniscus was sutured in another patient. The bacteria isolated were as follows: 12 Staphylococcus species (80 %) of which 9 were CNS (60 %) and 3 Staphylococcus aureus (20 %); there was an infection due to Propionibacterium acnes and one culture-negative infection. One of the patients needed graft removal and a 2-stage ACLR procedure because of treatment failure after the third arthroscopic debridement and lavage.
There was no infection among patients who received systemic antibiotic prophylaxis and graft presoaking with vancomycin (group 2). This represented a rate of infection of 0 % (0 out of 734).
Statistical analysis showed that the prior saturation of the ACL graft in a vancomycin solution significantly reduced the infection rate (p < 0.001) in comparison with patients in which this technique was not performed.
Discussion
The main finding of this study was that the use of local vancomycin (presoaking of the autograft) in combination with prophylactic IV antibiotic reduced the ACLR infection rate compared with prophylactic IV antibiotics alone. The reduction in the infection rate occurred in both hamstring and BPTB groups. Based on these findings, the hypothesis was confirmed and supports the results obtained by Vertullo et al. [25].
Although knee joint infection following an ACLR is not as common as other implant-associated infections in orthopaedic surgery, the magnitude of this complication is equally important as an inadequate treatment could compromise joint function [2, 5, 23]. For this reason, different studies have been focused on the surgical management of this complication over recent years. Most of those studies concluded that aggressive arthroscopic debridement in combination with an antibiotic therapy should be the treatment of choice for this complication [1, 6, 12, 16, 21, 23]. Despite this, antibiotic treatment guidelines remain unclear.
Little has been reported about the prevention of a septic arthritis following an ACLR. Some proceedings such as antibiotic prophylaxis or limiting hair removal to the cases needing it, which are usually applied so as to avoid this complication, have been imported from other orthopaedic procedures (basically joint replacement procedures) [22, 24]. Grayson et al. [10] studied the amount of vancomycin released from the pre-soaked bovine tendons. They observed that tendons elute vancomycin into the environment in which they were placed and where they act as a reservoir of vancomycin. Furthermore, tendons with larger dimensions provide a greater reservoir. This technique was posteriorly applied in an in vivo study by them. It showed an important decrease of the rate of joint infection following an ACLR when this prophylactic measure was included in the surgical protocol [25]. Interestingly, their results were comparable to the findings observed in the present investigation.
Vancomycin is a useful bactericidal drug against staphylococci and enterococci [24] and has been described as an alternative in the treatment of Propionibacterium acnes implant-associated infections [18]. Vancomycin has shown to be safe for a local use [11], and it has already been used in both local prophylaxis and treatment in orthopaedics. For instance, it has been utilised with antibiotic-loaded cement spacers or nails [27], bioactive glasses or composite biomaterials [11]. Furthermore, it is a thermostable antibiotic and less toxic to eukaryotic cells than cefazolin or aminoglycosides [7]. The minimal vancomycin concentration to eradicate most of Staphylococcus infections is about 2 µg/ml. Grayson et al. [10] showed that this concentration can be maintained for at least 24 h when a tendon has been previously presoaked with vancomycin and this same elution was lower than the reported osteoblast and chondroblast toxicity concentrations [7].
Different studies have demonstrated that the infection rate using hamstrings autograft is higher than when using BPTB autograft [4, 15]. In the current study, the percentage of hamstring autografts used was superior in the group where the graft was presoaked. However, the infection rate was 0 % in this group. This suggests that graft presoaking with vancomycin reduces the infection rate following an ACLR despite the graft selected.
Contamination of the graft can occur during harvest or even when it is introduced into the knee through the arthroscopic portals [6]. This might explain why the infection rate in hamstring autografts is higher [15] and mostly due to CNS (patient’s skin flora around the portal). Plante et al. [17] found contamination in 23 % of hamstring autografts. Moreover, the fact that the steeping of the graft in vancomycin reduces the infection rate would give support to this theory, even though specific microbiological studies are needed to confirm this hypothesis.
Different limitations can be attributed to this study. First of all, it had a retrospective design with a lack of randomization. On the other hand, the fact that some steps in the surgical technique changed during the studied period might be considered another bias. The location of the femoral tunnel moved from an almost over the top position to an anatomical location in recent years, and the fixation by means of a transversal fixation has been replaced by a cortical suspensory system. This change was made because a cortical suspensory fixation system has been shown to be safer when an anatomical femoral tunnel placement is being performed [8, 9]. Regardless this variation in the fixation system in the femur, no data suggested that the decrease in the rate of infection after ACLR could be attributed to the change of fixation.
Despite these limitations, the present technique will be of relevance in daily clinical practice to prevent infection after ACLR.
Conclusions
Autograft presoaking with vancomycin in combination with classical intravenous antibiotic prophylaxis reduces the rate of knee joint infection following an ACLR in comparison with antibiotic prophylaxis alone.
References
Abdel-Aziz A, Radwan YA, Rizk A (2013) Multiple arthroscopic debridement and graft retention in septic knee arthritis after ACL reconstruction: a prospective case-control study. Int Orthop 38(1):73–82
Ardern CL, Webster KE, Taylor NF, Feller JA (2011) Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med 45(7):596–606
Armstrong RW, Bolding F, Joseph R (1992) Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy 8(2):213–223
Barker JU, Drakos MC, Maak TG, Warren RF, Williams RJ 3rd, Allen AA (2009) Effect of graft selection on the incidence of postoperative infection in anterior cruciate ligament reconstruction. Am J Sports Med 38(2):281–286
Bostrom, Windhamre H, Mikkelsen C, Forssblad M, Willberg L (2014) Postoperative septic arthritis after anterior cruciate ligament reconstruction: does it affect the outcome? A retrospective controlled study. Arthroscopy. doi:10.1016/j.arthro.2014.03.019
Cadet ER, Makhni EC, Mehran N, Schulz BM (2013) Management of septic arthritis following anterior cruciate ligament reconstruction: a review of current practices and recommendations. J Am Acad Orthop Surg 21(11):647–656
Edin ML, Miclau T, Lester GE, Lindsey RW, Dahners LE (1996) Effect of cefazolin and vancomycin on osteoblasts in vitro. Clin Orthop Relat Res 333:245–251
Gelber PE, Reina F, Torres R, Monllau JC (2010) Effect of femoral tunnel length on the safety of anterior cruciate ligament graft fixation using cross-pin technique: a cadaveric study. Am J Sports Med 38(9):1877–1884
Gelber PE, Reina F, Torres R, Monllau JC (2010) Effect of femoral tunnel length on the safety of anterior cruciate ligament graft fixation using cross-pin technique: a cadaveric study. Am J Sports Med 38(9):1877–1884
Grayson JE, Grant GD, Dukie S, Vertullo CJ (2011) The in vitro elution characteristics of vancomycin from tendons. Clin Orthop Relat Res 469(10):2948–2952
Hanssen AD (2005) Local antibiotic delivery vehicles in the treatment of musculoskeletal infection. Clin Orthop Relat Res 437:91–96
Judd D, Bottoni C, Kim D, Burke M, Hooker S (2006) Infections following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy 22(4):375–384
Kim YM, Joo YB (2012) Clinical presentation of staphylococcus epidermidis septic arthritis following anterior cruciate ligament reconstruction. Knee Surg Relat Res 24(1):46–51
Lind M, Menhert F, Pedersen AB (2009) The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc 17(2):117–124
Maletis GB, Inacio MC, Reynolds S, Desmond JL, Maletis MM, Funahashi TT (2013) Incidence of postoperative anterior cruciate ligament reconstruction infections: graft choice makes a difference. Am J Sports Med 41(8):1780–1785
Mouzopoulos G, Fotopoulos VC, Tzurbakis M (2009) Septic knee arthritis following ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 17(9):1033–1042
Plante MJ, Li X, Scully G, Brown MA, Busconi BD, DeAngelis NA (2013) Evaluation of sterilization methods following contamination of hamstring autograft during anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21(3):696–701
Portillo ME, Corvec S, Borens O, Trampuz A (2013) Propionibacterium acnes: an underestimated pathogen in implant-associated infections. Biomed Res Int 2013:804391
Schollin-Borg M, Michaelsson K, Rahme H (2003) Presentation, outcome, and cause of septic arthritis after anterior cruciate ligament reconstruction: a case control study. Arthroscopy 19(9):941–947
Sonnery-Cottet B, Archbold P, Zayni R, Bortolletto J, Thaunat M, Prost T, Padua VB, Chambat P (2011) Prevalence of septic arthritis after anterior cruciate ligament reconstruction among professional athletes. Am J Sports Med 39(11):2371–2376
Sonnery-Cottet B, Thaunat M, Archbold P, Issartel B, Cadet ER (2014) Management of septic arthritis following anterior cruciate ligament reconstruction: a review of current practices and recommendations. J Am Acad Orthop Surg 22(5):271–273
Tanner J, Norrie P, Melen K (2011) Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev 9(11):CD004122
Torres-Claramunt R, Pelfort X, Erquicia J, Gil-Gonzalez S, Gelber PE, Puig L, Monllau JC (2012) Knee joint infection after ACL reconstruction: prevalence, management and functional outcomes. Knee Surg Sports Traumatol Arthrosc 21(12):2844–2849
Trampuz A, Zimmerli W (2006) Antimicrobial agents in orthopaedic surgery: prophylaxis and treatment. Drugs 66(8):1089–1105
Vertullo CJ, Quick M, Jones A, Grayson JE (2013) A surgical technique using presoaked vancomycin hamstring grafts to decrease the risk of infection after anterior cruciate ligament reconstruction. Arthroscopy 28(3):337–342
Wang C, Lee YH, Siebold R (2014) Recommendations for the management of septic arthritis after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 22(9):2136–2144
Wasko MK, Borens O (2013) Antibiotic cement nail for the treatment of posttraumatic intramedullary infections of the tibia: midterm results in 10 cases. Injury 44(8):1057–1060
Acknowledgments
We would like to thank Mr. Eric L. Goode for his help with the English correction. We are also grateful to Prof Andrej Trampuz for his suggestions in the microbiological and infectious diseases field.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pérez-Prieto, D., Torres-Claramunt, R., Gelber, P.E. et al. Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 24, 2724–2728 (2016). https://doi.org/10.1007/s00167-014-3438-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3438-y