Abstract
Purpose
Matrix-induced autologous chondrocyte implantation (MACI) has demonstrated effectiveness in treating isolated cartilage defects of the knee but medium- and long-term evidence and information on the management of postoperative complications or partially successful cases are sparse. This study hypothesised that MACI is effective for up to 5 years and that patients with posttreatment problems may go on to obtain clinical benefit from other interventions.
Methods
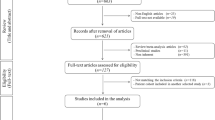
A follow-on, prospective case series of patients recruited into a previous controlled, randomised, prospective study or newly enroled. Patients were followed up 6, 12, 24 and 60 months after surgery. Outcome measures were Tegner (activity levels) and Lysholm (pain, stability, gait, clinical symptoms) scores. Zone-specific subgroups were analysed 6, 12 and 24 months postoperatively.
Results
Sixty-five patients were treated with MACI. Median Tegner score improved from II to IV at 12 months; an improvement maintained to 60 months. Mean Lysholm score improved from 28.5 to 76.6 points (±19.8) at 24 months, settling back to 75.5 points after 5 years (p > 0.0001). No significant differences were identified in the zone-specific analysis. Posttreatment issues (N = 12/18.5 %) were resolved with microfracture, debridement, OATS or bone grafting.
Conclusions
MACI is safe and effective in the majority of patients. Patients in whom treatment is only partially successful can go on to obtain clinical benefit from other cartilage repair options. This study adds to the clinical evidence on the MACI procedure, offers insight into likely treatment outcomes, and highlights MACI’s usefulness as part of an armamentarium of surgical approaches to the treatment of isolated knee defects.
Level of evidence
Prospective case control study with no control group, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cartilage defects are currently treated with a variety of surgical approaches. Osteochondral autologous grafts [8, 21, 36] are commonly used to replace the damaged cartilage but the usefulness of this technique is limited by the quantity of harvesting possible without causing donor site morbidity [34, 37]. Bone marrow stimulation techniques (abrasion, drilling and microfracture) [24, 37, 38] aim to prompt a healing response by exposing the subchondral bone marrow and creating a blood clot that allows the migration of mesenchymal stem cells. Autologous chondrocyte implantation (ACI) is a regenerative technique aiming to stimulate the production of hyaline-like cartilage repair tissue, which contains type II collagen but does not share the structure and biomechanical properties of endogenous hyaline cartilage [9].
First generation ACI techniques involved the injection of chondrocytes in liquid suspension under an autologous periosteal patch and showed successful long-term results [11, 29–31]. However, drawbacks of the technique such as periosteal hypertrophy, delamination of the defect and a demanding surgical technique led to the development of a second generation technique (ACI-C) in which a collagen membrane was used to secure the chondrocytes in the defect, negating the need for a periosteal patch [19].
Matrix-induced autologous chondrocyte implantation (MACI®, Genzyme Biosurgery, Cambridge, MA) is a third generation product in which the chondrocytes are supplied seeded onto a type I/III collagen scaffold [7, 16], which is simply secured into the defect with fibrin sealant. MACI has been shown to not only deliver comparative clinical results to traditional ACI [2, 31] but also to simplify the surgical technique, prevent periosteal hypertrophy and provide better re-differentiation of the seeded chondrocytes [7, 16, 23].
The short-term effectiveness of MACI has been reported in several single-armed and controlled studies [1–4, 7]. After first being introduced to Giessen University Hospital in 1999, MACI was compared to microfracture in a controlled, randomised, prospective study, which showed superior clinical results in the MACI group [4]. Subsequently, patients from that study, plus additional recruits, were enroled into the current follow-on, prospective case series study which hypothesised that MACI offers long-term symptomatic improvement, clinical improvement is independent of defect location and that additional techniques could be used to improve the clinical outcome of patients achieving only partial success with MACI treatment.
Materials and methods
The study was conducted at Giessen University Hospital between 2000 and 2010 and was open to patients of either gender aged ≥18 and ≤50 years with a single, posttraumatic, isolated, symptomatic chondral defect (3–10 cm2) of the femoral condyle or patella.
This prospective case series followed a previous prospective, controlled, randomised study comparing MACI with microfracture [4]. The decision to continue enrolment and undertake a larger, single-arm MACI study was based on the results of the controlled study, which showed significantly better clinical scores in the MACI group compared to microfracture in defects larger than 3.5 cm2.
Exclusion criteria included the presence of chronic inflammatory arthritis, instability of the knee joint, prior or planned subtotal meniscectomy (>30 % of the meniscus), BMI > 30, varus (>3°) or valgus (>5°) abnormality, osteonecrosis, osteoarthritis, untreated patellar malalignment and chondrocalcinosis. The treatment of concomitant meniscus lesions during treatment was permitted, assuming that the meniscus could be largely preserved.
Patients were followed up 6, 12, 24 and 60 months after surgery for the evaluation of efficacy and safety. Outcome measures were the Tegner (activity levels) and Lysholm (pain, stability, gait, clinical symptoms) scores [39]. Subgroups for medial femoral condyle (MFC), lateral femoral condyle (LFC) and patellar-trochlear region (PT) were formed to enable a zone-specific comparison of outcomes. These comparisons were performed at 6, 12 and 24 months only as at 60 months the groups were statistically underpowered.
Operative technique
For consistency of quality and technique, all surgical procedures were performed at the same clinic by the same surgeon.
Treatment with MACI was performed in two stages. First, a cartilage biopsy was harvested and sent for culturing. Four to six weeks later, the chondrocyte-seeded collagen scaffold was implanted via mini-arthrotomy. Patients in the PT group with minor patellar malalignment (diagnosed clinically, arthroscopically or radiologically) were either excluded, treated successfully prior to implantation or, where necessary, treated with soft tissue realignment (loose reattachment of the lateral retinaculum) during MACI implantation. No patients were recruited into the study with pathological Q-angles requiring tubercle osteotomy, MPFL-insufficiency requiring soft tissue reconstruction, or varus/valgus deformities requiring realignment.
During surgery, the defect was prepared by removing all fibrous tissue, cartilage fragments and calcifying cartilage layer until the subchondral bone plate was exposed. Once sharp, vertical walls of healthy cartilage of normal thickness were achieved around the defect, the subchondral bone plate was checked to ensure that it was completely intact and free of fibrous tissue and bleeding.
A template of the defect was made from sterile aluminium foil and used to cut the MACI membrane to size (Fig. 1). The implant was placed into the defect cell side down, facing the subchondral bone, and affixed with fibrin sealant (Fig. 2). No supplemental fixation with sutures was necessary. The treated knee was moved through a full range of motion to ensure the security of the implant prior to closure.
Rehabilitation
Patients were required to follow a postoperative rehabilitation programme which included a dorsal plaster cast (10° flexion) for 2 days postoperatively (to prevent uncontrolled flexion which might increase the risk of implant delamination), followed by continuous passive motion, physiotherapy, and 8 weeks of partial weight bearing (10 kg) on crutches. In the PT group, partial weight bearing was limited to 3 weeks. Patients also received anti-thrombotic prophylaxis with low molecular weight heparin certoparin-natrium (Monoembolex s.c. 1 per day) for the entire period of partial weight bearing.
Ethical approval
Both studies were approved by the Ethics Committee of Giessen University Hospital (Ethik-Kommission Justus-Liebig Universität Giessen) reference 106/10.
Statistical methods
A fully nonparametric rank method [12] was used to analyse the time courses of each of the scores. This allowed a unified longitudinal inferential analysis of the ordinal outcome measures and for the (quasi-) metric scores (Tegner and Lysholm). All available data (not just those from patients with complete records) were used as missing values could be considered ‘missing completely at random’. All statistical analyses were performed using the statistics software R, version 2.8.0 (2008-10-20) [33] including the Matrix [5] and MASS [41] packages.
Results
Sixty-five patients were included in the prospective case series. Mean patient age was 32(±9) years, and mean BMI was 24(±3) kg/m2. Onset of symptoms, cartilage defect location and gender disposition are shown in Table 1.
Follow-up was completed on all 65 patients (100 %) at 6 months, 61 patients (93.8 %) at 12 and 24 months, and 25 patients (38.5 %) at 60 months (due to losses to follow-up and patients not yet reaching 5 years postoperatively or the 5-year follow-up visit). The Lysholm score (mean/median) improved from 51.9/52.0 preoperatively to 84.7/90.0 at 6 months, 90.0/93.0 at 12 months, 88.1/94.0 at 24 months and 85.4/95.0 at 60 months (Fig. 3). The median Tegner score improved from II preoperatively to III at 6 months, IV at 12 months and then remained at IV at 24 and 60 months. Both scores showed a sharp improvement within the first 6 months, improvement was significant (p = 0.0001) at all follow-up intervals compared to baseline, and the maximum symptomatic relief achieved was sustained to the 60-month follow-up.
Zone-specific results (subgroup analysis)
The 6, 12 and 24 month data were analysed for differences in zone-specific treatment outcomes (Table 2). Due to the small numbers of patients in each subgroup and the relative dominance of the MFC subgroup (see Table 1), it was not possible or desirable to draw any conclusions from this analysis and there was no significant difference between the three subgroups for Tegner or Lysholm scores.
Management of postoperative problems
As with all surgical techniques, the management of postoperative symptoms requiring further treatment, and MACI treatment failures, must be evaluated. Twelve patients (18.5 %) developed symptoms such as persistent pain, locking, crepitus or recurrent effusion between 6 and 36 months, underwent second-look arthroscopy or MRI evaluation and were treated with a range of different techniques (Table 3).
Two years after MACI implantation, three implants showed mostly integrated regenerative tissue but with some nonintegrated areas at the border with the surrounding cartilage. We interpreted these as being areas of less robust regenerative tissue or areas of disintegration of the adjacent cartilage. These small lesions were treated with debridement and microfracture. Two patients with small diameter (1–2 cm2) disintegration of the regenerated tissue and subchondral plate defects (cysts) 1 year postimplantation were treated with OATS. Two patients with persistent, painful, deep subchondral oedema, but intact regenerated cartilage tissue and subchondral bone plate, received a retrograde subchondral bone graft from the iliac crest.
In four patients treated for patellar site defects, symptomatic graft fibrillation without marked hypertrophy was observed at 12 months and treated successfully with arthroscopic debridement.
In one patient, MACI was implanted in a medial condyle defect after failed ACI. Twelve months postoperatively, there was a rapid increase in deep pain in the femoral condyle and osteoarthritic symptoms. This patient was classified as a treatment failure and went on to be treated successfully with unicondylar medial compartment knee resurfacing, achieving excellent clinical scores for up to 3 years subsequently. Any recurrent effusion and/or local pain in the scar region immediately postimplantation resolved spontaneously within 3 months.
Discussion
The results of this prospective, single-centre case series of 65 patients with isolated knee cartilage defects treated with MACI, with 61 two-year and 25 five-year follow-ups, confirm MACI as an appropriate treatment option. They suggest that defect location does not influence treatment outcome and demonstrate that patients who do not achieve adequate or sustained clinical benefit from treatment with MACI can go on to benefit from other interventions.
The results show statistically significant improvements in outcomes at 6, 12 and 24 months postoperatively. Although the high loss to follow-up rate at 5 years limits their value, the data suggest that these clinical improvements may be sustained for up to 60 months and add weight to the growing body of evidence showing successful medium- and long-term results with cell-based cartilage repair techniques.
Peterson et al. followed up ACI patients (N = 224) for 10–20 years and reported successful clinical outcomes, especially in isolated defects, though multiple lesions and patellar site lesions showed smaller improvements in clinical scores.
MACI has previously been shown to offer successful short-term outcomes in the treatment of knee cartilage defects [4, 20, 35, 40]. The first five-year retrospective case series of MACI patients (N = 15) reported that 58 % of patients experienced satisfactory results [6]. Another multicentre case study (N = 41) reported satisfactory and improved ratings from 98 and 86 % of patients, respectively, during 5 years of follow-up, concluding that MACI is a useful medium-term treatment option [13].
There is scant information in the literature enabling comparison and definition of problems after MACI implantation. According to a systematic review, ACI showed a failure rate between 1.5 and 7.7 %, with the highest rates in periosteal-covered ACI and the lowest with MACI [22]. Periosteal hypertrophy was commonly reported after first generation ACI [10, 26, 28, 32] but MACI’s resorbable membrane negates the need for a periosteal flap, and therefore, this problem has not been observed in these, or other [27, 42], studies using MACI. Some patients in the current study showed minor symptomatic graft fibrillation without marked hypertrophy solely in patellar locations, which suggests shear forces may affect graft growth.
Symptoms that required further treatment and treatment failures could both be addressed with a variety of alternative surgical procedures. Retrograde bone grafting, or revision MACI after ACI, has to be categorised as salvage procedures, especially in the knowledge that failed cartilage repair is often followed by early osteoarthritic changes. The correlation of postoperative clinical symptoms with changes in the subchondral bone highlighted the vital role that subchondral bone plays in the success of cartilage repair treatments [18]. The method of replacing pathologic subchondral bone with autologous grafts confirms that chondral repair is likely to fail without a viable subchondral bed. Depending on the age of the patient resurfacing or osteotomy can also successfully complement partially successful cartilage regeneration. Except for the one reported patient where joint resurfacing was necessary, all other posttreatment complications in the current study could be addressed with biologic joint sparing techniques.
There is consensus in the literature that MACI represents a safe and effective regenerative technique in isolated cartilage defects larger than 3 cm2 [4, 14, 35, 40, 43] but it has been difficult to correlate the clinical and macroscopic appearance of regenerative tissue closely with the histological outcomes [15]. Although their usefulness is limited by the small sample size of the subgroups studied, the results of the present study, which focuses on the functional status of a comparatively high number of patients, are in agreement with this consensus and add to the existing evidence [6, 13, 17, 25]. They also offer insight into medium-term (5 years) effectiveness, zone-specific outcomes and the successful management of posttreatment complications and treatment failures.
Conclusion
This study shows that the treatment of isolated knee cartilage defects with MACI is safe and effective in the majority of patients, with clinical scores showing significant improvement at 2 years and some results suggesting clinical benefit continuing for up to 5 years. Patients in whom treatment was only partially successful can go on to obtain clinical benefit from other cartilage repair options. This study adds to the body of clinical evidence on the MACI procedure, offers insight into likely treatment outcomes, and highlights MACI’s usefulness as part of an armamentarium of surgical approaches to the treatment of isolated knee defects.
References
Bachmann G, Basad E, Lommel D, Steinmeyer J (2004) MRI in the follow-up of matrix-supported autologous chondrocyte transplantation (MACI) and microfracture. Radiologe 44(8):773–782
Bartlett W, Skinner JA, Gooding CR, Carrington RW, Flanagan AM, Briggs TW, Bentley G (2005) Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee. J Bone Joint Surg Br 87(5):640–645
Bartlett W, Krishnan SP, Skinner JA, Carrington RWJ, Briggs TWR, Bentley G (2006) Collagen-covered versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a comparison of tourniquet times. Eur J Ortho Surg Traumatol 16:315–317
Basad E, Ishaque B, Bachmann G, Stürz H, Steinmeyer J (2010) Matrix-induced autologous chondrocyte implantation versus microfracture in the treatment of cartilage defects of the knee: a 2-year randomised study. Knee Surg Sports Traumatol Arthrosc 18(4):519–527
Bates D, Maechler M. Matrix: sparse and dense matrix classes and methods. R package version 0.999375-16. http://cran.r-project.org/
Behrens P, Bitter T, Kurz B, Russlies M (2006) Matrix-associated autologous chondrocyte transplantation/implantation (MACT/MACI)—5-year follow-up. Knee 13(3):194–202
Behrens P, Ehlers EM, Köchermann KU, Rohwedel J, Russlies M, Plötz W (1999) [New therapy procedure for localized cartilage defects. Encouraging results with autologous chondrocyte implantation]. MMW Fortschr Med 141(45):49–51
Bobic V (1999) Autologous osteo-chondral grafts in the management of articular cartilage lesions. Orthopade 28(1):19–25
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331(14):889–895
Brittberg M, Peterson L, Sjögren-Jansson E, Tallheden T, Lindahl A (2003) Articular cartilage engineering with autologous chondrocyte transplantation. A review of recent developments. J Bone Joint Surg Am 85-A(Suppl 3):109–115
Browne JE, Anderson AF, Arciero R, Mandelbaum B, Moseley JB, Micheli LJ, Fu F, Erggelet C (2005) Clinical outcome of autologous chondrocyte implantation at 5 years in US subjects. Clin Orthop Relat Res 436:237–245
Brunner E, Langer F (2000) Nonparametric analysis of ordered categorical data in designs with longitudinal observations and small sample sizes. Biom J 42(6):663–675
Ebert JR, Robertson WB, Woodhouse J, Fallon M, Zheng MH, Ackland T, Wood DJ (2011) Clinical and magnetic resonance imaging-based outcomes to 5 years after matrix-induced autologous chondrocyte implantation to address articular cartilage defects in the knee. Am J Sports Med 39(4):753–763
Ebert JR, Fallon M, Ackland TR, Wood DJ, Janes GC (2012) Arthroscopic matrix-induced autologous chondrocyte implantation: 2-year outcomes. Arthroscopy 28(7):952–964
Enea D, Cecconi S, Busilacchi A, Manzotti S, Gesuita R, Gigante A (2012) Matrix-induced autologous chondrocyte implantation (MACI) in the knee. Knee Surg Sports Traumatol Arthrosc 20(5):862–869
Fuss M, Ehlers EM, Russlies M, Rohwedel J, Behrens P (2000) Characteristics of human chondrocytes, osteoblasts and fibroblasts seeded onto a type I/III collagen sponge under different culture conditions. A light, scanning and transmission electron microscopy study. Ann Anat 182(4):303–310
Gobbi A, Kon E, Berruto M, Filardo G, Delcogliano M, Boldrini L, Bathan L, Marcacci M (2009) Patellofemoral full-thickness chondral defects treated with second-generation autologous chondrocyte implantation: results at 5 years’ follow-up. Am J Sports Med 37(6):1083–1092
Gomoll AH, Madry H, Knutsen G, van Dijk N, Seil R, Brittberg M, Kon E (2010) The subchondral bone in articular cartilage repair: current problems in the surgical management. Knee Surg Sports Traumatol Arthrosc 18(4):434–447
Gooding CR, Bartlett W, Bentley G, Skinner JA, Carrington R, Flanagan A (2006) A prospective, randomised study comparing two techniques of autologous chondrocyte implantation for osteochondral defects in the knee: periosteum covered versus type I/III collagen covered. Knee 13(3):203–210
Goyal D, Goyal A, Keyhani S, Lee EH, Hui JH (2013) Evidence-based status of second- and third-generation autologous chondrocyte implantation over first generation: a systematic review of level I and II studies. Arthroscopy 29(11):1872–1878
Hangody L, Vásárhelyi G, Hangody LR, Sükösd Z, Tibay G, Bartha L, Bodó G (2008) Autologous osteochondral grafting–technique and long-term results. Injury 39(Suppl 1):S32–S39
Harris JD, Siston RA, Brophy RH, Lattermann C, Carey JL, Flanigan DC (2011) Failures, re-operations, and complications after autologous chondrocyte implantation—a systematic review. Osteoarthritis Cartilage 19(7):779–791
Jagiello MJ, Rogers B, Briggs TWR (2007) Sequential outcome improvement following autologous chondrocyte implantation—7 year follow-up Podium presentation (no. 182) at the American Academy of Orthopaedic Surgeons, 14th—18th February 2007, San Diego, USA
Johnson LL (2001) Arthroscopic abrasion arthroplasty: a review. Clin Orthop Relat Res 391(Suppl):S306–S317
Kon E, Di Martino A, Filardo G, Tetta C, Busacca M, Iacono F, Delcogliano M, Albisinni U, Marcacci M (2011) Second-generation autologous chondrocyte transplantation: MRI findings and clinical correlations at a minimum 5-year follow-up. Eur J Radiol 79(3):382–388
Minas T, Gomoll AH, Rosenberger R, Royce RO, Bryant T (2009) Increased failure rate of autologous chondrocyte implantation after previous treatment with marrow stimulation techniques. Am J Sports Med 37(5):902–908
Nehrer S, Dorotka R, Domayer S, Stelzeneder D, Kotz R (2009) Treatment of full-thickness chondral defects with hyalograft C in the knee: a prospective clinical case series with 2 to 7 years’ follow-up. Am J Sports Med 37(Suppl 1):81S–87S
Niemeyer P, Pestka JM, Kreuz PC, Erggelet C, Schmal H, Suedkamp NP, Steinwachs M (2008) Characteristic complications after autologous chondrocyte implantation for cartilage defects of the knee joint. Am J Sports Med 36(11):2091–2099
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med 30(1):2–12
Peterson L, Minas T, Brittberg M, Lindahl A (2003) Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am 85-A(Suppl 2):17–24
Peterson L, Minas T, Brittberg M, Nilsson A, Sjögren-Jansson E, Lindahl A (2000) Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res 374:212–234
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38(6):1117–1124
R Development Core Team (2008) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, http://www.r-project.org
Reddy S, Pedowitz DI, Parekh SG, Sennett BJ, Okereke E (2007) The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med 35(1):80–85
Saris DB, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, Luyten F, TIG/ACT/01/2000&EXT Study Group (2009) Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 Months in a randomized trial compared to microfracture. Am J Sports Med 37(Suppl 1):10S–19S
Schnettler R, Horas U, Meyer C (2008) Autologous osteochondral transplants. Orthopade 37(8):734–742
Steadman JR, Rodkey WG, Briggs KK (2002) Microfracture to treat full-thickness chondral defects: surgical technique, rehabilitation, and outcomes. J Knee Surg 15(3):170–176
Steadman JR, Rodkey WG, Briggs KK, Rodrigo JJ (1999) The microfracture technic in the management of complete cartilage defects in the knee joint. Orthopade 28(1):26–32
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Vavken P, Samartzis D (2010) Effectiveness of autologous chondrocyte implantation in cartilage repair of the knee: a systematic review of controlled trials. Osteoarthr Cartil 18(6):857–863
Venables WN, Ripley BD (2003) Modern applied statistics with S. Springer, New York. ISBN 978-0387954578
Zeifang F, Oberle D, Nierhoff C, Richter W, Moradi B, Schmitt H (2010) Autologous chondrocyte implantation using the original periosteum-cover technique versus matrix-associated autologous chondrocyte implantation: a randomized clinical trial. Am J Sports Med 38(5):924–933
Zheng MH, Willers C, Kirilak L, Yates P, Xu J, Wood D, Shimmin A (2007) Matrix-induced autologous chondrocyte implantation (MACI): biological and histological assessment. Tissue Eng 13(4):737–746
Acknowledgments
The authors would like to thank Dr. Gerrit Eichner for his assistance with the statistical analysis.
Conflict of interest
The lead author received a grant from Genzyme Biosurgery (a Sanofi company) for statistical analysis and medical writing services. The other authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Basad, E., Wissing, F.R., Fehrenbach, P. et al. Matrix-induced autologous chondrocyte implantation (MACI) in the knee: clinical outcomes and challenges. Knee Surg Sports Traumatol Arthrosc 23, 3729–3735 (2015). https://doi.org/10.1007/s00167-014-3295-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3295-8