Abstract
Purpose
There is only one prospective randomized trial on acute primary patellar dislocation in adolescents comparing the long-term outcome after conservative versus operative procedures. Therefore, the long-term outcome, patellar redislocation rate, and functional outcome after conservative versus operative procedures were investigated in a prospective randomized study.
Methods
Initially, 36 patients with acute primary patellar dislocation were prospectively randomized to conservative (n = 20) versus operative procedures (n = 16) and 30 of them (83 %), 15/20 with conservative and 15/16 with operative procedures, were reached for a follow-up interview 6 years after primary procedure.
Results
Baseline and clinical parameters were similar in the two groups. The prevalence of patellar redislocation rate at 3 and 6 years after primary procedure was higher in the conservative group (7/20, 35 %, 3 years and 11/15, 73 %, 6 years) versus in the operative group (0/16, 0 %, 3 years and 5/15, 33 %, 6 years) (p = 0.02). The knee function was slightly better 6 years after primary treatment in the operative group than in the conservative group. Most patients in both groups had excellent or good knee function at 6-year follow-up, but four patients (4/15, 27 %) in conservative group and two patients (2/15, 13 %) in operative group had poor knee function at 6-year follow-up. Four patients in conservative group (4/15, 27 %) and two patients in the operative group (2/15, 13 %) were unsatisfied with the procedure at 6-year follow-up.
Conclusions
In conclusion, the results suggest that both conservative and operative procedures are feasible options for treatment of acute primary patellar dislocation in adolescents. A new finding with clinical relevance in the present work is a significantly higher redislocation rate in conservative group compared to operative group after 6-year follow-up in acute primary patellar dislocation in adolescents.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute primary patellar dislocation is a common surgical condition among the Western population with peak incidence at the age of 15 years [2, 6, 8, 12, 16, 17, 20]. The incidence rate of the primary patellar dislocation is 6/100,000 [12, 20] and reaches up to 29 in 100,000 in the group of patients aged between 10 and 17 and in females, the incidence rate is 104 in 100,000 per year [16, 18]. Palmu et al. [15] reported the incidence of acute primary patellar dislocation in the urban population in Finland been 43/100,000 for those under 16 years of age. The recent prospective randomized trials on acute primary patellar dislocation [7, 12, 14, 16, 18, 20] have involved mainly adult patient populations and have demonstrated that both conservative and operative procedures could be feasible options for treatment of acute primary patellar dislocation. To our knowledge, there is only one prospective randomized trial on acute primary patellar dislocation in adolescents comparing the long-term outcome after conservative versus operative groups [15]. Therefore, the present study was conducted with the aim to investigate the long-term outcome, patellar redislocation rate, and functional outcome in conservative versus operative groups in adolescents in a prospective randomized study. The study’s hypothesis was to compare conservative and operative groups for treatment of acute primary patellar dislocation. A new design with clinical relevance in the present work is an assessment of long-term outcome after conservative versus operative procedures in acute primary patellar dislocation in adolescents.
Materials and methods
Thirty-six adolescents with acute primary patellar dislocation were randomly allocated to undergo either conservative treatment (conservative group) (n = 20) or operative treatment (operative group) (n = 16). The inclusion criteria for the 36 patients were as follows: acute primary patellar dislocation, no previous history of knee surgery or substantial knee injury, no tibiofemoral ligamentous injury requiring surgery and no osteochondral fragments requiring fixation. We did not enroll any patients with the knee trauma and the osteochondritic lesions. The flowchart of the study is presented in Fig. 1.
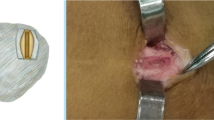
Conventional AP, side and skyline view radiographs were taken; the patellofemoral radiological parameters—patellofemoral angle, lateral patellar displacement and tilt—were measured, and the mean values were determined. Acute primary patellar dislocation diagnosis was confirmed by the ability to dislocate and lock the patella laterally under anesthesia. The degree of patellar instability was graded both clinically and arthroscopically according to Fulkerson classification [9]: (1) type I—patellar instability alone; (2) type II—patellar instability and tilt; (3) type III—patellar tilt alone; (4) type IV—malalignment. The patients with Fulkerson type I instability (n = 3) underwent lateral retinacula release (LLR) and the patients with Fulkerson types II, III and IV underwent modified Roux–Goldwaithe (RG) procedure (n = 13), which is a combination of proximal and distal realignment with LRR and medial imbrications. A midline incision with a subcutaneous lateral release was performed, a distal third of the vastus lateralis tendon was released, and the incision was extended obliquely along the superolateral edge of the muscle. The patellar tendon was split longitudinally, and the lateral half was detached from the tibial tubercle, brought medially underneath the intact medial half and sutured into the subperiostieal pocket beneath the pes anserinus insertion. The medial retinacula band was detached posteriorly, brought proximally up to the level of the vastus medialis muscle, pulled laterally through the tunnel across the distal quadriceps tendon and pulled back over to the medial side where it was anchored to the medial capsule. The knee was flexed to 30° angle to check the tightness of the reconstruction, and the medial retinacula were closed.
All patients were put on a brace allowing 30° flexion for 3 weeks and 90° flexion for the next 3 weeks. All study patients had conventional lateral patellar support-Rehab-brace. The rehabilitation protocol was the same for both groups including 1–2 visits physiotherapy per month for 6 months. The rehabilitation therapy was instructed for all patients as follows: full range of joint movement was allowed; strengthening of quadriceps muscle was done with first isometric exercises; and after, the knee motion was free of pain; and isokinetic exercises were started. Physiotherapy took at least 3 weeks and all the patients got written instructions for home exercises. The brace was removed after 6 weeks, and the patients were encouraged full range of motion. Full weight bearing was allowed from the start. The patients were followed up in the Department of Pediatric Surgery at 3, 6, 12 and 24 months. A clinical and functional assessment was done at 36 months and a functional assessment was done by questionnaire in a telephone interview at 72 months.
IRB approval
This study was carried out in Kuopio University Hospital in a 24-month period from 1998 to 2000 in accordance with the Declaration of Helsinki principles, and the protocol was approved by the Research Ethics Committee of Hospital District of Northern Savo, Kuopio, Finland (approval number 60//97, April 3, 1997). The legal guardians provided an informed consent and the adolescents were assented.
Statistical analysis
The sample size calculation was based on the redislocation rate, and in order to show a significant difference (40 %) in the redislocation rate between two groups, 15 patients per group were required at a study power of 0.6 and two-sided alpha level of 0.0278 to show a statistically significant difference between the two groups. The data were stored and analyzed with the Statistical Package for the Social Sciences (IBM SPSS Statistics 19.0, IBM Corporation., Somers, NY, USA). Bonferroni-type false discovery rate procedure was used to adjust the p values for multiple comparisons. A Student’s t test was used to evaluate demographic characteristic between the conservative group and the operative group. Linear mixed model (random intercept model) with the main effect factor being the treatment group (conservative treatment versus operative treatment for the patients) was used to compare treatment across the groups. A p value of 0.05 or lower was considered as statistically significant.
Results
The baseline demographic (Table 1), clinical and radiographic characteristics (Table 2) were similar in the two groups. There were no intraoperative complications in the operative group neither in patients in the conservative group. In the operative group, there were three minor postoperative complications: One patient developed a superficial wound infection and underwent local debridement with success; one patient get dermatitis of surgical dressing, and it was successfully treated with antihistamine; and one patient developed a peroneal palsy due to the tight brace, and she was treated with peroneal splint and physiotherapy and she recovered completely after 6 months treatment.
The prevalence of patellar redislocation rate at 3 years after primary procedure was lower in the operative group (0/16, 0 %, 3 years) versus in the conservative group (7/20, 35 %, 3 years) (p = 0.03). The prevalence of patellar reoperation (the reoperation in the operative group) rate at 3 years after primary procedure was slightly lower in the operative group (0/16, 0 %, 3 years) versus in the conservative group (5/20, 25 %, 3 years) (n.s.). At 6 years, there were 15 patients in the operative group and 15 patients in the conservative group for analysis. The prevalence of patellar redislocation rate at 6 years after primary procedure was significantly lower in the operative group (5/15, 33 %, 6 years) versus in the conservative group (11/15, 73 %, 6 years) (p = 0.02). The prevalence of patellar reoperation rate 6 years after primary procedure was slightly higher in the conservative group (27 %, 4/15) versus patellar reoperation rate in the operative group (0 %, 0/15) (n.s.). All patients (n = 4) with patellar reoperation in the conservative group underwent RS procedure. The functional outcome was slightly better 6 years after primary treatment in the operative group than in the conservative group. Most patients in both groups had excellent or good knee function at 6-year follow-up, but four patients (4/15, 27 %) in conservative group and two patients (2/15, 13 %) in operative group had poor knee function at 6-year follow-up (n.s.) (Table 1). Four patients in conservative group (4/15, 27 %) and two patients in the operative group (2/15, 13 %) were unsatisfied with the procedure at 6-year follow-up (n.s.) (Table 1).
Discussion
The most important finding of the present study was that both conservative and operative procedures are feasible options for treatment of acute primary patellar dislocation. The present study showed a slightly better long-term outcome after primary operative treatment of acute primary patellar dislocation in adolescents. Only a few studies have reported the long-term prevalence of patellar redislocation rate after conservative versus operative treatment protocols. In the present 6-year follow-up study, there were sixteen patients with patellar redislocation (11/15 in conservative group versus 5/15 in operative group) and the results indicate, in accordance with some previous studies, that patellar redislocations are common even after 6 years after acute primary patellar dislocation. In the present study, LLR procedure appeared to be effective in all patients with Fulkerson type I acute primary patellar dislocation and in Fulkerson types II–IV dislocation the RG procedure had 40 % failure rate in 6-year follow-up.
Stefancin et al. [21], Frosch et al. [8], Hing et al. [12] and Smith et al. [20] searched MEDLINE, Cochrane and EMBASE for studies on conservative and operative treatment after patellar dislocation, and four prospective randomized studies cited in the literature of conservative versus operative treatment after acute primary patellar dislocation were found and reviewed. Nikku et al. [14] randomized 127 patients with acute primary patellar dislocation either to conservative (n = 57) or operative (n = 70) group. In the operative group, the procedure consisted of proximal realignment operation; 63 patients had repair of the medial retinaculum and 54 patients of these had LLR procedure. All patients were reevaluated 7 years after primary treatment, and Nikku et al. [14] found that operative treatment of acute primary patellar dislocation does not improve the outcome, and on the basis of their study, they do not recommend the proximal realignment surgery for the patients with acute primary patellar dislocation. In another 7-year study, Sillanpää et al. [18] found in a prospective randomized trial of 40 young adults with a median age of 20 years (range 19–22 years) with acute primary patellar dislocation that the only significant difference was a lower rate of patellar redislocation rate in the operative group. However, no clear subjective benefits of initial stabilizing surgery were seen after 7-year follow-up. Christiansen et al. [7] randomized eighty patients with acute primary patellar dislocation to conservative or operative groups. Their operative procedure consisted of surgical reinsertion of the medial patellofemoral ligament to the adductor tubercle (MPFL). In 2-year follow-up, Christiansen et al. [7] found no significant difference (n.s.) in patellar redislocation rate between the conservative (patellar redislocation rate, 20 %) and operative (patellar redislocation rate, 17 %) groups after 2-year follow-up. Palmu et al. [15] gathered prospectively a cohort of 74 acute primary patellar dislocations in 71 patients younger than 16 years. Sixty-four knees were randomized to conservative group (n = 28 knees) or operative group (n = 36 knees). Their operative procedure consisted primary repair of the medial structures (n = 29 knees) or lateral release alone (LLR) (n = 7 knees). All but four patients had a concomitant LLR. The rehabilitation protocol was the same for both groups. The patients were seen at 2 years, a telephone interview was conducted at a mean of 14 years after primary treatment in 2008, and they found no significant difference in patellar redislocation rate between the conservative (patellar redislocation rate, 20/28, 71 %) and operative (patellar redislocation rate, 24/36, 67 %) groups. On the basis of their study, they conclude that immediate direct repair of the medial structures with LLR procedure does not improve the long-term outcome of the patients with acute primary patellar dislocation.
Frosch et al. [8] reviewed the nonrandomized studies on conservative and operative treatment after patellar dislocation, and three studies cited in the literature of conservative versus operative treatment after acute primary patellar dislocation showed no clear subjective benefits of operative versus conservative treatment protocols [4, 6, 11].
Harilainen and Sandelin [10] reported that patient satisfaction did correlate with redislocation, and in our study, most of the patients in both groups were satisfied with the procedure and had good or excellent knee function at 6-year follow-up. One limitation of the present study, from the methodological point of view, is the small sample size of 30 analyzed patients. However, this research question is quite specific, and therefore, we did not expect high number of patients and this could be taken in account in planning new scientific studies in the future. Future studies are also recommended to address the outcomes of medial patellofemoral ligament reconstruction for patellar instability in adolescents [3, 5, 19]. In the meta-analysis, Smith et al. [20] found that operative management of first patellar dislocation is associated with a significantly lower risk of subsequent patellar dislocation compared with non-surgical management, but a significantly higher risk of patellofemoral osteoarthritis. The current concepts on anatomy and biomechanics of patellar instability should be taken account in planning operative procedure for future trials [1, 13]. A new finding with clinical relevance in the present work is a significantly higher redislocation rate in conservative group compared to operative group after 6-year follow-up in acute primary patellar dislocation in adolescents.
Conclusion
In conclusion, the results suggest that both conservative and operative procedures are feasible options for treatment after acute primary patellar dislocation. A new finding with clinical relevance in the present work is a significantly higher redislocation rate in conservative group compared to operative group after 6-year follow-up.
References
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sport Med Arthrosc 15:48–56
Beasley LS, Vidal AF (2004) Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr 16:29–36
Bitar AC, Demange MK, D’Elia CO, Camanho GL (2012) Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 40:114–122
Buchner M, Baudendistel B, Sabo O, Schmitt H (2005) Acute traumatic primary patellar dislocation: longterm results comparing conservative and surgical treatment. Clin J Sport Med 15:62–66
Camanho GL, de Viegas AC, Bitar AC, Demange MK, Hernandez AJ (2009) Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 25:620–625
Cash JD, Hughston JC (1988) Treatment of acute patellar dislocation. Am J Sports Med 16:244–249
Christiansen SE, Jakobsen BW, Lund B, Lind M (2008) Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 24:82–87
Frosch S, Balcarek P, Walde TA, Schuttrumpf JP, Wachowski MM, Ferleman K-G et al (2011) The treatment of patellar dislocation: a systematic review. Z Orthop Unfall 149:630–645
Fulkerson JP, Schutzer SF, Ramsby GR, Bernstein RA (1987) Computerized tomography of the patellofemoral joint before and after lateral release or realignment. Arthroscopy 3:19–24
Harilainen A, Sandelin J (1993) Prospective long-term results of operative treatment in primary dislocation of the patella. Knee Surg Sports Traumatol Artrosc 1:100–103
Hawkins RJ, Bell RH, Anisette G (1986) Acute patellar dislocations. The natural history. Am J Sports Med 14:117–120
Hing CB, Smith TO, Donell S, Song F (2012) Surgical versus non-surgical interventions for treating patellar dislocation (review). Cochrane Database Syst Rev 11:CD008106. doi:10.1002/14651858
Nakagawa K, Wada Y, Minamide M, Tsuchiya A, Moriya H (2002) Deterioration of long-term clinical results after the Elmslie–Trillat procedure for dislocation of the patella. J Bone Jt Surg (Br) 84:861–864
Nikku R, Nietosvaara Y, Aalto K, Kallio PE (2005) Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop Scand 76:699–704
Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y (2008) Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Jt Surg (Am) 90:463–470
Panni AS, Vasso M, Cerciello S (2013) Acute patellar dislocation. What to do? Knee Surg Sports Traumatol Artrosc 21:275–278
Runow A (1983) The dislocating patella: etiology and prognosis in relation to generalized joint laxity and anatomy of the patellar articulation. Acta Orthop Scand Suppl 201:1–53
Sillanpää PJ, Mattila VM, Mäenpää H, Kiuru M, Visuri T, Pihlajamäki H (2009) Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Jt Surg (Am) 91:263–273
Smith TO, Walker J, Russell N (2007) Outcomes of medial patellofemoral ligament reconstruction for patellar instability in adolescents: a systematic review. Knee Surg Sports Traumatol Artrosc 15:1301–1314
Smith TO, Song F, Donell S, Hing CB (2011) Operative versus non-operative management of patellar dislocation: a meta-analysis. Knee Surg Sports Traumatol Artrosc 19:988–998
Stefancin JJ, Parker RD (2007) First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 455:93–101
Acknowledgments
We thank Mrs Eeva Oittinen for the technical assistance. This work has been financially supported by EVO Grant from the Hospital District of Northern Savo, Finland.
Conflict of interest
Authors have no conflict of interest, and they have full control of all primary data. Authors allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Regalado, G., Lintula, H., Kokki, H. et al. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 24, 6–11 (2016). https://doi.org/10.1007/s00167-014-3271-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3271-3