Abstract
Purposes
To determine the long-term survival rate of an all-polyethylene tibial unicompartmental knee arthroplasty (UKA) in a large series of consecutive patients and to investigate the possible factors that could influence the outcome.
Methods
A retrospective evaluation of 273 patients at 6–13 years of follow-up was performed. Clinical evaluation was based on KSS and WOMAC scores. Subjective evaluation was based on a visual analogue scale for pain self-assessment. Radiographic evaluation was performed to assess femoral-tibial angle (FTA), posterior tibial slope (PTS) and tibial plateau angle (TPA). A Kaplan–Meier survival analysis was performed assuming revision for any reason as primary endpoint.
Results
The 10-year implant survivorship was 87.6 %. Twenty-five revisions (9.2 %) were performed, and aseptic loosening of the tibial component was the most common failure mode (11 cases, 4 %). The comparison of survival rate according to age at surgery did not show significant difference. Age at surgery, FTA, TPA and PTS were not related to higher risk of revision. No correlations were found between BMI, age at surgery and clinical scores. Finally, no statistical differences of radiographic measurements were found between revisions and non-revisions.
Conclusions
The present study has demonstrated on a large series of patients that UKA with an all-polyethylene tibial component, with an accurate technique and a proper patient selection, can provide a satisfactory clinical and functional outcome and a good overall survivorship of the implant at long-term follow-up. These advantages could be achieved at a lower cost.
Level of evidence
Retrospective Therapeutic Study, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many authors [2, 3, 7, 11] have reported survival rates of different unicompartmental knee arthroplasty (UKA) implants ranging from 85 to 100 % at 5–10-year follow-up. Some studies [1, 24, 29] have reported high failure rates at a short term using an all-polyethylene tibial component UKA. Mariani et al. [24] reported a 38 % failure rate of 39 all-polyethylene UKAs at 9–12-month post-operatively. Schai et al. [29] reported a 7 % failure rate at 12 months post-operatively in a group of 28 patients who received an all-polyethylene UKA.
Other studies found no superiority of metal back versus all-polyethylene UKA. Borus and Thornhill [8] failed to demonstrate significant differences regarding the failure rate and clinical results between all-polyethylene and metal-backed implants at more than 10 years of follow-up. Hyldahl et al. [19] failed to demonstrate any difference in clinical outcome or tibial component migration using radiostereometric analysis in 45 patients randomized to all-polyethylene or metal-backed tibial implants. They concluded in favour of all-polyethylene tibial design because of optimal biomechanical strength, with no problems of modularity and reduced wear at interface, at a lower cost. Zambianchi et al. [35] did a comparative study between all-polyethylene and metal back designs, and they found that prosthetic designs, models and fixation geometry do not affect UKA outcome.
Many studies have assessed all-polyethylene tibial component UKA either at short-term follow-up or of a small number of patients [12, 24, 28]. To the best of our knowledge, this is the first study to assess the long-term follow-up of a large number of patients. Starting from the hypothesis that all-polyethylene UKA provides a good survivorship at long-term follow-up and that age at surgery and mal-alignment influence UKA survivorship, the primary aim of the present study was to perform a long-term survival analysis of a single-design all-polyethylene tibial component UKA in a large series of consecutive patients, assuming revision for any reason as primary endpoint, and the secondary aim was to investigate whether age at surgery and post-operative femoro-tibial axis and tibial component alignment on the coronal and sagittal plane could be associated with an increased risk of revision.
Materials and methods
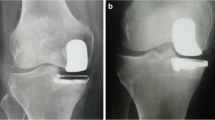
Two-hundred and eighty consecutive patients underwent unilateral medial UKA (DePuy, Preservation Uni) from 2000 to 2007. At a mean 122-month follow-up, 7 patients had died for reasons unrelated to surgery leaving 273 patients for the analysis. Demographics data are resumed in Table 1. Pre-operative visual analogue scale (VAS) for pain self-assessment was collected for all patients from patients’ medical records. Short-film pre-operative weight-bearing radiographs of the knee were also evaluated to determine the tibial component positioning in the coronal plane by measuring the femoro-tibial angle (FTA) and the tibial plateau angle (TPA) and in the sagittal plane by measuring the posterior tibial slope (PTS). Moreover, all patients received a pre-operative magnetic resonance imaging (MRI) to document the absence of significant degenerative changes in the lateral and the patello-femoral (PF) compartment. The mean pre-operative range of motion (ROM) was determined with a high-precision goniometer.
All patients were retrospectively evaluated clinically at final follow-up using the KSS, WOMAC score, ROM and VAS. Moreover, FTA, TPA and PTS angles were measured at final follow-up on short-film weight-bearing radiographs of the knee and compared between revised and non-revised patients. Any surgical treatments related to the UKA implant were considered as failure. Influence of age at surgery (<60 and ≥60 years) on survival curves was assessed. A correlation between BMI and age at surgery and clinical scores was also investigated.
The surgical indications for UKA were pain and tenderness localized to the medial joint line, active and passive flexion >90°, extension lag <10°, isolated medial compartment osteoarthritis with complete loss of cartilage on pre-operative radiographs (Ahlbäck grade 4) or avascular necrosis of the medial compartment on MRI, varus deformity <15°, no significant cartilage degeneration in the lateral and PF compartment at pre-operative MRI, correctable varus under spinal anaesthesia, intact anterior cruciate ligament and posterior cruciate ligament, full-thickness cartilage wear restricted to the antero-medial half of the resected medial tibial plateau at intra-operative inspection, no previous high tibial osteotomy, patients with BMI < 35, and the absence of PF joint symptoms, chondrocalcinosis or other inflammatory degenerative joint diseases [9, 25].
Pre-operative clinical and radiographic values are reported in Table 2. Varus knee was defined as FTA > 175°, normal knee was defined as 170° < FTA < 175°, and valgus knee was defined as FTA < 170°. Moreover, it was assumed a TPA > 90° for valgus knee and a TPA < 90° for varus knee. All patients presented a varus deformity (Table 2). All pre- and post-operative radiographic measurements were taken using a recognised technique [10].
Reason for revision was accurately documented based on radiographic and clinical evaluation and intra-operative direct inspection.
This is a retrospective study and post hoc power analysis is non-informative (if not misleading). Some articles report the futility of post hoc power analysis [14, 21]. To show the uncertainty of these results, confidence intervals have been reported.
Surgical technique
All UKAs (De Puy, Preservation Uni) were performed with a minimally invasive quadriceps-sparing technique [11]. The key factor was the restoration of the pre-pathological mild varus alignment to avoid over-constraining of the lateral compartment and to preserve a little laxity which improves post-operative ROM [4, 5, 34]. An undercorrection by 3°–5° was the surgical goal [11, 25]. To restore the pre-pathological native alignment, the tibial cut was performed perpendicular to the epiphyseal axis, i.e. the line perpendicularly joining the visible residual line of the metaphyseal growing cartilage and the midpoint of the tibial plateau. After removal of the tibial resection, the adequate trial polyethylene component was positioned. The minimum thickness for the tibial component, which is 7 mm, was used in 237 cases (86.8 %), while the intermediate thickness, which is 9.5 mm, was used in 36 cases (13.2 %). In no case, the maximum polyethylene thickness, which is 11.5 mm, was used. To verify that the bone cut was perpendicular to the epiphyseal axis, a fluoroscopic check was performed in every case and all components were cemented using a single 20 g mix of cement with no antibiotic addition.
Statistical analysis
Statistical analysis was performed using SPSS 16 (SPSS Inc., Chicago, Illinois). Measurable parameters were expressed as arithmetic mean ± standard deviation and min–max ranges. Categorical variables were expressed as percentage. Statistical comparisons between the pre-operative and follow-up parametric data and between follow-up radiological parameters of revised and non-revised cases were performed using the Student’s t test. Comparisons of clinical scores between patients under and over 60 years old were also analysed using Student’s t test. The population study was tested for normal distribution before the Student’s t test was applied. Correlations between BMI and age at surgery and clinical scores were performed using Wilcoxon test. Survival analysis was performed with a Kaplan–Meier curve, with revision surgery as failure criteria. Comparison of survival rate between dichotomized subgroups was evaluated using the log-rank test. A logistic regression was performed using failure as endpoint, age at surgery as independent variable.
Results were considered statistically significant with P < 0.05. Confidence interval was set at 95 %.
Results
Twenty-five patients (9.2 %) underwent revision surgery after a mean interval time of 6 years (range 3–9) from index surgery. In one case out of 25, the revision was performed, due to severe joint stiffness. Five patients out of 25 were revised for persistent pain on the tibial side with no radiographic evidence of medial tibial collapse, three patients out of 25 were revised for medial tibial collapse, thirteen patients out of 25 were revised for aseptic loosening of tibial component, and finally, three patients out of 25 were revised for prosthetic infection (Table 3).
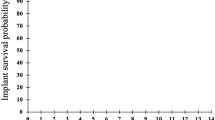
The Kaplan–Meier curve (Fig. 1) showed a survival rate of 92.2 % at 5 years and of 87.6 % at 10 years, with a mean survival time of 122 months (SD 18). The comparison of survival rate according age at surgery did not show significant difference (n.s) (Fig. 2). The logistic regression did not found any of the considered parameters (age at surgery, FTA, TPA and PTS) to be related to higher risk of revision (n.s). No correlations were found between BMI, age at surgery and clinical scores (n.s). No statistical differences of radiographic measurements were found between revisions and non-revisions (n.s). FTA, PTA and PTS results are described in Table 2.
Discussion
The most important finding of the present study was that a 10-year Kaplan–Meier survivorship of 87.6 % with revision for any reason as endpoint was found in 273 patients with medial compartment OA treated with an all-polyethylene tibial component UKA. Moreover, age at surgery, FTA, PTA and PTS were not associated with higher risk of revision.
Some studies have reported unsatisfactory failure rates of all-polyethylene UKAs, indicating aseptic loosening of the femoral component and medial tibial collapse as the predominant failure modes [5, 24]. On the contrary, other authors reported a survivorship ranging from 90 to 98 % at 5–10-year follow-up [23, 27, 29]. These conflicting results were based on small series of non-consecutive patients, while the present study has retrospectively reviewed 273 consecutive patients, demonstrating a survival rate of 92.2 % at 5 years and of 87.6 % at 10 years which is comparable to results reported in the literature [13, 23, 31].
Schai et al. [29] reported a 93 % survivorship at 2–6 years in 28 UKAs performed in patients under 60 years of age, with 90 % of the patients rated good or excellent using the KSS. Similarly, Romanowski et al. [27] reported a 98 % survivorship at 8-year follow-up with a sample of 136 patients, with 86 % of the patients rated as good or excellent using the KSS. The present study has demonstrated similar clinical results. It has shown that 83.9 % of the patients were rated as good or excellent with KSS (177 patients with excellent KSS results, 52 patients with good KSS results).
In the present study, age was not correlated with a higher risk revision, which is in contrast with other studies [9, 20, 34]. W-Dahl et al. [33] have reported that the risk of revision for UKA is affected by age and the cumulative rate of revisions decreases with increasing age. This could be due to the low activity level of patients who underwent a UKA regardless of age. This low activity level could be due to worries connected with the presence of the prosthesis, and the advice of the surgeon to be cautious because of concerns about increased wear of weight-bearing surfaces, which could result in implant loosening [6, 18, 30].
In the present study, no statistical difference of radiographic measurements was found between revised and non-revised patients and this could be due to the fact that the surgical technique used by the authors respect the guidelines reported in the literature [15, 17]. Gulati et al. [15] recommended a range of implantation for the tibial component between ±5° varus/valgus and between 2° and 12° posterior tibial slope avoiding a posterior tibial slope >7°. In all cases, a slight undercorrection was performed in order to avoid both rapid degeneration of the non-replaced compartment and early loosening of the implant without changing the posterior slope [17, 25].
In the present study, no correlations were found between BMI, age at surgery and clinical scores which is in agreement with other studies [22, 26, 31].
Femoral fixation failure has been addressed in the current literature as the most frequent reason for revision [16, 29, 32], while in the present study, aseptic loosening of the tibial component was the most common mode of failure and no femoral component loosening was documented. Wear debris could have produced a higher rate of tibial component loosening [4]. However, creep and true wear of the all-polyethylene tibial component could not be found either radiographically or intra-operatively. Moreover, as stated by the authors in a previous study [9], cement fixation of an all-polyethylene tibial component may be inferior to a metal-backed component placing additional mechanical stress at the bone–cement implant interface resulting in higher failure rate of this type of implants.
The results reported in the present study confirmed the hypothesis that all-polyethylene UKA provides a good survivorship and that age at surgery and femoro-tibial anatomical axis and tibial component alignment do not influence UKA survivorship; thus, the authors recommend the use of all-polyethylene UKA that provides a satisfactory outcome at a lower cost.
The present study has several limitations: first, its retrospective design. Second, a correlation between BMI and higher revision rate was not assessed because selection criteria limited the indications to patients with a BMI <35 to lower the risk of revision, which is confirmed by the results reported by Bonutti et al. who concluded that patients with BMIs >35 are at a higher risk of early failure when compared to patients with BMIs <35. Third, there is no direct comparison to a group of patients who received a metal-backed polyethylene component. However, there are several advantages of this study: it assessed the results of a large series of patients who underwent an all-polyethylene tibial component UKA.
Conclusions
The present study has demonstrated on a large series of patients that UKA with an all-polyethylene tibial component, with an accurate technique and patient selection, can provide a satisfactory clinical and functional outcome and a good overall survivorship of the implant at long-term follow-up.
References
Aleto TJ, Berend ME, Ritter MA, Faris PM, Meneghini RM (2008) Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty 23:159–163
Amin AK, Patton JT, Cook RE, Gaston M, Brenkel IJ (2006) Unicompartmental or total knee arthroplasty?: Results from a matched study. Clin Orthop Relat Res 451:101–106
Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM (2002) Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am 84-A(12):2235–2239
Argenson JN, Parratte S (2006) The unicompartmental knee: design and technical considerations in minimizing wear. Clin Orthop Relat Res 452:137–142
Argenson JN, Parratte S, Flecher X, Aubaniac JM (2007) Unicompartmental knee arthroplasty: technique through a mini-incision. Clin Orthop Relat Res 464:32–36
Bauman S, Williams D, Petruccelli D et al (2007) Physical activity after total joint replacement: a cross-sectional survey. Clin J Sport Med 17(2):104–108
Berger RA, Meneghini RM, Jacobs JJ, Sheinkop MB, Della Valle CJ, Rosenberg AG, Galante JO (2005) Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am 87(5):999–1006
Borus T, Thornhill T (2008) Unicompartmental knee arthroplasty. J Am Acad Orthop Surg 16(1):9–18
Bruni D, Akkawi I, Iacono F, Raspugli GF, Gagliardi M, Nitri M, Grassi A, Zaffagnini S, Bignozzi S, Marcacci M (2013) Minimum thickness of all-poly tibial component unicompartmental knee arthroplasty in patients younger than 60 years does not increase revision rate for aseptic loosening. Knee Surg Sports Traumatol Arthrosc 21(11):2462–2467
Bruni D, Iacono F, Raspugli G, Zaffagnini S, Marcacci M (2012) Is unicompartmental arthroplasty an acceptable option for spontaneous osteonecrosis of the knee? Clin Orthop Relat Res 470(5):1442–1451
Bruni D, Iacono F, Russo A, Zaffagnini S, Muccioli GM, Bignozzi S, Bragonzoni L, Marcacci M (2010) Minimally invasive unicompartmental knee replacement: retrospective clinical and radiographic evaluation of 83 patients. Knee Surg Sports Traumatol Arthrosc 18(6):710–717
Cartier P, Khefacha A, Sanouiller JL, Frederick K (2007) Unicondylar knee arthroplasty in middle-aged patients: a minimum 5-year follow-up. Orthopedics 30(8 Suppl):62–65
Chatellard R, Sauleau V, Colmar M et al (2013) Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res 99(4 Suppl):S219–S225
Goodman SN, Berlin JA (1994) The use of predicted confidence intervals when planning experiments and the misuse of power when interpreting results. Ann Intern Med 121(3):200–206
Gulati A, Pandit H, Jenkins C, Chau R, Dodd CA, Murray DW (2009) The effect of leg alignment on the outcome of unicompartmental knee replacement. J Bone Joint Surg Br 91(4):469–474
Hamilton WG, Collier MB, Tarabee E, McAuley JP, Engh CA Jr, Engh GA (2006) Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty 21(6 Suppl 2):98–107
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86:506–511
Huch K, Müller KA, Stürmer T et al (2005) Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis 64(12):1715–1720
Hyldahl HC, Regnér L, Carlsson L, Kärrholm J, Weidenhielm L (2001) Does metal backing improve fixation of tibial component in unicondylar knee arthroplasty? A randomized radiostereometric analysis. J Arthroplasty 16(2):174–179
Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC (2009) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17(1):48–52
Levine M, Ensom MH (2001) Post hoc power analysis: an idea whose time has passed? Pharmacotherapy 21(4):405–409
Lustig S, Barba N, Magnussen RA, Servien E, Demey G, Neyret P (2012) The effect of gender on outcome of unicompartmental knee arthroplasty. Knee 19(3):176–179
Lustig S, Paillot JL, Servien E, Henry J, Ait Si Selmi T, Neyret P (2008) Cemented all polyethylene tibial insert unicompartmental knee arthroplasty: a long term follow-up study. Orthop Traumatol Surg Res 95(1):12–21
Mariani EM, Bourne MH, Jackson RT, Jackson ST, Jones P (2007) Early failure of unicompartmental knee arthroplasty. J Arthroplasty 22(6 Suppl 2):81–84
Mullaji AB, Sharma A, Marawar S (2007) Unicompartmental knee arthroplasty: functional recovery and radiographic results with a minimally invasive technique. J Arthroplasty 22(4 Suppl 1):7–11
Murray DW, Pandit H, Weston-Simons JS, Jenkins C, Gill HS, Lombardi AV, Dodd CA, Berend KR (2013) Does body mass index affect the outcome of unicompartmental knee replacement? Knee 20(6):461–465
Romanowski MR, Repicci JA (2002) Minimally invasive unicondylar arthroplasty: eight-year follow-up. J Knee Surg 15(1):17–22
Saenz CL, McGrath MS, Marker DR, Seyler TM, Mont MA, Bonutti PM (2010) Early failure of a unicompartmental knee arthroplasty design with an all-polyethylene tibial component. Knee 17(1):53–56
Schai PA, Suh JT, Thornhill TS, Scott RD (1998) Unicompartmental knee arthroplasty in middle-aged patients: a 2- to 6-year follow-up evaluation. J Arthroplasty 13(4):365–372
Schmalzried TP, Shepherd EF, Dorey FJ et al (2000) Wear is a function of use, not time. Clin Orthop 381:36–46
Sébilo A, Casin C, Lebel B, Rouvillain JL, Chapuis S, Bonnevialle P (2013) Clinical and technical factors influencing outcomes of unicompartmental knee arthroplasty: retrospective multicentre study of 944 knees. Orthop Traumatol Surg Res 99(4 Suppl):S227–S234
Skyrme AD, Mencia MM, Skinner PW (2002) Early failure of the porous-coated anatomic cemented unicompartmental knee arthroplasty: a 5- to 9-year follow-up study. J Arthroplasty 17(2):201–205
W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S (2010) Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop 81(1):90–94
Whiteside LA (2005) Making your next unicompartmental knee arthroplasty last: three keys to success. J Arthroplasty 20(4 Suppl 2):2–3
Zambianchi F, Digennaro V, Giorgini A, Grandi G, Fiacchi F, Mugnai R, Catani F (2014) Surgeon’s experience influences UKA survivorship: a comparative study between all-poly and metal back designs. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2958-9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bruni, D., Gagliardi, M., Akkawi, I. et al. Good survivorship of all-polyethylene tibial component UKA at long-term follow-up. Knee Surg Sports Traumatol Arthrosc 24, 182–187 (2016). https://doi.org/10.1007/s00167-014-3361-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3361-2