Abstract
Purpose
Counteracting posterior translation of the tibia with an anterior force on the posterior proximal tibia has been demonstrated clinically to improve posterior knee laxity following posterior cruciate ligament (PCL) injury. This study quantified forces applied to the posterior proximal tibia by two knee braces designed for treatment of PCL injuries.
Methods
The forces applied by two knee braces to the posterior proximal tibia and in vivo three-dimensional knee kinematics of six adult, male, healthy volunteer subjects (mean ± standard deviation: height, 182.5 ± 5.2 cm; body mass, 83.2 ± 9.3 kg; body mass index, 24.9 ± 1.5 kg/m2; age, 25.8 ± 2.9 years) were measured using a custom pressure mapping technique and traditional surface marker motion capture techniques, while subjects performed three functional activities. The activities included seated unloaded knee flexion, squatting, and stair descent in a new generation dynamic force (DF) PCL brace and a static force (SF) PCL brace.
Results
During unloaded flexion at the lowest force level setting, the force applied by the DF brace increased as a function of flexion angle (slope = 0.7 N/°; p < 0.001) compared to the SF brace effect. Force applied by the SF brace did not significantly change as a function of flexion angle (slope = 0.0 N/°; n.s.). By 45° of flexion, the average force applied by the DF brace (48.1 N) was significantly larger (p < 0.001) than the average force applied by the SF brace (25.0 N). The difference in force continued to increase as flexion angle increased. During stair descent, average force (mean ± standard deviation) at toe off was significantly higher (p = 0.013) for the DF brace (78.7 ± 21.6 N) than the SF brace (37.3 ± 7.2 N). Similar trends were observed for squatting and for the higher force level settings.
Conclusions
The DF brace applied forces to the posterior proximal tibia that dynamically increased with increased flexion angle. Additionally, the DF brace applied significantly larger forces at higher flexion angles compared to the SF brace where the PCL is known to experience larger in situ forces. Clinical studies are necessary to determine whether the loading characteristics of the DF brace, which more closely replicated the in situ loading profile of the native PCL, results in long-term improved posterior knee laxity following PCL injury.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tears of the posterior cruciate ligament (PCL) can be functionally disabling, especially during descent and deceleration activities, due to increased posterior laxity of the knee. Although favourable clinical outcomes have been reported for non-operative treatment of most isolated grade I–II PCL injuries [9, 23], increased rates of osteoarthritis have been associated with non-operative treatment of chronic grade III injuries [3, 4, 16] and surgical intervention has been recommended for most combined ligament injuries [20]. Although an improved understanding of PCL anatomy and function has led to more anatomic reconstructions [2, 18, 27], posterior tibial translation (PTT) has reportedly not been restored to normal levels following both non-operative and operative treatment of PCL injuries [15, 24, 26, 28] due to healing of the ligament or graft in an elongated position. Increased PTT during functional activities and while in the supine position, due to gravity (posterior sag), reportedly contributed to the described elongation [26].
Counteracting the increased PTT observed in PCL-disrupted knees with an anterior directed force on the proximal tibia has been validated clinically to improve posterior knee laxity [1, 15, 28]. Despite the high rates of PCL injuries observed in trauma centres [7, 8], few braces have been developed specifically for the treatment of PCL injuries. A PCL brace that applies a static anterior directed force to the posterior proximal tibia is the only commercially available brace that has been evaluated clinically for use in conjunction with operative and non-operative treatment of PCL injuries (PCL-Jack brace, Albrecht, Stephanskirchen, Germany) [13, 25]. Although the brace reportedly contributed to satisfactory clinical outcomes, posterior sag of the tibia was not restored to intact levels following non-operative treatment [13]. A new generation functional brace (Rebound PCL, Össur Inc., Foothill Ranch, CA, USA) for PCL injuries, which applies a dynamic anterior directed force to the posterior proximal tibia, has recently been introduced to the market but has not been biomechanically or clinically validated.
A recent article on PCL bracing [14] suggested that PCL braces should apply forces to the knee joint which replicate the anatomic forces applied by the native PCL to best support the PCL-disrupted knee. The in situ force behaviour of the PCL has been demonstrated in vitro and in vivo to be dependent on the flexion angle of the knee, with maximal force and elongation occurring between 90° and 120° of flexion and decreasing as the knee is extended [5, 6, 10, 11, 18, 19, 22, 27]. To date, bracing of PCL injuries has only been evaluated clinically, and the mechanical constraint applied by PCL braces to the knee joint has not been quantified.
Therefore, the purpose of this study was to quantify the external forces applied to the posterior proximal tibia by both the static force (SF) PCL brace and a dynamic force (DF) brace. Forces applied by the DF brace were hypothesized to dynamically change as a function of flexion angle, while forces applied by the SF brace would remain constant. Additionally, forces applied by the DF brace were hypothesized to be significantly larger than forces applied by the SF brace by 45° of flexion and this difference would continue to increase as flexion angle increased.
Materials and methods
This study was approved by the Institutional Review Board at the Vail Valley Medical Center, and all participants signed an informed consent. The anterior forces applied by two knee braces to the posterior proximal tibia and in vivo three-dimensional (3D) kinematic data of the braced limb were collected with a custom pressure mapping technique and traditional surface marker motion capture techniques on six adult, male, active, healthy volunteer subjects [mean ± standard deviation: height, 182.5 ± 5.2 cm; body mass, 83.2 ± 9.3 kg; body mass index (BMI), 24.9 ± 1.5 kg/m2; age, 25.8 ± 2.9 years], while performing three activities common to PCL post-operative rehabilitation programmes (Fig. 1). The subjects had no prior history of knee injury or surgery to the lower limbs.
Test protocol
Subjects performed unloaded knee flexion, squatting, and stair descent. To perform unloaded flexion, the subject was in a seated position and flexed the braced knee from full extension to 90° over 2 s. To perform the squat, the subject stood in full extension and squatted to 90° of flexion over 2 s. The stair descent activity required subjects to descend three stairs at 75 steps per minute, and the data from the third stair were analysed. The first step was taken with the braced leg. The rate of steps during stair descent was determined during pilot testing and was slightly slower than what has been reported for flat level walking (90 steps per minute) [21].
Functional braces
Two braces were evaluated on each subject: a SF PCL brace (PCL-Jack brace, Albrecht GmbH, Stephanskirchen, Germany) and a DF PCL brace (Rebound PCL brace, Össur Inc., Foothill Ranch, CA, USA). The SF brace has 15 manually adjustable levels of static force which the brace applies to the posterior proximal tibia through a spring-loaded hinge. The level of force can be manually adjusted with a manufacturer provided hex driver. The DF brace reportedly applies a dynamic force to the posterior proximal tibia that increases with increased flexion through a tensioned cable and pulley system. The initial level of force of the DF brace at full extension can manually be adjusted through tensioning of the cable with three manufacturer provided torque knobs. Notably, the SF brace is designed with a stop at 0° and 90° of knee flexion, whereas the DF brace comes with a stop at 0° and 105°. Although the stops can be removed for both braces, they were left intact for this study to emulate standard clinical care. Proper brace sizing and fit were performed according to the manufacturers’ recommendations. All braces were worn on the left leg. The DF brace was tested at each of the three force levels that correspond to the provided torque knobs. The SF brace was tested at force levels 5, 10, and 15.
Motion analysis
Prior to testing, five retro-reflective spherical markers (10 mm diameter) were securely attached to the subject to create a three-marker-per-segment configuration for the collection of lower extremity kinematic data. One marker was placed adjacent to the subject’s lateral malleolus, one marker was placed adjacent to the subject’s greater trochanter, and three markers were placed on the lateral frame of the brace. A static trial was first obtained with the subject in full extension to document the initial flexion angle of the markers at the extended position. Subjects practiced the activities until they were comfortable and could reproducibly perform the activities. Subsequently, one trial of each activity was collected. Three-dimensional marker position data were recorded using standard motion capture techniques using ten high-speed cameras (Motion Analysis Corp, Santa Rosa, CA, USA), sampled at 100 Hz. Three-dimensional coordinates of the three markers were used to calculate flexion angles during the activities.
Pressure mapping
A calibrated pressure sensor (area: 27.9 mm × 33.0 mm, thickness: 0.1 mm, Model 4000, Tekscan Inc., Boston, MA, USA) was used to quantify forces applied to the posterior proximal tibia by each brace. The sensor was secured between the posterior aspect of the brace and the posterior compartment of the tibia with a custom fixture. The custom fixture ensured all anterior directed forces were captured by the sensor. Accuracy of the calibrated pressure sensor with custom fixture was verified with an Electropuls E1000 test frame (Instron, Norwood, MA, USA) to be within ±5 % of the indicated force for the force range observed in this study. Pressure data were recorded simultaneously with the motion capture data at 100 Hz using the corresponding software (I-Scan, Tekscan Inc.), and the total force on the sensor was recorded.
Data reduction
Simultaneous force and motion capture data were used to determine the anterior directed force that each brace applied to the proximal posterior tibia in relation to flexion angle. The data were analysed from 0° (or full extension) to 90° of knee flexion in 15° intervals using a custom algorithm (MATLAB, The Mathworks, Natick, MA, USA).
Statistical analyses
An a priori power analysis was conducted and determined that six subjects were needed to detect a significant difference in anterior directed force at 30° of flexion with 80 % power between the SF brace and the DF brace. Data were analysed with linear mixed-effect models for each force level and each measurement with brace as a fixed repeated factor and flexion angle as a random repeated covariate. For all models, the SF brace was used as a baseline for parameter estimation and the additional contribution of the DF brace was determined.
Results
The median (minimum, maximum) forces applied to the posterior proximal tibia by the SF and DF braces for seated flexion, squat, and stair descent at the three force settings are reported in Table 1.
Unloaded flexion
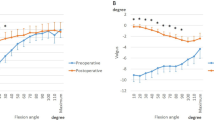
During unloaded flexion at the lowest force level, the anterior directed force applied to the posterior proximal aspect of the tibia by the SF brace did not significantly change as a function of flexion angle (slope = 0.0 N/°; n.s.) (Fig. 2). Conversely, the anterior directed force applied to the posterior proximal aspect of the tibia by the DF brace did increase as a function of flexion angle (slope = 0.7 N/°; p < 0.001) compared to the SF brace effect. The Y-intercept, corresponding to the force at full extension, was not significantly different (n.s.) for the SF brace (23.6 N) and DF brace (18.6 N). However, by 45° of flexion, the average force applied by the DF brace (48.1 N) had become significantly larger (p < 0.001) than the average force applied by the SF brace (25.0 N). Results for the other force level settings are similarly reported in Table 2. A trend of increasing force corresponding to higher force level settings was observed for both braces.
Squat
During squatting at the lowest force level, the anterior directed force applied to the posterior proximal aspect of the tibia by the SF brace did not significantly change as a function of flexion angle (slope = 0.0 N/°; n.s.) (Fig. 2). Conversely, the anterior directed force applied to the posterior proximal aspect of the tibia by the DF brace did increase as a function of flexion angle (slope = 0.9 N/°; p < 0.001) compared to the SF brace effect. The Y-intercept, corresponding to the force at full extension, was not significantly different (n.s.) for the SF brace (32.7 N) and DF brace (23.5 N). However, by 45° of flexion, the average force applied by the DF brace (64.7 N) had become significantly larger (p < 0.001) than the average force applied by the SF brace (34.5 N). Results for the other force level settings are similarly reported in Table 2. A trend of increasing force corresponding to higher force level settings was observed for both braces.
Stair descent
For the lowest force setting, the force (mean ± standard deviation) at toe off, which corresponded to the peak flexion angle achieved during stair descent, was significantly higher (p = 0.013) for the DF brace (78.7 ± 21.6 N) than the SF brace (37.3 ± 7.2 N). The force at toe off applied by the SF brace (43.2 ± 12.0 N) was not significantly different (n.s.) from the DF brace (33.3 ± 8.2 N). The force applied by the DF brace significantly increased (p = 0.014) from toe strike to toe off. The force applied by the SF brace did not significantly change (n.s.). Results for the other force level settings are similarly reported in Table 3. A trend of increasing force corresponding to higher force level settings was observed for both braces.
Discussion
The most important finding of this study was the dynamically changing anteriorly directed force applied by the DF brace to the posterior proximal tibia as a function of flexion angle and the constant force applied by the SF brace. Additionally, forces applied by the DF brace were significantly larger than forces applied by the SF brace at higher flexion angles where the PCL is maximally loaded in vivo. The results of this study confirmed our hypothesis that forces applied by the DF brace would dynamically change as a function of flexion angle and forces applied by the SF brace would remain constant. Additionally, forces applied by the DF brace were confirmed to be significantly larger than forces applied by the SF brace by 45° of flexion and this difference continued to increase as flexion angle increased. The use of a static anterior directed load to the posterior tibia has been demonstrated to improve posterior knee laxity following PCL reconstruction [1, 15, 25]. The authors theorize that more physiologic loading, rather than a pure static force, of a knee brace on a PCL reconstructed knee will further improve post-operative posterior knee laxity. Clinical studies are needed to determine whether the dynamic loading characteristics of the DF brace observed in the present study will result in improved patient outcomes following PCL reconstruction.
The force-flexion behaviour observed in the present study for the DF brace is similar to reports of the in situ force-flexion behaviour of the native PCL and reconstructed PCL [5, 6, 10, 11, 17, 22] (Fig. 3). Additionally, Iwata et al. [12] demonstrated that maximum posterior knee instability in isolated PCL deficient knees during stair descent occurred immediately after toe off with the knee in deep flexion. This further highlights the need for increased support at deeper knee flexion angles during functional activities. Although the forces applied by the DF brace were less than reported tension in the PCL, the authors theorize that the increased forces applied by the DF brace during deep knee flexion may provide additional protection to the healing ligament or graft at these higher risk flexion angles. Additionally, the overall higher forces observed for the DF brace relative to the SF will provide additional resistance to posterior sag throughout full range of motion. The DF brace provides additional posterior support to the joint at flexion angles which place increased load on the PCL and demonstrates an important shift from static to dynamic and physiologic support of knee ligament injuries.
Comparison of single bundle (SB) PCL graft forces [17] in response to a 134-N posterior tibial load with forces generated by the DF brace and SF brace at the highest force setting during squatting
Despite the discrepancies between the static forces applied by the SF brace and dynamic in situ force behaviour of the native PCL, improved posterior knee laxity has been observed clinically with the application of a static anterior directed force to the posterior proximal tibia [1, 15] and with the use of the SF brace [13, 25]. However, Jacobi et al. [13] reported that posterior laxity was not restored to the intact state. The improved clinical outcomes reported for the SF brace despite the biomechanical limitations encourage the use of braces with an anterior force mechanism for the treatment of PCL injuries. Further clinical studies are needed to determine whether the improved biomechanical characteristics of the DF brace leads to posterior stability more similar to the native state and improved clinical outcomes.
It is acknowledged that there were limitations to the present study. Only asymptomatic, male subjects were tested. However, it was not necessary to have a PCL deficient population to characterize the force-flexion behaviour of the braces. Asymptomatic knees provided a control in which to compare the force patterns of the two braces. Additionally, the braces may behave differently on female subjects due to inter-gender anatomic and body composition variability. However, the authors theorize that although the magnitude of force may change, the observed static versus dynamic nature of the braces would be preserved due to the inherent mechanical designs of the braces. Additionally, subjects were an active, healthy, and low BMI population and these results may not be transferable to populations with different body compositions. Subjects performed the activities in a controlled laboratory setting, which is not representative of a high-intensity competitive setting. Additionally, patient compliance with brace prescription is a well-recognized challenge associated with current bracing technologies, and patient compliance associated with the braces tested in the present study is unknown. Therefore, no conclusions can be drawn on how the loading characteristics of these braces will influence long-term patient outcomes. However, this well-controlled and reproducible study design allowed for the braces to be evaluated in direct comparison and the activities were relevant to PCL injury and rehabilitation.
Conclusions
The DF brace applied dynamically increasing forces to the posterior proximal tibia as flexion angle increased and applied significantly larger forces at higher flexion angles where the PCL is known to experience larger in situ forces. Clinical studies are necessary to determine whether the loading characteristics of the DF brace, which more closely replicated the in situ loading profile of the native PCL, results in long-term improved posterior knee laxity following PCL injury.
References
Ahn JH, Lee SH, Choi SH, Wang JH, Jang SW (2011) Evaluation of clinical and magnetic resonance imaging results after treatment with casting and bracing for the acutely injured posterior cruciate ligament. Arthroscopy 27:1679–1687
Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF (2012) Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Jt Surg Am 94:1936–1945
Clancy WG Jr, Shelbourne KD, Zoellner GB, Keene JS, Reider B, Rosenberg TD (1983) Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament: report of a new procedure. J Bone Jt Surg Am 65:310–322
Covey CD, Sapega AA (1993) Injuries of the posterior cruciate ligament. J Bone Jt Surg Am 75:1376–1386
DeFrate LE, Gill TJ, Li G (2004) In vivo function of the posterior cruciate ligament during weightbearing knee flexion. Am J Sports Med 32:1923–1928
Escamilla RF, Zheng N, MacLeod TD, Imamura R, Edwards WB, Hreljac A, Fleisig GS, Wilk KE, Moorman CT, Paulos L, Andrews JR (2010) Cruciate ligament tensile forces during the forward and side lunge. Clin Biomech (Bristol, Avon) 25:213–221
Fanelli GC (1993) Posterior cruciate ligament injuries in trauma patients. Arthroscopy 9:291–294
Fanelli GC, Edson CJ (1995) Posterior cruciate ligament injuries in trauma patients: part II. Arthroscopy 11:526–529
Fowler PJ, Messieh SS (1987) Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med 15:553–557
Fox RJ, Harner CD, Sakane M, Carlin GJ, Woo SL (1998) Determination of the in situ forces in the human posterior cruciate ligament using robotic technology: a cadaveric study. Am J Sports Med 26:395–401
Harner CD, Janaushek MA, Kanamori A, Yagi M, Vogrin TM, Woo SL (2000) Biomechanical analysis of a double-bundle posterior cruciate ligament reconstruction. Am J Sports Med 28:144–151
Iwata S, Suda Y, Nagura T, Matsumoto H, Otani T, Toyama Y (2007) Dynamic instability during stair descent in isolated PCL-deficient knees: what affects abnormal posterior translation of the tibia in PCL-deficient knees? Knee Surg Sports Traumatol Arthrosc 15:705–711
Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP (2010) Acute isolated injury of the posterior cruciate ligament treated by dynamic anterior drawer brace: a preliminary report. J Bone Jt Surg Br 92:1381–1384
Jansson KS, Costello KE, O’Brien L, Wijdicks CA, Laprade RF (2013) A historical perspective of PCL bracing. Knee Surg Sports Traumatol Arthrosc 21:1064–1070
Jung YB, Tae SK, Lee YS, Jung HJ, Nam CH, Park SJ (2007) Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc 16:729–733
Keller PM, Shelbourne KD, McCarroll JR, Rettig AC (1993) Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med 21:132–136
Kennedy NI, Laprade RF, Goldsmith MT, Faucett SC, Rasmussen MT, Coatney GA, Engebretsen L, Wijdicks CA (2014) Posterior cruciate ligament graft fixation angles, part 1: biomechanical evaluation of anatomic single-bundle reconstruction. Am J Sports Med. doi:10.1177/0363546514541225
Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Aroen A, Engebretsen L, LaPrade RF (2013) Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med 41:2828–2838
Li G, DeFrate LE, Sun H, Gill TJ (2004) In vivo elongation of the anterior cruciate ligament and posterior cruciate ligament during knee flexion. Am J Sports Med 32:1415–1420
Lopez-Vidriero E, David SA, Johnson DH (2010) Initial evaluation of posterior cruciate ligament injuries: history, physical examination, imaging studies, surgical and nonsurgical indications. Sports Med Arthrosc 18:230–237
Myers CA, Torry MR, Shelburne KB, Giphart JE, LaPrade RF, Woo SL, Steadman JR (2012) In vivo tibiofemoral kinematics during 4 functional tasks of increasing demand using biplane fluoroscopy. Am J Sports Med 40:170–178
Papannagari R, DeFrate LE, Nha KW, Moses JM, Moussa M, Gill TJ, Li G (2007) Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med 35:1507–1512
Parolie JM, Bergfeld JA (1986) Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med 14:35–38
Shelbourne KD, Davis TJ, Patel DV (1999) The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med 27:276–283
Spiridonov SI, Slinkard NJ, LaPrade RF (2011) Isolated and combined grade-III posterior cruciate ligament tears treated with double-bundle reconstruction with use of endoscopically placed femoral tunnels and grafts: operative technique and clinical outcomes. J Bone Jt Surg Am 93:1773–1780
Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ (2002) Fixed posterior subluxation in posterior cruciate ligament-deficient knees: diagnosis and treatment of a new clinical sign. Am J Sports Med 30:32–38
Wijdicks CA, Kennedy NI, Goldsmith MT, Devitt BM, Michalski MP, Aroen A, Engebretsen L, LaPrade RF (2013) Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med 41:2839–2848
Yoon KH, Park SW, Lee SH, Kim MH, Park SY, Oh H (2013) Does cast immobilization contribute to posterior stability after posterior cruciate ligament reconstruction? Arthroscopy 29:500–506
Acknowledgments
The authors acknowledge Kyle Jansson for his contributions to technology development and planning and design of this study. The authors acknowledge Grant Dornan, MSc for his contributions to the statistical analysis in this study and Angelica Wedell for the photography presented in this study.
Conflict of interest
Össur provided unrestricted in-kind donations of the braces utilized in this study. Dr. LaPrade is a consultant for Arthrex and Smith & Nephew.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
LaPrade, R.F., Smith, S.D., Wilson, K.J. et al. Quantification of functional brace forces for posterior cruciate ligament injuries on the knee joint: an in vivo investigation. Knee Surg Sports Traumatol Arthrosc 23, 3070–3076 (2015). https://doi.org/10.1007/s00167-014-3238-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3238-4