Abstract
Purpose
Reconstruction of the anterior cruciate ligament (ACL) remains a major concern in the prepubescent, skeletally immature patient with wide open growth plates. Different surgical techniques have been proposed. This study reports the results and complications of ACL reconstruction in young children using an all epiphyseal technique.
Methods
Between 2006 and 2010, 12 patients (10–13 years, median 12.1 years) underwent epiphyseal primary ACL reconstruction, with a total of 13 knee procedures. Patients were assessed retrospectively with a median follow-up of 54 months (range 39–80 months) consisting of a clinical examination, instrumented arthrometer testing and radiological analysis. Functional status was assessed using the Lysholm knee score, Tegner activity scale and IKDC-2000 form.
Results
According to the IKDC examination form, five knees were rated as normal, six near normal and two abnormal. The median IKDC score at follow-up was 88.5 points (range 75–99 points). The mean side–to-side difference in KT-1000 ligament laxity testing was 1.5 mm (±2.5 mm). In two patients, reoperation was necessary due to graft failure. Two patients developed significant leg length inequality; one with 20 mm overgrowth and varus malalignment after re-reconstruction and the second developed arthrofibrosis and overgrowth of 16 mm. Four patients had minor limb length discrepancy ranging between +5 and +10 mm; no growth arrest was noted. One patient with an intact but slightly elongated graft required a meniscal suture 34 months after ACL reconstruction following a traumatic medial meniscal lesion.
Conclusion
Despite using the epiphyseal technique in ACL reconstruction, relevant growth discrepancy can occur. Thereby, overgrowth rates appear to potentially pose a major clinical problem, which has remained unreported so far. Overall, there is a considerable high risk of complications in this patient group.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although the knee joint represents a common site for injuries in children, the overall reported incidence is low [19]. This is especially true regarding risk of cruciate ligament injury [28]. Nevertheless, incidence of mid-substance tears of the anterior cruciate ligament (ACL) seems to have increased over the past decades [2, 32]. Reasons include the growing number of children and adolescents participating in organized sports, intensive sports training at an earlier age and a higher rate of diagnosis because of an elevated awareness and an increased use of advanced medical imaging [21].
Treatment of these patients still remains a challenge [2, 7, 10]. Due to poor therapy results, conservative treatment after ACL tears in children has been increasingly abandoned [1, 9, 12, 22, 29, 30]. Delaying operative procedure until the epiphyseal plate has closed is only an option in selected patients. This measure generally involves restricting activity and stabilising the knee using a brace [26, 33]. In order to prevent secondary damage to the meniscal and cartilage structures, operative treatment is suggested [1, 10, 12]. To harm epiphyseal plates in surgical treatment is a major concern in this population. Therefore, to preserve growth plates [34] and to avoid concomitant malalignment and an inequality in leg length, various physeal-sparing ACL reconstruction techniques have been described [4, 5, 13, 17, 23, 25]. The intraarticular anatomical reconstruction sparing the physes as described by Anderson [4] was applied in this case series.
The hypothesis of the present study is that the epiphyseal growth plate sparing reconstruction of the ACL in children avoids the risk of growth disturbance.
Materials and methods
Between 2006 and 2010, 13 knees in 12 patients (two girls, ten boys) were treated using primary, anatomic ACL reconstruction at the University hospital Balgrist, Zurich. A fully physeal-sparing procedure as described by Anderson [4] was used, due to wide open, skeletally immaturity physes. One male patient sustained a bilateral ACL tear, which was treated sequentially. The median age at the time of surgery was 12.1 years (range 10.4–13.4 years). The median interval between injury and surgery was 5 months. One ACL tear was treated in an acute manner (<2 weeks), two subacute (2 weeks–3 month) and ten delayed (>3 month, Ø 10.9 months, range 4–25 months).
All patients were preoperatively assessed by clinical examination and MRI. No combined, complex injuries with accessory ligamentous involvement were detected.
A vertical incision was centred over the insertion of the pes anserinus. The sartorial fascia was then sharply dissected from the tibia, creating an inverted L-shaped flap to facilitate harvesting of the semitendinous (ST) with or without the gracilis (G) tendon. The graft was prepared on a back Table (four ST/G doubled, seven ST threefold-stranded, two ST quadruple-stranded). The epiphyseal femoral and tibial tunnel positioning was performed according to the technique described by Anderson. To ensure that the physeal plate remained unaffected, the guide wires were inserted under image intensifier control. The correct intraarticular insertion of the guide wires was controlled arthroscopically. A position between the anatomic footprint of the anteromedial and posterolateral bundles was chosen to obtain the closest possible anatomic positioning of the graft. Proximally, the graft was attached to a Flipptack™ (Fa. Karl Storz, Tuttlingen, Germany), distally the sutures were secured over a tibial 3.5 mm screw. No additional interference screws were utilized to prevent further damage of epiphyseal cartilage.
The post-operative rehabilitation protocol included partial weight-bearing (15 kg for 6 weeks) and additional bracing (Donjoy 4titude, DJO Global, Guildford, England). Maximal flexion amplitude was restricted to 120° during the first 6 weeks. The tibial screw for distal graft fixation was removed in 10 of 13 knees after a median time of 26 months.
Data of all twelve patients were collected in a retrospective manner. All patients were accessible to follow-up with a median duration of 54 months (range 39–80 months) and assessed by clinical examination (IKDC knee evaluation form) including bilateral instrumented ligament examination using the KT-1000™ knee ligament arthrometer applying 134-N force (MEDmetric® Corporation, San Diego, California).
To assess subjective outcome, patients completed the IKDC subjective form [14], Lysholm knee score [6] and Tegner [6, 31] activity scale at follow-up.
Radiological analysis at follow-up included antero-posterior and lateral knee radiographics as well as long leg radiographs to evaluate limb length discrepancy and leg alignment.
The prospectively collected data according to our routine follow-up protocol were retrospectively analysed. Therefore, no ethical approval was necessary. All patients gave their informed consent.
Results
Only prepubescent patients were included in this study. Maximal age in female was 13.2, in male 13.4 years.
Objective evaluation
Median increase in body height was 26.0 cm (range 5–38 cm) between preoperative status and follow-up.
Clinical examination revealed no extension deficit, but in four knees a slightly reduced flexion of 5°–10° was noted as compared to the opposite side. The patient with bilateral surgery showed a symmetric range of motion with 145-0-5°.
The mean side-to-side difference was 1.5 ± 2.5 mm (range −1 to 8 mm) in ligament laxity testing with the KT-1000 arthrometer. Five knees showed a side-to-side difference >3 mm. No additional ligament injuries were detected.
According the IKDC knee examination form, five knees were rated as grade A, six as grade B and two as grade C.
Subjective assessment
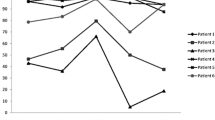
All patients reported normal knee function before injury. According to the IKDC subjective knee evaluation form, median knee function at follow-up was rated 88.5 points (range 74.7–98.9). The median Lysholm score was 93 points (range 73–100). Retrospective self-assessment of pre-injury activity level (Tegner activity scale) averaged 7.7 of 10 points at follow-up 6.2 points.
Radiological assessment
At the latest follow-up, all patients showed closed or nearly closed growth plates without any degenerative alterations in the plain radiographs. Two relevant leg length discrepancies of >10 mm have been observed in this cohort. One patient with early failure followed by second epiphyseal ACL-re-reconstruction developed a leg length discrepancy of + 21 mm and slight varus angulation (1.5° varus, opposite side 4.5° valgus; Fig. 1). The over-length was localized mainly femoral and treated 33 month after index surgery by temporary epiphysiodesis of the distal femur. The second patient showed an excessive leg length of 16 mm. Since he was asymptomatic, no further treatment was necessary.
Four other patients showed an overgrowth of the affected leg between 5 and 10 mm. No tibial slope alteration was measured. All patients with over-length more than 5 mm were male.
Reoperations
During the follow-up period, 3 of 13 knees had unplanned re-intervention, with two symptomatic graft failures. One patient sustained a traumatic graft failure during an ice hockey match 24 month after index surgery. Revision surgery was performed using a standard (adult) technique at the age of 17 years. Another male patient showed graft failure after premature sport activities (goal keeping) between weeks 6 and 12 after ACL reconstruction. The ACL was again reconstructed by the same physeal-sparing technique with ST-Allograft. The third patient sustained a traumatic medial bucket handle tear 34 months after index surgery treated by arthroscopic meniscal suture. Intraoperatively, the reconstructed ACL was slightly elongated but intact.
Discussion
The most important finding of this study was that in spite of physeal-sparing ACL reconstruction, we could find leg length discrepancy in this very young and prepubescent patient group. To our surprise, no premature growth arrest occurred but overgrowth of the affected limb. Overall complication rate remained high.
Overall outcome after ACL reconstruction in skeletally immature patients is difficult to determine due to different bone ages of the subjects and the variety of surgical techniques and grafts used. Limitations of previous studies analysing reconstruction of the ACL in skeletally immature patients mainly include adolescents with advanced bone age; this leads to a less reliable interpretation of data. No clear consensus exists regarding the appropriate treatment algorithm in ACL deficiency in children especially due to the non-existence of randomized controlled trials. On the basis of poor knee function in non-operative treatment [1, 9, 22, 33], the international consensus favours a surgical approach in symptomatic children sustaining an ACL tear, especially for protection against secondary meniscal and chondral damage. Even if most of the studies [8, 11, 15, 18, 20, 27] report a transepiphyseal technique without any growth disturbances even in younger children, Anderson [4] popularized in 2003 a physeal-sparing intraarticular and near anatomical ACL reconstruction and reported successful results without evidence of growth disturbances. To our knowledge, no growth disturbance is reported in the literature using this technique except in one case report which describes distal femoral valgus angulation after revision ACL reconstruction due to premature closure of the lateral side of the femoral physis [24].
No premature closure of growth plates was detectable in this case series. In contrast, we observed two patients with significant limb length difference with overgrowth of more than 10 mm, mainly on the femoral side; in one patient this was associated with varus angulation. In four more children, a limb length discrepancy ranging between 5 and 10 mm was detected. We assumed this was due to a mechanical stimulation of the zone of proliferation of the epiphyseal plate provoked by reaming drill-holes. This phenomenon is also known in children with traumatized growth plate inducing overgrowth and malformation of the affected limb [16, 35]. The overgrowth rate with epiphyseal ACL reconstruction appears to be a potential major clinical problem, which has remained unreported to our knowledge.
The instrumented anterior ligament testing showed a mean side-to-side difference of 1.5 mm. This value is comparable to published data in ACL reconstruction in adults [3]. But 5 of 13 knees showed a side-to-side difference in KT-1000 rating of >3 mm, whereby in two knees a positive Lachman test and pivot-shift test was detectable, suggestive of graft failure. The former patient did not cooperate with post-operative rehabilitation and sustained an early graft failure and developed recurrent instability after revision surgery.
The explanation of this tendency to stretch out after epiphyseal ACL reconstruction remains hypothetical. A causative factor could be the size of the graft, respectively, the horizontal position of the tibial drilling tunnel.
There are several limitations in the present study. First, the cohort was very small, which is explained by the preadolescent age of the patients. Second, the precise radiological determination of skeletal age was not available for every patient. Additionally, the mechanical axes were available only at the post-operative follow-up and not preoperatively. Therefore, physiological limb axe differences could not be excluded. Nevertheless, the cohort is uniform regarding the identical, standardized technique used by one single orthopaedic surgeon in a young and prepubescent age group.
Conclusion
This study demonstrates that epiphyseal ACL reconstruction in prepubescent children results in acceptable clinical outcome with good patient satisfaction. Nevertheless, a high percentage of patients showed a KT-1000 rating of greater than 3 mm side–to-side difference at follow-up.
The most important finding of this study is the high overgrowth rate with epiphyseal ACL reconstruction. Therefore, regular follow-ups of these children until growth is completed is strongly recommended.
The overall failure and reoperation rate is higher than in ACL reconstruction in adults and has to be explained to the parents. Children’s compliance remains a concern after such surgery. As a consequence, we prescribe brace treatment for at least 3 months post-operatively.
References
Aichroth PM, Patel DV, Zorrilla P (2002) The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. J Bone Joint Surg Br 84(1):38–41
Al-Hadithy N, Dodds AL, Akhtar KS, Gupte CM (2013) Current concepts of the management of anterior cruciate ligament injuries in children. Bone Joint J 95-B(11):1562–1569
Alentorn-Geli E, Lajara F, Samitier G, Cugat R (2010) The transtibial versus the anteromedial portal technique in the arthroscopic bone-patellar tendon-bone anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 18(8):1013–1037
Anderson AF (2003) Transepiphyseal replacement of the anterior cruciate ligament in skeletally immature patients. A preliminary report. J Bone Joint Surg Am 85-a(7):1255–1263
Bonnard C, Fournier J, Babusiaux D, Planchenault M, Bergerault F, de Courtivron B (2011) Physeal-sparing reconstruction of anterior cruciate ligament tears in children: results of 57 cases using patellar tendon. J Bone Joint Surg Br 93(4):542–547
Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR (2009) The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med 37(5):890–897
Chotel F, Henry J, Seil R, Chouteau J, Moyen B, Berard J (2010) Growth disturbances without growth arrest after ACL reconstruction in children. Knee Surg Sports Traumatol Arthrosc 18(11):1496–1500
Courvoisier A, Grimaldi M, Plaweski S (2011) Good surgical outcome of transphyseal ACL reconstruction in skeletally immature patients using four-strand hamstring graft. Knee Surg Sports Traumatol Arthrosc 19(4):588–591
Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL (2012) Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med 40(9):2128–2133
Fabricant PD, Jones KJ, Delos D, Cordasco FA, Marx RG, Pearle AD, Warren RF, Green DW (2013) Reconstruction of the anterior cruciate ligament in the skeletally immature athlete: a review of current concepts: AAOS exhibit selection. J Bone Joint Surg Am 95(5):e28
Gaulrapp HM, Haus J (2006) Intraarticular stabilization after anterior cruciate ligament tear in children and adolescents: results 6 years after surgery. Knee Surg Sports Traumatol Arthrosc 14(5):417–424
Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK (1992) Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy 8(2):229–233
Guzzanti V, Falciglia F, Stanitski CL (2003) Physeal-sparing intraarticular anterior cruciate ligament reconstruction in preadolescents. Am J Sports Med 31(6):949–953
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Hui C, Roe J, Ferguson D, Waller A, Salmon L, Pinczewski L (2012) Outcome of anatomic transphyseal anterior cruciate ligament reconstruction in Tanner stage 1 and 2 patients with open physes. Am J Sports Med 40(5):1093–1098
Jordan SE, Alonso JE, Cook FF (1987) The etiology of valgus angulation after metaphyseal fractures of the tibia in children. J Pediatr Orthop 7(4):450–457
Kocher MS, Garg S, Micheli LJ (2006) Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. Surgical technique. J Bone Joint Surg Am 88(Suppl 1 Pt 2):283–293
Kohl S, Stutz C, Decker S, Ziebarth K, Slongo T, Ahmad SS, Kohlhof H, Eggli S, Zumstein M, Evangelopoulos DS (2014) Mid-term results of transphyseal anterior cruciate ligament reconstruction in children and adolescents. Knee 21(1):80–85
Kraus T, Svehlik M, Singer G, Schalamon J, Zwick E, Linhart W (2012) The epidemiology of knee injuries in children and adolescents. Arch Orthop Trauma Surg 132(6):773–779
Kumar S, Ahearne D, Hunt DM (2013) Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: follow-up to a minimum of sixteen years of age. J Bone Joint Surg Am 95(1):e1
Labella CR, Hennrikus W, Hewett TE (2014) Anterior cruciate ligament injuries: diagnosis, treatment, and prevention. Pediatrics. doi:10.1542/peds.2014-0623
Lawrence JT, Argawal N, Ganley TJ (2011) Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med 39(12):2582–2587
Lawrence JT, Bowers AL, Belding J, Cody SR, Ganley TJ (2010) All-epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clin Orthop Relat Res 468(7):1971–1977
Lawrence JT, West RL, Garrett WE (2011) Growth disturbance following ACL reconstruction with use of an epiphyseal femoral tunnel: a case report. J Bone Joint Surg Am 93(8):e39
McCarthy MM, Graziano J, Green DW, Cordasco FA (2012) All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech 1(2):e231–e239
Moksnes H, Engebretsen L, Eitzen I, Risberg MA (2013) Functional outcomes following a non-operative treatment algorithm for anterior cruciate ligament injuries in skeletally immature children 12 years and younger. A prospective cohort with 2 years follow-up. Br J Sports Med 47(8):488–494
Nikolaou P, Kalliakmanis A, Bousgas D, Zourntos S (2011) Intraarticular stabilization following anterior cruciate ligament injury in children and adolescents. Knee Surg Sports Traumatol Arthrosc 19(5):801–805
Parkkari J, Pasanen K, Mattila VM, Kannus P, Rimpela A (2008) The risk for a cruciate ligament injury of the knee in adolescents and young adults: a population-based cohort study of 46,500 people with a 9 year follow-up. Br J Sports Med 42(6):422–426
Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ (2013) Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. doi:10.1177/0363546513510889
Streich NA, Barie A, Gotterbarm T, Keil M, Schmitt H (2010) Transphyseal reconstruction of the anterior cruciate ligament in prepubescent athletes. Knee Surg Sports Traumatol Arthrosc 18(11):1481–1486
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Utukuri MM, Somayaji HS, Khanduja V, Dowd GS, Hunt DM (2006) Update on paediatric ACL injuries. Knee 13(5):345–352
Vavken P, Murray MM (2011) Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy 27(5):704–716
Yoo WJ, Kocher MS, Micheli LJ (2011) Growth plate disturbance after transphyseal reconstruction of the anterior cruciate ligament in skeletally immature adolescent patients: an MR imaging study. J Pediatr Orthop 31(6):691–696
Zionts LE, Harcke HT, Brooks KM, MacEwen GD (1987) Posttraumatic tibia valga: a case demonstrating asymmetric activity at the proximal growth plate on technetium bone scan. J Pediatr Orthop 7(4):458–462
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koch, P.P., Fucentese, S.F. & Blatter, S.C. Complications after epiphyseal reconstruction of the anterior cruciate ligament in prepubescent children. Knee Surg Sports Traumatol Arthrosc 24, 2736–2740 (2016). https://doi.org/10.1007/s00167-014-3396-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3396-4