Abstract
Purpose
Excellent clinical and kinematical performance is commonly reported after medial pivot knee arthroplasty. However, there is conflicting evidence as to whether the posterior cruciate ligament should be retained. This study simulated how the posterior cruciate ligament, post-cam mechanism and medial tibial insert morphology may affect postoperative kinematics.
Methods
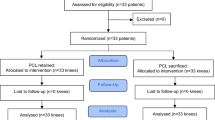
After the computational intact knee model was validated according to the motion of a normal knee, four TKA models were built based on a medial pivot prosthesis; PS type, modified PS type, CR type with PCL retained and CR type with PCL sacrificed. Anteroposterior translation and axial rotation of femoral condyles on the tibia during 0°–135° knee flexion were analyzed.
Results
There was no significant difference in kinematics between the intact knee model and reported data for a normal knee. In all TKA models, normal motion was almost fully restored, except for the CR type with PCL sacrificed. Sacrificing the PCL produced paradoxical anterior femoral translation and tibial external rotation during full flexion.
Conclusion
Either the posterior cruciate ligament or post-cam mechanism is necessary for medial pivot prostheses to regain normal kinematics after total knee arthroplasty. The morphology of medial tibial insert was also shown to produce a small but noticeable effect on knee kinematics.
Level of evidence
V.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The modern concept of total knee arthroplasty (TKA) was introduced in the early 1970s and has since then become a well-established procedure for the treatment of end-stage osteoarthritis. The ideal outcome of TKA is the retention of normal knee kinematics and functionality. However, it has been found that current prostheses, including posterior cruciate ligament retaining (CR) and posterior stabilizing (PS) prostheses, are typically unable to recover normal motion. Fluoroscopic analysis of CR knees has shown abnormal anterior translation and axial rotation between the tibia and femur during weight bearing activities [29]. The PS prosthesis can offer more predictable kinematics by using a post-cam system to substitute the posterior cruciate ligament (PCL), and it also forces more posterior femoral translation when compared with CR prostheses. But the kinematics also differ significantly from a normal knee, which may result from lack of engagement between the post and cam and excessive impingement between the tibial post and femoral notch [3]. These various kinematic abnormalities may reduce the maximum flexion angle achievable, affect the efficiency of the quadriceps, alter patella mechanics, provide inadequate stability, and not give the “feeling of a normal knee”, which inevitably impairs the prosthesis’ longevity [24, 25].
The concept of “medial-pivot” was proposed in 2002, and differs from the classic CR and PS prostheses in that it is characterized by a high conformity between the condyles and tibial insert. The medial and lateral condyles are spherical, and the insert has a socket with precise conformity on the medial side and an accurate trough on the lateral side [6]. It has been hypothesized that the constraining shape of the insert can substitute the function of the PCL and retain normal kinematics. This concept has been applied to several prostheses, including the ADVANCE Medial Pivot (Wright Medical, Arlington, TN), Medial Rotation Knee (Finsbury Orthopaedics, Surrey, UK), and Freeman-Samuelson Modular prosthesis (Zimmer-Centerpulse, Wintertur, Switzerland). Follow-up results in all aspects, clinical, radiological and kinematical, are promising [1, 14, 17, 22, 23, 26, 27]. During surgery, whether the PCL is preserved or resected depends on its functional level at the time of examination. No significant difference in clinical outcomes has been found between these two options [2, 6]. When compared with a PS prosthesis, such medial pivot designs offer a superior prognosis [13]. The postoperational kinematics have also been found to exhibit motion patterns similar to a normal knee [5, 23]. However, kinematic differences between PCL retaining and sacrificing knees have not yet been investigated.
The purpose of this study was to evaluate if PCL processing, the post-cam mechanism, and medial insert morphology may influence knee kinematics. Femoral anteroposterior translation and tibial axial rotation coupled with flexion were investigated in our simulation. It is hypothesized that suitable medial insert morphology can successfully substitute for the PCL and recover normal knee motion, and that both the PCL and post-cam mechanism are not necessary for medial pivot prostheses.
Materials and methods
Knee kinematics were analyzed using validated computer models of the knee joint. A healthy right knee of a female volunteer (age: 30 years old, weight: 50 kg, height: 160 cm) was used for scanning and reconstructing the intact knee model. This subject gave informed consent before scanning, and this study had been approved by Beijing Chao-Yang Hospital (approval number: 12-S-70). Images were acquired by sagittal magnetic resonance imaging (SIEMENS MAGNETOM Trio A Tim SYSTEM 3T, Siemens, Germany) and ImageJ (Slice interval: 1 mm, Resolution: 480 × 512 pixels). The proximal tibial bone and the distal femoral bone were transected approximately 75 mm from the natural joint line. The model was smoothed and substantiated using Geomagic Studio v9.0 (Parametric Technology Corp., Needham, MA, USA). Dynamic simulation was performed in MSC.ADAMS_R3 (MSC Software, Santa Ana, CA, USA). The meniscus and cruciate and collateral ligaments were reconstructed. Ligament forces were simulated by the following equation, with the parameters as in Table 1 [21]:
where ε is the strain in the ligament, K 1 and K 2 are the stiffness coefficients, L and L 0 are the ligament’s current and slack lengths. Both the medial and lateral menisci were separated into three segments, anterior, posterosuperior and posteroinferior portions for simulating the movements of menisci during knee flexion. The anterior meniscal portion was fixed on the tibial plateau, with the posterosuperior and posteroinferior portions being connected to the anterior portion by elastic tensile spring elements. The stiffness coefficients of medial and lateral menisci were simulated as 200 (N/mm) and 5 (N/mm), respectively. A damping coefficient of 0.5 (N s/mm) was applied to the lateral meniscus The only muscle considered in the current model was the quadriceps, with a 5° valgus to the mechanical axis of the femur. Both the quadriceps tendon and patellar tendon were also included, with stiffness coefficients of 2,000 and 1,142 N/mm respectively [20]. To simulate the wrapping of the quadriceps tendon around the trochlear groove during knee flexion, two rows of rigid beads were built along the medial and lateral bundles of the quadriceps tendon [18] (Fig. 1). The femoral flexion and extension axes were in compliance with the condylar radii of the medial and lateral femoral condyles. From full extension to 15° flexion, the femoral extension axis was designated as a connective line between the extension facet centers, and from 15° to 120° flexion, the femoral flexion axis was defined as a line connecting the flexion facet centers [15]. Only a flexion-extension motion was allowed for the tibial component and an average ground reaction force of 1.5 body weight (750 N) was applied to the center of mass of the tibial component [8]. The friction coefficients of cartilage-to-cartilage and metal-to-polyethylene surfaces were designated as frictionless and 0.04 respectively [11].
To calculate femoral anteroposterior translation (medial/lateral condyles) and tibial axial rotation, a Cartesian coordinate system was constructed in the models in ADAMS [16]. It was composed of a longitudinal axis (z, internal and external rotation axis), a mediolateral axis (y, flexion and extension axis), and an anteroposterior axis (x, varus and valgus rotation axis). Anteroposterior femoral translation was measured in the x direction on the coordinates of the medial and lateral condyle’s flexion facet centers relative to their original positions. Internal and external tibial rotation was measured in the z direction on the local coordinate of the tibia relative to the local coordinate of the femur. 0°–135° of knee flexion was simulated and the kinematics data was recorded every 10°.
If the performance of the intact model corresponded with the reported kinematics of a normal knee, it was imported into Pro/Engineer WildFire 5.0 (Parametric Technology Corp., Needham, MA, USA) for bone preparation. The clearance between the femoral condyle and tibial plateau, 3.4 mm in the present model, was occupied by femoral and tibial components equally. The bone was prepared according to standard surgical techniques. The distal femoral was cut at an angle perpendicular to the mechanical axis (the line between the center of the femoral head and the trochlear notch) of the femur with 0° of retroversion. The transepicondylar axis was used for rotational alignment. The amount of bone removed was the same as that replaced by the femoral component. The size of the femoral component was determined by anteroposterior dimensions of the distal femur; both ‘anterior referencing’ and ‘posterior referencing’ techniques were used to avoid notching of the anterior cortex and to reduce posterior condylar offset. The tibia was cut perpendicular to its mechanical axis (the line linking the center of the tibial plateau and the center of the talus) with 0° of posterior slope. The patella was not resurfaced.
The medial pivot knee prosthesis used in this study, D-knee, was designed by a senior surgeon (T. B. Qu). The D-knee is characterized by posterior stability with a medial pivot (Figs. 2, 3). To further understand the effect of different insert radii and PCL processing on kinematic performance, the D-knee was modified into four different models; PS-r25, PS-r40, CR-PCL and CR-no PCL. A post and cam was included in the PS models, and the medial side of the insert used 2 different medial–lateral radii, 25 mm (r25) and 40 mm (r40) (Fig. 4). The CR models used a similar articulating geometry to the PS-r25 designs except without a tibial post (Fig. 4). Both PCL retaining (CR-PCL) and PCL scarified (CR-no PCL) concepts were simulated in the CR models. Kinematic performances, including anteroposterior translations of medial/lateral femoral condyles and tibial internal rotations, were compared against two commercial products, United Posterior-Stabilized Knee System (United Orthopaedic Corp., Taiwan) and U2 Total Knee System-CR type (United Orthopaedic Corp., Taiwan) [20, 21].
Results
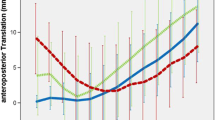
During model validation, the intact knee model showed similar kinematic behavior to the normal knee joint [16] (Fig. 5) by representing the maximum difference of condylar anteroposterior translations within 2 mm. The results of anterioposterior translation of the lateral condyle are shown in Fig. 6. In the PS models, the commercial knees displayed a totally different movement pattern to the normal knee. Although the medial pivot designs still had apparent differences with the intact knee, they did show similar movements and posterior translation. In addition, there were slight differences between the PS-r25 and PS-r40 models. For CR knees, the commercial product and CR-no PCL design demonstrated anterior translation after flexion beyond 70°, which does not correspond to normal knee movement. Of all models, the CR-PCL had the closest kinematic performance to a normal knee.
Figure 7 shows the movements of the medial condyle. Similar to the results of the lateral condyle, the commercial PS design had the greatest difference to a normal knee, and there was no obvious difference in performance between PS-r25 and PS-r40. The movement of the medial condyle in CR types was also similar to lateral condyle, with the CR-PCL having the closest resemblance to a normal knee.
For rotation (Fig. 8), all PS types showed similar movements before knee flexion to 70°. Again, the CR-PCL was most similar to the intact knee and the PS knees showed obvious deviations from this. However, the CR-no PCL had the greatest difference to the normal knee in terms of rotation.
Discussion
The most important finding of the present study was demonstrating how retention of the PCL affects knee kinematics after TKA. For validating our model, we compared the anterioposterior translation of the medial and lateral condyles to a knee model presented by Johal et al. [16]. Johal et al. investigated tibio-femoral movement in a living knee using interventional MRI. Anteroposterior translations of medial and lateral femoral condyles were measured every 10° from hyperextension (−5°) to 120°. Similar motion patterns have been reproduced in our study’s intact knee model. The maximum error in anterioposterior translation was within 3 mm while the translation of the lateral condyle showed nearly identical movements to the previous study. Both of the PS models and the CR-PCL model showed more similar kinematic performance to the intact knee than the other two commercial products. The articulating surface of the D-Knee tibial insert has a medial pivot and thus can be expected to mimic the kinematic behavior of an intact knee joint. The results demonstrated that the concept of using a medial pivot can effectively increase tibial internal rotation during knee flexion, except for in the CR-no PCL model (Fig. 8). Several studies have also revealed improved knee joint kinematics when using medial pivot designs in clinical practice [4, 5, 23], which may be a key factor to improving the feasibility of high flexion performance.
The CR-PCL performed most similar to the intact knee in this current study. Cates et al. [7] also compared the performance of CR and PS knees at high flexion angles and reported less posterior translation of femoral components in CR designs, but had greater tibial internal rotation. A similar phenomenon was also found in kneeling in a related study [12]. On the contrary, some studies have reported poor kinematic performance in CR knees [9], or claimed no significant differences with PS knees [28]. Possible reasons for such contradictory conclusions may be due to differences in experimental activities (active or passive motion, squatting/kneeling/lunging, etc.) or the design of knee prosthesis for specific demands (e.g. high flexion).
The performance of the PS-r25 and PS-r40 models were quite similar in both femoral anteroposterior translation and tibial internal rotation. The major difference between the two PS knee designs was that greater tibial internal rotation was found in the PS-r40 model at full flexion. The medial pivot concept is achieved by better geometrical conformity in the medial articulating contact pair, and better constraint on the medial side shall possibly enhance the tibial rotation during knee flexion [10]. However, the greater posterior translation of the medial condyle in the PS-r25 model indicated a disparity between medial and lateral condyles which may reduce tibial rotation. The PS-r40 model has a slightly more lax constraint on the medial contact pair in the mediolateral direction, but greater tibial internal rotation was achieved around the terminal range of knee flexion simulated in current study. It may imply that, even when using a medial pivot design, adequate constraint should be maintained rather than perfect conformity of the medial contact pair. The slightly released constraint on the medial contact pair would also influence the post-cam mechanism, since the mediolateral constraint had been altered in the PS-r40 model. However, it should also be noted that the magnitude of tibial internal rotation around the terminal knee flexion range in this current study exceeded that of the intact model. Further investigation is required to find out the optimal geometry of the medial contact pair of the medial pivot knee prosthesis.
The CR-no PCL model, without PCL and post-cam mechanism, was created to investigate if medial pivot constraints can adequately guide knee motion. However, the results revealed that insufficient posterior translations of both femoral condyles and tibial internal rotation. The dish-like geometry of the medial tibial insert can practically prevent the paradoxical posterior movement, but may also be an obstacle to knee flexion due to the lack of femoral rollback. In addition, loss of the guiding function of the PCL or post-cam would lead to the decrease in tibial internal rotation observed during knee flexion.
Unfortunately, the results of this study have rejected our original hypothesis that suitable medial insert morphology can successfully substitute the function of the PCL and recover normal knee motion after TKA, and that both the PCL and post-cam mechanism are not necessary for medial pivot prostheses. The CR-no PCL model demonstrated that only medial pivot morphology cannot completely substitute the function of PCL or the post-cam mechanism in PS knee designs. Considering the results of the CR-PCL model, retaining the PCL is important for restoring knee kinematics in CR knee designs.
Some limitations of this study should be noted.
-
(1)
The D-knee prosthesis utilized in the current study was a new product designed by our team. More detailed design parameters should be further verified in clinical practice.
-
(2)
Not all of the functions of surrounding soft tissues including the joint capsule, hamstrings, and gastrocnemius can be perfectly reconstructed in current study. For example, the joint capsule plays an important role in passive flexion, whereby it normally acts to push the tibia anteriorly, resulting in continual femoral rollback at high flexion angles.
-
(3)
Individual anatomic variations were not considered in the simulations. Nevertheless, the current dynamic models do have the capacity to distinguish the effects of any modifications to implant design and PCL. More studies regarding kinematics after medial pivot knee arthroplasty with the PCL sacrificed or retained are essential.
-
(4)
According to previous studies, TKA alignment, such as the tibial slope, will affect the kinematics after TKA [19]. For better kinematic performance of the D-Knee, these alignment variables should be considered in further study.
Conclusion
For regaining normal knee motion, including femoral anteroposterior translation and tibial axial rotation, this current study demonstrated that a CR knee solely constrained by a medial pivot is not stable enough to substitute the PCL. Either retention of the PCL or a post-cam mechanism is necessary when using this kind of prosthesis. Such designs that incorporate a medial pivot and post-cam mechanism may offer a superior kinematic performance. Current study may provide referable information for surgeons to adequately identify when a medial pivot knee prosthesis is considered in TKA.
References
Amin A, Al-Taiar A, Sanghrajka AP, Kang N, Scott G (2008) The early radiological follow-up of a medial rotational design of total knee arthroplasty. Knee 15(3):222–226
Bae DK, Song SJ, Cho SD (2011) Clinical outcome of total knee arthroplasty with medial pivot prosthesis a comparative study between the cruciate retaining and sacrificing. J Arthroplast 26(5):693–698
Banks SA, Harman MK, Hodge WA (2002) Mechanism of anterior impingement damage in total knee arthroplasty. J Bone Joint Surg Am 84(Suppl 2):237–242
Barnes CL, Blaha JD, DeBoer D, Stemniski P, Obert R, Carroll M (2012) Assessment of a medial pivot total knee arthroplasty design in a cadaveric knee extension test model. J Arthroplast 27(8):1460–1468
Barnes CL, Sharma A, Blaha JD, Nambu SN, Carroll ME (2011) Kneeling is safe for patients implanted with medial-pivot total knee arthroplasty designs. J Arthroplast 26(4):549–554
Blaha JD (2002) A medial pivot geometry. Orthopedics 25(9):963–964
Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M (2008) In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplast 23(7):1057–1067
D’Lima DD, Patil S, Steklov N, Chien S, Colwell CW Jr (2007) In vivo knee moments and shear after total knee arthroplasty. J Biomech 40(Suppl 1):S11–S17
Fantozzi S, Catani F, Ensini A, Leardini A, Giannini S (2006) Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res 24(12):2222–2229
Fitz W, Sodha S, Reichmann W, Minas T (2012) Does a modified gap-balancing technique result in medial-pivot knee kinematics in cruciate-retaining total knee arthroplasty?: a pilot study. Clin Orthop Relat Res 470(1):91–98
Godest AC, Beaugonin M, Haug E, Taylor M, Gregson PJ (2002) Simulation of a knee joint replacement during a gait cycle using explicit finite element analysis. J Biomech 35(2):267–275
Hamai S, Miura H, Higaki H, Matsuda S, Shimoto T, Sasaki K, Yoshizumi M, Okazaki K, Tsukamoto N, Iwamoto Y (2008) Kinematic analysis of kneeling in cruciate-retaining and posterior-stabilized total knee arthroplasties. J Orthop Res 26(4):435–442
Hossain F, Patel S, Rhee SJ, Haddad FS (2011) Knee arthroplasty with a medially conforming ball-and-socket tibiofemoral articulation provides better function. Clin Orthop Relat Res 469(1):55–63
Iida T, Minoda Y, Kadoya Y, Matsui Y, Kobayashi A, Iwaki H, Ikebuchi M, Yoshida T, Nakamura H (2012) Mid-term clinical results of alumina medial pivot total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(8):1514–1519
Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82(8):1189–1195
Johal P, Williams A, Wragg P, Hunt D, Gedroyc W (2005) Tibio-femoral movement in the living knee. A study of weight bearing and non-weight bearing knee kinematics using ‘interventional’ MRI. J Biomech 38(2):269–276
Karachalios T, Roidis N, Giotikas D, Bargiotas K, Varitimidis S, Malizos KN (2009) A mid-term clinical outcome study of the advance medial pivot knee arthroplasty. Knee 16(6):484–488
Kessler O, Patil S, Colwell CW Jr, D’Lima DD (2008) The effect of femoral component malrotation on patellar biomechanics. J Biomech 41(16):3332–3339
Kim JH (2013) Effect of posterior femoral condylar offset and posterior tibial slope on maximal flexion angle of the knee in posterior cruciate ligament sacrificing total knee arthroplasty. Knee Surg Relat Res 25(2):54–59
Lin KJ, Huang CH, Liu YL, Chen WC, Chang TW, Yang CT, Lai YS, Cheng CK (2011) Influence of post-cam design of posterior stabilized knee prosthesis on tibiofemoral motion during high knee flexion. Clin Biomech (Bristol, Avon) 26(8):847–852
Liu YL, Lin KJ, Huang CH, Chen WC, Chen CH, Chang TW, Lai YS, Cheng CK (2011) Anatomic-like polyethylene insert could improve knee kinematics after total knee arthroplasty-a computational assessment. Clin Biomech (Bristol, Avon) 26(6):612–619
Mannan K, Scott G (2009) The Medial Rotation total knee replacement a clinical and radiological review at a mean follow-up of six years. J Bone Joint Surg Br 91(6):750–756
Moonot P, Mu S, Railton GT, Field RE, Banks SA (2009) Tibiofemoral kinematic analysis of knee flexion for a medial pivot knee. Knee Surg Sports Traumatol Arthrosc 17(8):927–934
Moonot P, Shang M, Railton GT, Field RE, Banks SA (2010) In vivo weight-bearing kinematics with medial rotation knee arthroplasty. Knee 17(1):33–37
Pritchett JW (2004) Patient preferences in knee prostheses. J Bone Joint Surg Br 86(7):979–982
Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ (2003) Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res 410:139–147
Vecchini E, Christodoulidis A, Magnan B, Ricci M, Regis D, Bartolozzi P (2012) Clinical and radiologic outcomes of total knee arthroplasty using the Advance Medial Pivot prosthesis. A mean 7 years follow-up. Knee 19(6):851–855
Victor J, Banks S, Bellemans J (2005) Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br 87(5):646–655
Yoshiya S, Matsui N, Komistek RD, Dennis DA, Mahfouz M, Kurosaka M (2005) In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty 20(6):777–783
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Fang, CH., Chang, CM., Lai, YS. et al. Is the posterior cruciate ligament necessary for medial pivot knee prostheses with regard to postoperative kinematics?. Knee Surg Sports Traumatol Arthrosc 23, 3375–3382 (2015). https://doi.org/10.1007/s00167-014-3249-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3249-1