Abstract
Purpose
To prospectively investigate whether preoperative functional flexion axis in patients with osteoarthritis- and varus-alignment changes after total knee arthroplasty and whether a correlation exists both between preoperative functional flexion axis and native limb deformity.
Methods
A navigated total knee arthroplasty was performed in 108 patients using a specific software to acquire passive joint kinematics before and after implant positioning. The knee was cycled through three passive range of motions, from 0° to 120°. Functional flexion axis was computed using the mean helical axis algorithm. The angle between the functional flexion axis and the surgical transepicondylar axis was determined on frontal (α F) and axial (α A) plane. The pre- and postoperative hip-knee-ankle angle, related to femur mechanical axis, was determined.
Results
Postoperative functional flexion axis was different from preoperative only on frontal plane, while no differences were found on axial plane. No correlation was found between preoperative α A and native limb deformity, while a poor correlation was found in frontal plane, between α F and preoperative hip-knee-ankle angle.
Conclusions
Total knee arthroplasty affects functional flexion axis only on frontal plane while has no effect on axial plane. Preoperative functional flexion axis is in a more varus position respect to the transepicondylar axis both in pre- and postoperative conditions. Moreover, the position of the functional axis on frontal plane in preoperative conditions is dependent on native limb alignment, while on axial plane is not dependent on the amount of preoperative varus deformity.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Progress in imaging and computer technology has enabled great advances in analysis of the knee’s geometry and knee’s kinematics. In fact, they have made possible the building of 3-dimensional (3D) models of knee motion and computer representations of the joint surfaces [15, 21, 24, 38]. All these studies were performed with the aim of improving prosthesis design rather than for kinematic analysis of reconstructed knees.
Only in recent years, navigation has been used for intraoperative acquisition of the patient’s-specific kinematics and the development of a method to determine the individual axis of the knee.
One of the main methods used to estimate the axis of rotation of the knee joint, based on a kinematic technique, is called the “functional flexion axis” (FFA) method [23, 48, 49]. The FFA computation is based on the estimation of the mean helical axis (MHA), which aims to describe the motion of a rigid body as a rotation around and a translation along an instantaneous axis of rotation [49].
The FFA is a kinematically acquired reference related to the specific kinematics of the patient, as opposed to the conventional total knee arthroplasty (TKA) technique, which relies on anatomical landmarks. It can be determined reliably and reproducibly intraoperatively [12, 28, 31]. The FFA and the surgical transepicondylar axis (sTEA) are reported to be coincident by some Authors [3, 28], whereas others found these two axes to be non-coincident and non-parallel [13, 31]. Furthermore, the FFA is kinematically derived, surgeon independent and patient specific. Theoretically, it could be surgically used as an alternative reference for femoral component positioning in TKA. Unfortunately, at the present on the basis of available data, the accurate femoral component positioning relative to the FFA cannot be recommended [12, 28, 31].
No data were reported in the literature regard the influence of the preoperative limb alignment on the FFA estimation. This is the first study performed in vivo on such a large group of patients that deals with the importance of the native limb deformity on the FFA usefulness for the daily clinical practice in navigated TKA. Therefore, starting from the hypothesis that the orientation of the FFA does not depend on the degree of limb alignment, the main purpose of the present study was to investigate, in patients with end-stage osteoarthritis (OA) and varus alignment, the correlation between the amount of preoperative varus deformity and the FFA position, both in pre- and in postoperative conditions.
Material and methods
A unilateral, cruciate-retaining (CR), mobile-bearing (MB) TKA (Gemini-Light, Waldemar Link, Hamburg, Germany) was performed in a series of 108 consecutive patients with primary knee OA and a Kellgren/Lawrence (K/L) [20] score of at least four points in the Authors’ institution between 2008 and 2010. Demographics and preoperative radiographic evaluation of limb alignment are resumed in Table 1.
Preoperatively, all patients had weight-bearing antero-posterior (AP) and latero-lateral (LL) long-film radiographs [21]. The hip-knee-ankle angle (HKA), computed with respect to femur mechanical axis, was assumed to be a valgus knee greater than 180°, and less than 180° for a varus knee [9]. Twelve patients with valgus alignment were excluded from the study to avoid data dispersion due to the non-normal distribution of limb alignment in patients with OA and because of possible kinematics abnormalities in patients with valgus knees [10, 45, 51].
The TKA was performed with a standard, non-navigated surgical technique, aiming to restore a neutral mechanical alignment, and the average post- to preoperative correction on both frontal and axial plane is resumed in Table 2.
Navigation protocol
A surgical navigation system (BLU-IGS, Orthokey, Lewes, Delaware) [26] and a specific software (KLEE, Orthokey, Lewes, Delaware) [25] were used to acquire anatomical landmarks and passive joint kinematics [24]. This system was reported by the producer to have a 3D RMS volumetric accuracy of 0.350 mm and a 3D RMS volumetric repeatability of 0.200 mm [46].
The anatomical and kinematic data were collected by the two Senior Authors (MM and FI) after medial parapatellar arthrotomy, before anterior cruciate ligament (ACL) and meniscal removal and after cementing final implant. All the data were analysed offline using the Matlab software (Mathworks, Natick, MA, USA).
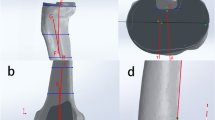
The joint coordinate reference system (JCS) was defined according to Cole et al. [7] and Grood and Suntay [17]. Anatomical landmarks acquired during the procedure are shown in Fig. 1. The functional hip-joint centre (HJC) was identified through a pivoting motion, as described by Siston et al. [36]. By a femoral circumduction movement, the surgeon first located the hip centre and then used the stylus tracked by the navigation system to establish the standard anatomical landmarks, to compute the reference system in the femur and tibia (femoral epicondyles, femoral intercondylar notch, tibial malleoli, tibial spine and tibial tuberositas) [8, 24] (Fig. 1).
For the femoral anatomical reference system, the proximal–distal (PD) axis was defined with the femoral mechanical axis [14], i.e. the line connecting the HJC and the deepest point in the femoral notch (FN), as defined by Bertin [6]. The medial–lateral (ML) axis was defined as the sTEA, i.e. the line connecting the medial sulcus of the medial epicondyle (MFE) and the lateral epicondyle (LFE), defined as the most lateral prominence of the lateral femoral condyle [3, 5]. The cross-product between the PD- and ML-axis was defined as the anterior-posterior (AP) axis (Fig. 1).
For the tibial anatomical reference system, the PD-axis was defined as the tibial mechanical axis, i.e. the line connecting the tibial spine (TS) and the midpoint between the medial (MM) and the lateral (LM) malleoli. The AP-axis was defined as the projection of tibial tuberosity (TT) to the PD-axis, and the ML-axis, as the cross-product between PD-axis and ML-axis [24] (Fig. 1).
FFA acquisition
The knee was cycled through three complete passive range of motions (PROM), from full extension to 120° of flexion and back to full extension, before and after implant positioning. For each patient, the preoperative FFA acquisition was performed after medial parapatellar arthrotomy to allow acquisition of anatomical landmarks, with intact menisci and ACL, using a temporary suture repair to reduce the patella in its anatomical position. In all acquisitions, the movement was performed while maintaining the femur elevated with one hand and holding the heel in neutral position with the open palm of the other hand, without superimposing any additional load [24, 26] and allowing the physiological rotations of the leg. The FFA was computed using the MHA algorithm [35]. The angle between the FFA and the surgical TEA was determined on the frontal (α F-pre) and the axial (α A-pre) plane (Fig. 2). The navigation technology was used to determine implant positioning. The femoral component rotational positioning was determined according to the sTEA [2, 44]. After the final implant positioning and the capsular closure, the postoperative FFA acquisition was performed, repeating the same movement. The angle between the FFA and the surgical TEA was again determined on the frontal (α F-post) and the axial (α A-post) plane (Fig. 2).
a, b Illustrates the angle between FFA and surgical TEA on frontal and axial plane before TKR implantation. c, d Illustrates the angle between FFA and surgical TEA after final implant positioning. The drawing illustrates a significant modification of FFA position with respect to TEA only on frontal plane and underlines that preoperative FFA is in a more varus position respect to TEA
A varus position of the FFA, with respect to the sTEA in frontal plane, was assigned a negative value, while a valgus orientation of the FFA to the sTEA was assigned a positive value. On axial plane, we assigned negative values to internal rotations of the FFA with respect to the sTEA, while positive values were assigned to external rotations of the FFA with respect to the sTEA (Fig. 2).
The inter- and intraobserver variability of the FFA acquisition was determined [9]. The angle between the FFA and the transepicondylar axis demonstrated a good repeatability coefficient, ranging between 4.4° and 3.4°. The intraclass correlation coefficient (ICC) ranged between 0.87 and 0.93 with a standard deviation between 1.3° and 1.0° [9].
Data analysis
The Grood and Suntay algorithm [17] was used to describe the relative motion of the tibial frame with respect to the femoral one. Knee kinematics during PROM were described by means of instantaneous flexion–extension (FE), internal–external (IE) and varus–valgus (VV) rotations.
Starting from the instantaneous helical axes (IHA), elaborated for each PROM with a least square approach [49], the mean helical axis (MHA) was computed and defined as the functional flexion axis (FFA) [35].
The study was approved by the Institutional Review Board of the Istituto Ortopedico Rizzoli (Bologna, Italy, protocol number 11551/CE/US/ml, 5 May 2006), and all patients provided their informed consent to the operating surgeon.
Statistical analysis
Descriptive statistical analysis was performed to evaluate data distribution both on pre- and postimplant values.
The paired Student’s t test was performed to investigate the difference between α F-pre and α F-post and between α A-pre and α A-post. The Pearson correlation was used to test whether a relationship exists between both α F and α A, before and after implant positioning and preoperative limb alignment determined with the HKA angle. Statistical significance was set to 95 % (p = 0.05) for all tests. Values were expressed as mean ± standard deviation.
The minimum sample size was prospectively estimated for a two-tailed paired Student’s t test with a power of 95 %, starting from the hypothesis of a mean of difference of 2.3° ± 5.4° between pre- and postoperative angles in the frontal plane and of −0.7° ± 1.0° in the axial plane (referring to Colle et al. [8]. Considering a minimum 15 % dropout rate in a possible long-run follow-up (given the intention to perform further additional long-term biomechanical analyses on this group), we decided to enrol at least 85 patients.
Results
Data distribution was analysed for α F and α A angles, and both pre- and postimplant data are normally distributed (Shapiro–Wilk coefficient > 0.15).
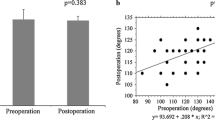
The difference between preoperative and postoperative FFA on frontal plane was 3.2° ± 11.7° (p < 0.0001). No significant difference was found between pre- and postoperative FFA on axial plane (Fig. 2; Table 2).
A poor correlation was found between FFA orientation and preoperative limb alignment on frontal plane (Fig. 4; Table 3), while no correlation was found on axial plane (Fig. 3; Table 3).
Pre- and postoperative values of limb alignment are reported in Table 2.
Discussion
The most important finding of this study was that the TKA procedure modifies the FFA in patients with end-stage OA only on frontal plane. In fact, no difference was found between the pre- and postoperative FFA on the axial plane. A poor correlation was found between the preoperative FFA orientation on the frontal plane and the preoperative limb alignment, whereas no correlation was found between the preoperative FFA orientation on the axial plane and the preoperative limb alignment. The axial rotation of the femoral component is a key factor for achieving well-balanced flexion gap, tibiofemoral alignment and patellofemoral congruency through flexion [18, 34, 43, 47]. The optimal surgical reference to optimize rotational positioning of the femoral component during TKA is an open issue. The navigation technology has been suggested to improve the accuracy of implant positioning and to reduce the number of outliers in the frontal and axial alignment [4, 11, 39, 41].
Previous studies [12, 19] have demonstrated the poor reproducibility of the TEA acquisitions, even using a navigation system, thus showing its limited usefulness as reference to set femoral component rotation. Conversely, other reports [25, 37] have demonstrated that the TEA remains the gold standard among anatomical landmarks. The same debate exists about the accuracy of others anatomical landmarks such as the Whiteside line [2, 42] and the posterior condylar line [16, 22, 29], confirming that in the literature, the question of which is the optimal reference for the femoral component positioning in TKA still remains.
Recently, kinematically derived knee flexion axis has been suggested as a more reproducible and reliable reference to optimize femoral component positioning in TKA [8, 12, 28, 31] over conventional anatomical references. To the best of our knowledge, no study analysed the kinematically derived FFA estimation, both in pre- and in postimplant conditions in navigated TKA, in relation to the amount of preoperative knee varus deformity.
The present study demonstrated in vivo that TKA modifies the FFA only on frontal plane. Indeed, no difference was found between the pre- and postoperative FFA on axial plane. Moreover, a poor correlation was only found between the preoperative FFA orientation and the preoperative limb alignment on the frontal plane, but not on the axial plane. This finding could be explained according to Repicci’s “extension-gap disease”: in a varus knee with OA, the cartilage and subchondral bone erosion are mainly present on the weight-bearing surface of the medial femoral condyle [32, 33]. The preoperative FFA position on the frontal plane may be influenced by this wear pattern and the postoperative FFA changing could be due either to prosthesis femoral component that replaces the wear and neutral mechanical alignment of the implant. On axial plane, the absence of wear on the posterior aspect of the medial femoral condyle and its circular shape are not altered by femoral component implantation.
This study has some limitations. Valgus knees were not included. As suggested by Akagi et al. [1], in valgus knees, an hypoplasia of the lateral femoral condyle exists and modifies the femoral rotation throughout the ROM. Further investigation is going on to have a sufficient sample size of patients with primary OA and preoperative valgus deformity.
The FFA position was referred to the position of the sTEA, because it was the most easily identifiable anatomical landmark on both frontal and axial plane. The sTEA is widely accepted as gold standard for intraoperative rotational positioning of the femoral component with a non-minimally invasive approach, with good direct visualization of the epicondyles and when surgery is performed by an expert surgeon [5, 27, 30, 40, 50, 51]. No CT scan was used to confirm the sTEA position because neither the comparison between intraoperative and radiological acquisition of the TEA nor the correspondence between the TEA and the FFA were the purposes of the present study. The sTEA was used as reference to evaluate FFA changes. Indeed, the sTEA was the same before and after implant positioning; therefore, every change of the angle between the TEA and the FFA depends on the change of the FFA orientation.
The preoperative FFA acquisition was performed after medial parapatellar capsulotomy. Oussedik et al. [31] and Doro et al. [12] have already demonstrated that the FFA is not influenced by this surgical exposure, but further investigation could be useful to underline a possible contribution of capsule on the FFA of the native knee.
The kinematically determined FFA could be influenced by tourniquet use and absence of active muscle contraction in the patient under anaesthesia, as already underlined by Oussedik et al. [31]. Further investigation is needed to evaluate the contribution of active muscle contraction to knee kinematics.
Even if further investigation is needed to determine the FFA in different conditions (i.e. valgus knees or different prosthesis designs), the present study has demonstrated that the FFA could be used as a functional reference for femoral component positioning in the axial plane. The amount of limb deformity did not affect the FFA estimation confirming its possible usefulness in the daily clinical practice as a good alternative choice in navigated TKA with respect to conventional surgical methods. Indeed, the FFA methodology relies on individual knee motion, thus bypassing eventual biases that increase the variability in determining conventional anatomical landmarks, particularly in computer-assisted TKA.
Conclusion
The present study demonstrates that TKA in varus knees with end-stage OA significantly modifies the orientation of the FFA only on frontal plane. In addition, the position of the FFA on frontal plane may depend on preoperative limb alignment. The position of the FFA on axial plane is not related to the amount of varus deformity and is not modified by TKA. The FFA methodology could be used as a n alternative functional reference for femoral component positioning in the axial plane.
References
Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T (2001) Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res 388:147–156
Arima J, Whiteside LA, McCarthy DS, White SE (1995) Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone Joint Surg Am 77:1331–1334
Asano T, Akagi M, Nakamura T (2005) The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty 20:1060–1067
Bäthis H, Perlick L, Tingart M, Lüring C, Zurakowski D, Grifka J (2004) Alignment in total knee arthroplasty. A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br 86:682–687
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Bertin K (1991) Intramedullary instrumentation for total knee arthroplasty. V Goldberg (Ed.), Controversies of total knee arthroplasty, Presented at the Zimmer Orthopaedic Symposium, Scottsdale, AZ, 1989, Raven Press, New York :175
Cole GK, Nigg BM, Ronsky JL, Yeadon MR (1993) Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng 115:344–349
Colle F, Bignozzi S, Lopomo N, Zaffagnini S, Sun L, Marcacci M (2012) Knee functional flexion axis in osteoarthritic patients: comparison in vivo with transepicondylar axis using a navigation system. Knee Surg Sports Traumatol Arthrosc 20:552–558
Colle F, Lopomo N, Bruni D, Visani A, Iacono F, Zaffagnini S, Marcacci M (2014) Analysis of knee functional flexion axis in navigated TKA: identification and repeatability before and after implant positioning. Knee Surg Sports Traumatol Arthrosc 22:694–702
Deakin AH, Basanagoudar PL, Nunag P, Johnston AT, Sarungi M (2012) Natural distribution of the femoral mechanical-anatomical angle in an osteoarthritic population and its relevance to total knee arthroplasty. Knee 19:120–123
Decking R, Markmann Y, Fuchs J, Puhl W, Scharf H-P (2005) Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty 20:282–288
Doro LC, Hughes RE, Miller JD, Schultz KF, Hallstrom B, Urquhart AG (2008) The reproducibility of a kinematically-derived axis of the knee versus digitized anatomical landmarks using a knee navigation system. Open Biomed Eng J 2:52–56
Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J (2007) Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop 461:238–244
Gamage SSHU, Lasenby J (2002) New least squares solutions for estimating the average centre of rotation and the axis of rotation. J Biomech 35:87–93
Garg A, Walker PS (1990) Prediction of total knee motion using a three-dimensional computer-graphics model. J Biomech 23:45–58
Griffin FM, Insall JN, Scuderi GR (1998) The posterior condylar angle in osteoarthritic knees. J Arthroplasty 13:812–815
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105:136–144
Harman MK, Banks SA, Kirschner S, Lützner J (2012) Prosthesis alignment affects axial rotation motion after total knee replacement: a prospective in vivo study combining computed tomography and fluoroscopic evaluations. BMC Musculoskelet Disord 13:206
Jenny JY, Boeri C (2004) Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop 75:74–77
Kellegren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kurosawa H, Walker PS, Abe S, Garg A, Hunter T (1985) Geometry and motion of the knee for implant and orthotic design. J Biomech 18:487–499
Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB (2010) Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc 18:381–387
Marin F, Sangeux M, Charleux F, Ho Ba Tho M-C, Dürselen L (2006) Can a finite set of knee extension in supine position be used for a knee functional examination? J Biomech 39:359–363
Martelli S, Zaffagnini S, Bignozzi S, Bontempi M, Marcacci M (2006) Validation of a new protocol for computer-assisted evaluation of kinematics of double-bundle ACL reconstruction. Clin Biomech Bristol Avon 21:279–287
Martelli S, Lopomo N, Greggio S, Ferretti E, Visani A (2006) Development and applications of a software tool for diarthrodial joint analysis. Comput Methods Prog Biomed 83:50–56
Martelli S, Zaffagnini S, Bignozzi S, Lopomo NF, Iacono F, Marcacci M (2007) KIN-Nav navigation system for kinematic assessment in anterior cruciate ligament reconstruction: features, use, and perspectives. Proc Inst Mech Eng [H] 221:725–737
Matsuda S, Matsuda H, Miyagi T, Sasaki K, Iwamoto Y, Miura H (1998) Femoral condyle geometry in the normal and varus knee. Clin Orthop Relat Res 349:183–188
Matziolis G, Pfiel S, Wassilew G, Boenicke H, Perka C (2011) Kinematic analysis of the flexion axis for correct femoral component placement. Knee Surg Sports Traumatol Arthrosc 19:1504–1509
Moon YW, Seo JG, Lim SJ, Yang JH (2010) Variability in femoral component rotation reference axes measured during navigation-assisted total knee arthroplasty using gap technique. J Arthroplasty 25:238–243
Olcott CW, Scott RD (1999) The ranawat award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res 367:39–42
Oussedik S, Scholes C, Ferguson D, Roe J, Parker D (2012) Is femoral component rotation in a TKA reliably guided by the functional flexion axis? Clin Orthop Relat Res 470:3227–3232
Repicci JA (2003) Mini-invasive knee unicompartmental arthroplasty: bone-sparing technique. Surg Technol Int 11:282–286
Repicci JA, Hartman JF (2004) Minimally invasive unicondylar knee arthroplasty for the treatment of unicompartmental osteoarthritis: an outpatient arthritic bypass procedure. Orthop Clin North Am 35:201–216
Romero J, Stähelin T, Binkert C, Pfirrmann C, Hodler J, Kessler O (2007) The clinical consequences of flexion gap asymmetry in total knee arthroplasty. J Arthroplasty 22:235–240
Sheehan FT (2007) The finite helical axis of the knee joint (a non-invasive in vivo study using fast-PC MRI). J Biomech 40:1038–1047
Siston RA, Delp SL (2006) Evaluation of a new algorithm to determine the hip joint center. J Biomech 39:125–130
Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ (2005) The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 87:2276–2280
Siu D, Rudan J, Wevers HW, Griffiths P (1996) Femoral articular shape and geometry. A three-dimensional computerized analysis of the knee. J Arthroplasty 11:166–173
Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A (2003) Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br 85:830–835
Stiehl JB, Abbott BD (1995) Morphology of the transepicondylar axis and its application in primary and revision total knee arthroplasty. J Arthroplasty 10:785–789
Stulberg SD, Loan P, Sarin V (2002) Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am 84-A Suppl 2:90–98
Vanin N, Panzica M, Dikos G, Krettek C, Hankemeier S (2011) Rotational alignment in total knee arthroplasty: intraoperative inter- and intraobserver reliability of whiteside’s line. Arch Orthop Trauma Surg 131:1477–1480
Verlinden C, Uvin P, Labey L, Luyckx JP, Bellemans J, Vandenneucker H (2010) The influence of malrotation of the femoral component in total knee replacement on the mechanics of patellofemoral contact during gait: an in vitro biomechanical study. J Bone Joint Surg Br 92:737–742
Victor J (2009) Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 95:365–372
Weidow J, Kärrholm J, Saari T, McPherson A (2007) Abnormal motion of the medial femoral condyle in lateral knee osteoarthritis. Clin Orthop Relat Res 454:27–34
Wiles AD, Thompson DG, Frantz DD (2004) Accuracy assessment and interpretation for optical tracking systems. In: Proceedings of SPIE medical imaging 2004 Vis. Image-Guid Proced Disp 5367:421–432
Wolterbeek N, Garling EH, Mertens BJA, van der Linden HMJ, Nelissen RGHH, Valstar ER (2012) Kinematics of a highly congruent mobile-bearing total knee prosthesis. Knee Surg Sports Traumatol Arthrosc 20:2487–2493
Woltring HJ (1994) 3-D attitude representation of human joints: a standardization proposal. J Biomech 27:1399–1414
Woltring HJ, Huiskes R, de Lange A, Veldpaus FE (1985) Finite centroid and helical axis estimation from noisy landmark measurements in the study of human joint kinematics. J Biomech 18:379–389
Yau WP, Leung A, Liu KG, Yan CH, Wong LS, Chiu KY (2008) Errors in the identification of the transepicondylar and anteroposterior axes of the distal femur in total knee replacement using minimally-invasive and conventional approaches: a cadaver study. J Bone Joint Surg Br 90:520–526
Yoshioka Y, Siu D, Cooke TD (1987) The anatomy and functional axes of the femur. J Bone Joint Surg Am 69:873–880
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iacono, F., Bruni, D., Bignozzi, S. et al. Does total knee arthroplasty modify flexion axis of the knee?. Knee Surg Sports Traumatol Arthrosc 22, 1728–1735 (2014). https://doi.org/10.1007/s00167-014-3054-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3054-x