Abstract
Purpose
Previous investigations suggested that the geometry of the proximal femur may be related to osteoarthritis of the tibiofemoral joint and various patellofemoral joint conditions. This study aims to investigate the correlation between proximal and distal femoral geometry. Such a correlation could aid our understanding of patient complications after total knee arthroplasty (TKA) and be of benefit for further development of kinematic approaches in TKA.
Methods
CT scans of 60 subjects (30 males, 30 females) were used to identify anatomical landmarks to calculate anatomical parameters of the femur, including the femoral neck anteversion angle, neck–shaft angle (NSA), mediolateral offset (ML-offset), condylar twist angle (CTA), trochlear sulcus angle (TSA) and medial/lateral trochlear inclination angles (MTIA/LTIA). Correlation analyses were carried out to assess the relationship between these parameters, and the effect of gender was investigated.
Results
The CTA, TSA and LTIA showed no correlation with any proximal parameter. The MTIA was correlated with all three proximal parameters, mostly with the NSA and ML-offset. Per 5° increase in NSA, the MTIA was 2.1° lower (p < 0.01), and for every 5 mm increase in ML-offset, there was a 2.6° increase in MTIA (p < 0.01). These results were strongest and statistically significant in females and not in males and were independent of length and weight.
Conclusions
Proximal femoral geometry is distinctively linked with trochlear morphology. In order to improve knowledge on the physiological kinematics of the knee joint and to improve the concept of kinematic knee replacement, the proximal femur seems to be a factor of clinical importance.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human body is a complex and continually adapting organism. The anatomy of the proximal femur has been proven to be a factor of influence in the biomechanics and morphology of the more distal parts of the lower limb [3, 9, 10, 17, 24, 33]. It follows that the continual development of the human body would allow it to adapt to compensate for altered biomechanics with consequences to the surrounding areas, such as the knee joint. Regarding the tibiofemoral joint, recent work of Boissonneault et al. [3] investigating 1,328 hip/knee joints confirms the results of others [9, 33] concluding that anatomical variations at the hip and pelvis are associated with compartment-specific osteoarthritis of the knee. Others studying the patellofemoral joint found that femoral anteversion is associated with higher patellofemoral contact pressures [17], anterior knee pain [10] and patellofemoral pain syndrome [24]. It is therefore theorised that the morphology of the distal femur is closely related to that of the proximal femur.
If this is the case, total knee arthroplasty (TKA) solely based on distal femoral morphology could create suboptimal component placement which may lead to pain, limited function or lower survival rates. Despite the high rate of TKA, of which 90,842 procedures were reported in the UK for 2012, only 70.8 % of patients report themselves as being much better with the reasoning for the remaining unsatisfactory results unknown [1]. The clinical success of TKA depends heavily on the relative position of the components, which have a direct effect on knee alignment, peri-articular ligament balancing and flexion/extension gap kinematics. Whereas correct component positioning in the coronal plane influences reconstruction of the mechanical axis of the leg, component positioning in the axial plane (often referred to as rotational alignment) affects joint stability in flexion, tibiofemoral and patellofemoral joint kinematics [22]. The incidence of implant malpositioning can be as high as 20–40 % as reported in the literature [21]. To reduce the amount of malpositioning, sophisticated intraoperative aids have been developed such as computer navigation and patient-specific instrumentation (PSI). Although these technologies in general lead to improved radiographic alignment, they do not necessarily lead to improved clinical outcome [5]. Therefore, a more kinematic approach in knee reconstruction has been proposed in addition to classical TKA based on anatomical or mechanical reconstruction of the knee joint. This concept, based on the work of Hollister et al. [12] and others [8, 16], is considered to be a three-dimensional alignment of components, in contrast to the classical concept which is two dimensional. Clinical results of the kinematic approach are promising, demonstrated by better clinical scores such as WOMAC, KSS and the Oxford knee score [7, 14]. Kinematic analysis of the human knee is also done in the field of ACL reconstruction. Hoshino et al. [13] studied the effect of distal femoral bony morphology on in vivo knee translational and rotational kinematics and found that the location and orientation of the transcondylar axis were significantly related to knee kinematics during high-load functional activity and that this effect was different between males and females. Despite the big interest in kinematic analysis of the physiological knee joint and in kinematic reconstruction of this joint in TKA, it has never been investigated whether the morphology of the proximal femur is correlated with the morphology of the distal femur. If a relationship does exist between the proximal and distal femur, it is necessary to take this into account in the kinematic approach in TKA, potentially leading to improved component placement and better clinical outcome.
Based on the evidence summarised above, indicating that the geometry of the proximal femur is of clinical importance in various conditions affecting the patellofemoral joint, we aimed to investigate this correlation further. The primary hypothesis of this study was that the femoral neck anteversion angle is correlated with the morphology of the distal femoral trochlea. The secondary hypothesis was that this correlation is gender specific. Finally, the study aimed to analyse the correlation between the morphology of the proximal and distal femur further by investigating additional parameters on the proximal femur in the coronal plane (neck–shaft angle and mediolateral offset) and on the distal femur (transepicondylar axis).
To the best of our knowledge, this is the first time that a correlation between the shape of the distal femoral trochlea and morphological parameters of the proximal femur has been investigated, not only in the transverse plane but also in the coronal plane.
Materials and methods
The study used CT scans to collect anthropometric data on 60 octogenarian subjects, of which 30 were male and 30 were female (mean age 83 years, SD 2.8 years, range 80–90 years). These subjects were taken randomly from a large CT database containing healthy Caucasian subjects aged 80 years and older. The scans were made as an extension of a medical prescribed CT scan, mainly to investigate gastro-intestinal or urogenital conditions. Subjects with bone metabolism disorders, skeletal metastases, post-traumatic conditions of the femur or femoral implants were excluded. The local institutional review board (IRB) of the Atrium Medical Centre Heerlen gave approval for this study (number 07-T-44/IIIb), and all subjects gave written informed consent.
Rationale behind outcome parameters
The aim was to choose proximal and distal femoral parameters that were considered to be the most relevant for the function of the femur and its adjacent hip and knee joint, not only in a physiological situation but also after arthroplasty. On the proximal femur, the mediolateral offset (ML-offset) and the neck-shaft angle (NSA) determine the position of the centre of rotation and therefore influence the abductor lever arm. Both parameters are also associated with osteoarthritis of the tibiofemoral joint [3, 20, 33]. The femoral neck anteversion angle (FNAA) determines the rotation of the lower limb in the transverse plane and is among other conditions also associated with anterior knee pain and patellar dislocation [10, 17]. The role of the FNAA in the development of osteoarthritis of the knee is still under debate [9, 11]. On the distal femur, the posterior condylar line (PCL) and the transepicondylar axis (TEA) are used to determine the axial rotation of the distal femur and form key parameters in TKA [22, 30, 32]. The trochlear sulcus angle (TSA) and the medial/lateral trochlear inclination angle (MTIA and LTIA) are key parameters in trochlear morphology and patellofemoral joint kinematics [27, 31].
Generation of standardised CT models
High-resolution CT scans (scan field of view 500 mm, 1 mm slice thickness, pixel size 0.98 × 0.98 mm) of the 60 subjects were loaded in DICOM file format into Mimics 10.01 (Materialise, Leuven, Belgium). To ensure that the studied femora were consistently aligned, the initial step of every sample analysis was to realign the femur to its mechanical axis (MA) as shown in Fig. 1. Firstly, a sphere was fitted to the femoral head, followed by locating the centre of the intercondylar notch (INC) [18]. The MA was then defined by joining the centre of the sphere (femoral head centre, FHC) to the INC. The femur was realigned, and reslicing was performed along this mechanical axis with a 1 mm slice thickness. The cortical bone was segmented using the built-in thresholding mask, which is based on the Hounsfield Unit (HU) scale to separate the bone from the soft tissues. The HU scale used ranged from 226 HU minimum to the maximum HU value found on the scan (mean 2,463 HU, range 1,995–3,070 HU). The region growing tool was then used to create a mask, so that a 3D model of the right femur could be formed. The accuracy of CT-based bony measurements has been proven to be around 1 mm (±0.27 mm) using the CT settings described above [23]. Rubin et al. [25] investigating the morphology of the proximal femur comparing CT scans with direct anatomical measurements using a calliper found a similar accuracy, namely 0.8 mm (±0.7 mm).
Definition of landmarks
Once the femur samples had been accurately aligned along the mechanical axis, it was possible to identify key anatomical landmarks and parameters in the proximal and distal femur as displayed in Figs. 2 and 3, respectively. In the proximal femur, two circles were drawn on the femoral neck of the slice just distal to the most caudal part of the femoral head according to the method described by Sugano et al. [28], and their centre points were noted (centre 1, centre 2). The femoral neck axis (FNA) was taken to be the angle of the femoral neck at the defined slice level as it is believed to provide the best approximation to the anteversion angle [28]. The position of the FNA was found by joining the centre 1 and centre 2 points (Fig. 2). This technique was used as it allowed calculation of the FNA using a single image slice, in addition to its repeatability when using Mimics software and CT scans. In the 3D model, the central axis of the proximal femur was found by fitting a cylinder to the periosteal tubular surface of the proximal femur, just distal to the lesser trochanter. The femoral neck axis was reconstructed in 3D by connecting the centre of the femoral head (FHC) and the centre of the femoral neck (Fig. 2). In the distal femur, the landmarks identified included the most prominent points of the medial and lateral epicondyles (ME and LE) and the most dorsal aspects of the medial and lateral condyles (MPC, LPC). The clinical transepicondylar axis (TEA) was found by joining the ME and LE points and the posterior condylar line (PCL) from the MPC and LPC points (Fig. 3). In addition, the geometry of the trochlear groove was defined at four separate slices perpendicular to the MA, each 5 mm apart, starting at the level of the INC (level 1 = INC; level 2 = 5 mm proximal to INC; level 3 = 10 mm proximal to INC; level 4 = 15 mm proximal to INC). On these slices, the deepest part of the trochlear groove (TG) and the most anterior points of the medial and lateral condyles (AMC, ALC) were marked to represent a consistent measurement of the trochlea. The medial and lateral inclination lines of the trochlea were found by connecting the TG point with the AMC and ALC point, respectively. Finally, x, y, z coordinates of all landmarks were inserted into the anthropometric data spreadsheet. The landmarks of interest are summarised in Table 1.
Anatomical landmarks of the distal femur. a Ventral view, b dorsal view, c caudal view, d medial view, e lateral view, f axial CT slice. LE lateral epicondyle, ME medial epicondyle, ALC anterior lateral condylar point, AMC anterior medial condylar point, TG trochlear groove point, LPC lateral posterior condylar point, MPC medial posterior condylar point, TEA transepicondylar axis, PCL posterior condylar line
Definition of outcome parameters
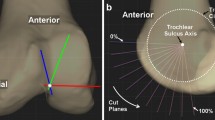
The anatomical points and axes measured were then processed to derive key anthropometric data for analysis. Firstly, the FNAA was calculated, which was defined as the angle between the FNA and the PCL (Fig. 4) [18]. The NSA was defined as the angle between the proximal femur axis and the FNA [19]. ML-offset was defined as the shortest distance between the FHC and the proximal femur axis (Fig. 2) [19]. At the distal femur, the condylar twist angle (CTA) was defined as the angle between the PCL and the clinical TEA (Fig. 5) [36]. The TSA was defined as the angle between the medial and lateral trochlear inclination lines (Fig. 6) [31]. The medial and lateral trochlear inclination angles (MTIA and LTIA) were defined as the angles between the PCL and the medial and lateral trochlear inclination line, respectively (Fig. 7) [31]. The outcome parameters and their definitions are summarised in Table 1.
Statistical analysis
All statistical analyses were carried out in IBM SPSS Statistics 20 (IBM Corp., Armonk, NY). To analyse inter-observer reliability, two observers (SW and TB) carried out the identification procedure of the landmarks in a subgroup of 20 subjects. The inter-observer reliability was determined by calculating the intraclass correlation coefficient of the final outcome parameters. The relationship between hip and knee anthropometry was analysed by comparing the FNAA, ML-offset and NSA of the proximal femur to the CTA and the TSA, MTIA and LTIA at various slices, respectively, using Pearson’s R correlation. The data were analysed for each anatomical parameter, and the mean and range values were found. A normality test was conducted, and all parameters were found to be normal (Kolmogorov–Smirnov p > 0.05), not only for the group as a whole but also per gender, so an independent samples T test was carried out for all parameters. For all statistical tests, a p value < 0.05 was considered statistically significant. The correct sample size needed to test the hypotheses was calculated using the formula described in Bonett et al. and using Fisher’s classic z-transformation [4]. The power was set at 0.8, and the alpha at 0.05. In statistics, a correlation coefficient (R) of 0.4 is considered a moderate correlation and an R of 0.5 is considered to represent a good correlation. Based on R = 0.5, a sample size of 29 subjects was needed. Because the effect of gender was one of the primary outcome parameters, at least 29 males and 29 females were needed (total 58 subjects).
Results
A total of 60 subjects were analysed, including 30 males and 30 females. The average age of the male group was 82.3 years (SD 2.4, range 80–89 years), and in the female group, this was 84.2 years (SD 2.9, range 80–90 years). Although this difference was statistically significant (p = 0.01), we did not consider this clinically relevant. Average height was 173.7 cm (SD 6.1) for males and 160.0 cm (SD 7.7) for females (p < 0.01), and average weight was 74.3 kg (SD 9.7) for males and 64.7 kg (SD 12.8) for females (p < 0.01). The diameter of the femoral head was on average 51.6 mm (SD 2.2) for males and 45.6 mm (SD 2.0) for females (p < 0.01). Regarding the outcome parameters, there was a significant gender difference in the FNAA and the TSA, LTIA and MTIA at level 2 (i.e. 5 mm proximal to the intercondylar notch centre) (Table 2).
Looking at the correlation between proximal and distal femur morphology, there was no statistically significant correlation between the CTA and either proximal femoral parameter (Table 3). However, the average CTA in a subgroup with a relatively low FNAA (lower than the total population’s average FNAA of 12.6°, n = 31, average FNAA 6.0°) was 6.4° (SD 1.2), whereas this was 7.1° (SD 1.4) in the subgroup with a FNAA higher than the total population’s average (n = 29, average FNAA 19.6°) (p = 0.03). Regarding the TSA, there was only a correlation between the TSA at level 3 and the NSA in the total group (n = 60) (p < 0.05), meaning that subjects with a larger NSA had a relative large TSA at that level. There was no correlation between this parameter in the female/male subgroups separately. The LTIA did not correlate with any proximal femoral parameter at any level. On the contrary, the MTIA did correlate with the morphology at the proximal femur. The MTIA at level 2 and 3 showed a weak correlation with the FNAA in the total group (p < 0.05), again without a correlation in the female and male subgroups. Furthermore, there was a good correlation between the MTIA on the one hand and the NSA and the ML-offset on the other hand. Subjects with a larger NSA and a smaller ML-offset had a smaller MTIA on average. This correlation was present at almost every level and was strongest and statistically significant only in females and the total group, independent of length and weight and thus solely an effect of gender.
In TKA, the margin for correct component rotation is considered to be within ±3°. A more in-depth analysis revealed that the influence of the NSA and ML-offset on the MTIA exceeded this clinical threshold of 3° on certain levels. Based on the correlation analysis, we can state that per 5° increase in NSA, the MTIA decreases 2.1°. At level 3 (i.e. 10 mm proximal to the intercondylar notch), for example, this means that the MTIA for subjects with a below average NSA (i.e. ‘coxa vara’, n = 29, mean NSA 120.1°, SD 2.9) is 3.8° higher than for subjects with an above average NSA (i.e. ‘coxa valga’, n = 31, mean NSA 128.1°, SD 3.0) (p < 0.01) (Fig. 8a). The ML-offset showed a similar result. Again, there was a linear correlation between these two parameters: for every 5 mm increase in ML-offset, there was a 2.6° increase in MTIA. At level 4 (i.e. 15 mm proximal to the intercondylar notch), for instance, the mean MTIA was 4.6° higher in the subgroup with a below average ML-offset (n = 29, mean ML-offset 41.6 mm, SD 3.0) compared to the subgroup with an above average ML-offset (n = 31, mean ML-offset 49.6 mm, SD 2.7) (p < 0.01) (Fig. 8b). Studying the effect of the FNAA in such a way did not reveal any clinical relevant difference in MTIA between subjects with a FNAA below the average versus subjects with a FNAA above the average.
The parameters describing the morphology of the proximal femur were also correlated with each other: subjects with a large NSA (i.e. coxa valga) on average had a smaller ML-offset (Pearson’s R = 0.51, p < 0.001) and a smaller FNAA (Pearson’s R = 0.36, p < 0.01).
Two observers defined the position of the landmarks on a subset of 20 subjects with an intraclass correlation coefficient of 0.99 (average difference 1.2° ± 0.7°) for the final outcome values.
Discussion
The most important finding of the present study was that all three parameters describing the morphology of the proximal femur (i.e. FNAA, NSA and ML-offset) were correlated with the medial trochlear inclination angle (MTIA) in females, while no such effect was found in males. Subjects with relatively high femoral neck anteversion, low NSA and high mediolateral offset had on average a higher MTIA, independent of length and weight. The effect of the NSA and the ML-offset on the MTIA was even larger than the clinical threshold of ±3°, frequently used to assess correct component rotation. These results not only confirm the hypothesis that a correlation exists between the morphology of the proximal femur with that of the distal femoral trochlea, but also the hypothesis that this correlation is gender specific.
Regarding the other parameters measured, we conclude that the CTA was not correlated with the FNAA in the correlation analysis. However, a subtle difference of 0.7° was observed when the total population was categorised in two groups based on a low or a high FNAA, indicating that subjects with a high FNAA had a slightly higher CTA. Nevertheless, the clinical relevance of this finding can be questioned. TSA was only correlated at the level 10 mm proximal to the intercondylar notch centre with the NSA, meaning that subjects with a relatively high NSA (i.e. coxa valga) had a greater TSA. LTIA was not correlated with any proximal femoral parameter studied.
The mean values and standard deviations for the individual parameters found in this study compare well to values reported in other studies. Across the 60 subject samples, the FNAA yielded an average of 12.6° which compares with other studies that have used a similar technique, in addition to those that have used a different technique to measure the FNAA [2, 28, 35]. The NSA and ML-offset found in the present study correspond with the values found by Maruyama et al. [19] studying the anatomy and morphology of 100 cadaveric femora: NSA 125.0° (SD 4.8), ML-offset 44.6 mm (SD 6.7); in the present study, these values were 124.2° and 45.8 mm, respectively. Regarding the CTA, our findings correspond very well with the values found by Yoshino et al. [34] (6.4°, SD 1.6), and the values from other studies summarised in their article comparing CTA values measured with CT, MRI and cadavers.
The TSA, LTIA and MTIA values are difficult to compare with previous work done by others, because there is high variation in methodology to assess the geometry of the trochlea. Van Haver et al. [31], who studied the differences in distal femur morphology between a population with trochlea dysplasia (n = 20) and healthy controls (n = 20), used a plane angled 15° caudal with the long axis of the femur and found a TSA of 150.3° (SD 4.4) in their control population. Reikeras [24] measured the TSA at a mid-patellar level and reported 145.0° (SD 10.0). Eckhoff et al. [10] described the same methodology, but did not report TSA values.
In existing literature, only a few studies have been published concerning the correlation between the morphology of the proximal femur with that of the distal femur. Weidow et al. and Boissonneault et al. studied this correlation only in the coronal plane and concluded that subjects with a higher ML-offset and a lower NSA more often had osteoarthritis of the medial compartment of the knee. In other words, a so-called coxa vara leads to a more varus hip–knee–ankle axis with degenerative changes as a consequence on the long term. On the contrary, they found that subjects with a lower ML-offset and a higher NSA (i.e. typical ‘coxa valga’) more often had osteoarthritis of the lateral compartment [3, 33]. Eckhoff et al. [10] investigated the correlation between anterior knee pain and femoral neck anteversion in a population of 20 symptomatic and 20 asymptomatic subjects. They found that femoral neck anteversion in subjects with anterior knee pain was significantly higher compared to asymptomatic subjects. They did not find any difference in trochlear morphology or configuration; however, the parameters to define this morphology were limited [10]. Reikeras [24] investigated patellofemoral characteristics in a population of 15 female patients who were evaluated for clinical symptoms of increased femoral anteversion compared to a population of 17 female control patients without symptoms. Their methodology was the same as Eckhoff et al. encompassing the same limitations and weaknesses, as well as a small study population, probably too small to detect any correlations. The CT scans used by Eckhoff et al. and Reikeras et al. were made in the supine position with the knee extended. As a consequence, the position of the patella is relatively proximal to the trochlea and the condyles. Measuring trochlear dimensions at the cranio-caudal middle of the patella in this position does not reflect the level of the trochlea where the patella usually articulates. Therefore, the results of both studies must be interpreted with caution. Takai et al. [29] studied the effect of rotational alignment of the lower limb in 43 patients with osteoarthritis of the knee and concluded that subjects with osteoarthritis of the patellofemoral compartment had a higher femoral neck anteversion angle. Lee et al. studied the effect of fixed rotation deformities of the femur on patellofemoral contact pressures in seven human cadaveric knees. They concluded that excessive internal rotation of the femur, which corresponds with a high femoral neck anteversion angle, resulted in higher contact pressures on the lateral facet of the patella. The opposite was also true: excessive external rotation of the femur (i.e. low femoral neck anteversion), resulted in higher contact pressures on the medial facet of the patella [17]. These findings can be linked to basic joint physiology, in which it is postulated that the morphology of the femoral condyles results from pressure applied by the patella throughout development [15]. The results presented in this study support the findings from others. For example, subjects with a relatively large NSA (i.e. ‘valgus hip’) appeared to have a relatively small mediolateral offset and a low femoral neck anteversion angle. This combination leads to an externally rotated leg and results in potential higher contact pressures on the medial trochlea, which in the long term might result in a flatter medial trochlear facet (i.e. low medial trochlear inclination angle).
The authors are aware of some limitations to the study and the potential for further work that this could lead to. Firstly, the age of the study population was between 80 and 90 years, often referred to as octogenarians. This population was chosen because it was investigated earlier for another study on femur morphology, and high-resolution CT scans of the complete femur were available. Although the very elderly form a rapidly growing population in which there are increasing incidences of joint replacement, it does not reflect the average age of patients undergoing TKA (on average 68 years [1]). Although age-related changes of external femoral morphology are described in children [6], we are not aware of any further age-related changes from the seventh to ninth decade of life. A second limitation was that this study used static CT scans instead of dynamic modalities to investigate the correlation between the morphology of the proximal and the distal femur. The disadvantage of using CT scans in this way is that only the static bony anatomy is analysed without the soft tissues and the dynamic situation being considered. When carrying out further investigations, a method of assessing correlations between the proximal and distal femur under dynamic situations should be used to link up with the static radiological analysis. It is only by doing this combined analysis that the true effect may be understood, as an isolated static view has limited how far the final conclusions can go regarding the relationship between the proximal and distal femur in this study. The third limitation concerns the fact that the trochlea angles were measured using CT describing the subchondral osseous anatomy rather than the cartilage as captured by MRI. However, while a study of Staubli et al. [26] quantified the thickness difference, angular measurements like in this study shall hardly be affected. A final limitation concerns the method to describe the anatomy of the trochlea. As stated above, many different methods are described, varying from an axial view of the distal femur/patella on X-rays till 3D reconstructions using CT or MRI. However, no golden standard has been described, and comparison of trochlear anatomy between studies remains difficult. Unfortunately, our version of the software program Materialise Mimics (v10) was not capable of reconstructing planes under a desired angle, as described by Van Haver et al. [31]. Therefore, we were forced to use the axial CT slices to obtain data on the morphology of the trochlea. In order to describe the anatomical features of the distal femur as accurately as possible, we measured the same parameters on four slices ranging from the level of the intercondylar notch centre (INC) to 15 mm proximal to that level. This is in contrast to the method used by Reikeras [24] and Eckhoff et al. [10] describing the morphology of the trochlea using a single level at the cranio-caudal middle of the patella.
The clinical importance of this study is that the geometry of the proximal femur has an effect on the morphology of the distal femur, in particular the medial trochlea. Excessive proximal femoral geometry, regardless of the plane in which it is present (either coronal or transverse), should therefore be noticed prior to surgery at the distal femur. In order to improve our understanding of the physiological kinematics of the knee joint and to improve the concept of kinematic knee replacement, the proximal femur seems to be a factor of clinical importance. In addition, orthopaedic surgeons treating conditions concerning the hip (varying from osteotomy to arthroplasty) should be aware of potential effects of their operations on the morphology of the distal femur on the long term. Further research is, however, needed to define the exact clinical implications of proximal femoral geometry on the biomechanical and kinematic behaviour of the distal femur. Thorough understanding of this correlation might also help to understand why some patients with an apparently successful TKA still have complaints and inferior knee function.
Conclusions
Combining the findings from previous clinical and biomechanical studies with the results presented in the current study, we conclude that the shape and configuration of the proximal femur is distinctively linked with the morphology of the distal femur. Interestingly, morphological features of the proximal femur in the coronal plane (i.e. NSA and ML-offset) appear to influence the morphology of the distal femur not only in the coronal plane (i.e. varus/valgus axis) but also in the transverse plane (e.g. trochlear morphology). These effects are more profound in females than in males and are independent of length and weight. The effect of the NSA and ML-offset on the medial trochlear inclination angle exceeds the clinical relevant threshold of 3°. This correlation has never been described before, either because of poor methodology, low study power, or simply because of focusing on a limited set of parameters instead of a more extensive analysis.
References
National Joint Registry (2013) 10th annual report 2013. National Joint Registry for England, Wales and Northern-Ireland
Bargar WL, Jamali AA, Nejad AH (2010) Femoral anteversion in THA and its lack of correlation with native acetabular anteversion. Clin Orthop Relat Res 468(2):527–532
Boissonneault A, Lynch JA, Wise BL, Segal NA, Gross KD, Murray DW, Nevitt MC, Pandit HG (2014) Association of hip and pelvic geometry with tibiofemoral osteoarthritis: Multicenter Osteoarthritis Study (MOST). Osteoarthr Cartil 22(8):1129–1135
Bonett DG, Wright TA (2000) Sample size requirements for estimating Pearson Kendall and Spearman correlations. Psychometrika 65(1):23–28
Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA (2014) Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med 7(2):89–95
Djuric M, Milovanovic P, Djonic D, Minic A, Hahn M (2012) Morphological characteristics of the developing proximal femur: a biomechanical perspective. Srp Arh Celok Lek 140(11–12):738–745
Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG (2012) Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 35(2):e160–e169
Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM (2005) Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am 87(Suppl 2):71–80
Eckhoff DG, Kramer RC, Alongi CA, VanGerven DP (1994) Femoral anteversion and arthritis of the knee. J Pediatr Orthop 14(5):608–610
Eckhoff DG, Montgomery WK, Kilcoyne RF, Stamm ER (1994) Femoral morphometry and anterior knee pain. Clin Orthop Relat Res 302:64–68
Hapa O, Muratli HH, Cakici H, Gulcek S, Aksahin E, Bicimoglu A (2009) Is there a relation between hip torsion, coverage and osteoarthritis of the knee? J Child Orthop 3(1):27–31
Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG (1993) The axes of rotation of the knee. Clin Orthop Relat Res 290:259–268
Hoshino Y, Wang JH, Lorenz S, Fu FH, Tashman S (2012) The effect of distal femur bony morphology on in vivo knee translational and rotational kinematics. Knee Surg Sports Traumatol Arthrosc 20(7):1331–1338
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471(3):1000–1007
Kapandji IA (2010) The physiology of the joints. Volume 2, The lower limb. Churchill Livingstone/Elsevier, London
Kessler O, Durselen L, Banks S, Mannel H, Marin F (2007) Sagittal curvature of total knee replacements predicts in vivo kinematics. Clin Biomech (Bristol, Avon) 22(1):52–58
Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC (1994) The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res 302:69–74
Lee YS, Oh SH, Seon JK, Song EK, Yoon TR (2006) 3D femoral neck anteversion measurements based on the posterior femoral plane in ORTHODOC system. Med Biol Eng Comput 44(10):895–906
Maruyama M, Feinberg JR, Capello WN, D’Antonio JA (2001) The Frank Stinchfield Award: morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res 393:52–65
Ollivier M, Parratte S, Lecoz L, Flecher X, Argenson JN (2013) Relation between lower extremity alignment and proximal femur anatomy. Parameters during total hip arthroplasty. Orthop Traumatol Surg Res 99(5):493–500
Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN (2013) Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc 21(10):2213–2219
Paternostre F, Schwab PE, Thienpont E (2014) The combined Whiteside’s and posterior condylar line as a reliable reference to describe axial distal femoral anatomy in patient-specific instrument planning. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-00014-02836-00165
Prevrhal S, Fox JC, Shepherd JA, Genant HK (2003) Accuracy of CT-based thickness measurement of thin structures: modeling of limited spatial resolution in all three dimensions. Med Phys 30(1):1–8
Reikeras O (1992) Patellofemoral characteristics in patients with increased femoral anteversion. Skeletal Radiol 21(5):311–313
Rubin PJ, Leyvraz PF, Aubaniac JM, Argenson JN, Esteve P, de Roguin B (1992) The morphology of the proximal femur. A three-dimensional radiographic analysis. J Bone Joint Surg Br 74(1):28–32
Staubli HU, Durrenmatt U, Porcellini B, Rauschning W (1999) Anatomy and surface geometry of the patellofemoral joint in the axial plane. J Bone Joint Surg Br 81(3):452–458
Stefanik JJ, Roemer FW, Zumwalt AC, Zhu Y, Gross KD, Lynch JA, Frey-Law LA, Lewis CE, Guermazi A, Powers CM, Felson DT (2012) Association between measures of trochlear morphology and structural features of patellofemoral joint osteoarthritis on MRI: the MOST study. J Orthop Res 30(1):1–8
Sugano N, Noble PC, Kamaric E (1998) A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr 22(4):610–614
Takai S, Sakakida K, Yamashita F, Suzu F, Izuta F (1985) Rotational alignment of the lower limb in osteoarthritis of the knee. Int Orthop 9(3):209–215
Thienpont E, Schwab PE, Paternostre F, Koch P (2014) Rotational alignment of the distal femur: anthropometric measurements with CT-based patient-specific instruments planning show high variability of the posterior condylar angle. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-00014-03086-00162
Van Haver A, De Roo K, De Beule M, Van Cauter S, Audenaert E, Claessens T, Verdonk P (2013) Semi-automated landmark-based 3D analysis reveals new morphometric characteristics in the trochlear dysplastic femur. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-00013-02573-00161
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95(5):365–372
Weidow J, Mars I, Karrholm J (2005) Medial and lateral osteoarthritis of the knee is related to variations of hip and pelvic anatomy. Osteoarthr Cartil 13(6):471–477
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y (2001) Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16(4):493–497
Yoshioka Y, Cooke TD (1987) Femoral anteversion: assessment based on function axes. J Orthop Res 5(1):86–91
Yoshioka Y, Siu D, Cooke TD (1987) The anatomy and functional axes of the femur. J Bone Joint Surg Am 69(6):873–880
Acknowledgments
This project was enabled due to the granting of a Special Experience Award by the Institution of Mechanical Engineers and funding from the University of Bath.
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Samantha J. Wright and Tim A. E. J. Boymans are joint first authors.
Rights and permissions
About this article
Cite this article
Wright, S.J., Boymans, T.A.E.J., Grimm, B. et al. Strong correlation between the morphology of the proximal femur and the geometry of the distal femoral trochlea. Knee Surg Sports Traumatol Arthrosc 22, 2900–2910 (2014). https://doi.org/10.1007/s00167-014-3343-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3343-4