Abstract
Purpose
Meniscal injury resulting in segmental loss of meniscal tissue is a major risk factor for the development of osteoarthritis. Tissue engineering strategies have provided scaffolds for meniscal regeneration in order to establish a treatment option for patients with limited opportunities for meniscal reconstruction. The purpose of this study was to assess the clinical and magnetic resonance imaging (MRI) results 2 years after implantation of a polyurethane scaffold for chronic segmental medial meniscus deficiency following partial medial meniscectomy.
Methods
Eighteen patients were treated with arthroscopic implantation of an ActiFit® (Orteq Sports Medicine) polyurethane meniscal scaffold for meniscus deficiency of the medial meniscus. Patients were followed up at 6, 12, and 24 months. Clinical outcome was assessed using patient-reported outcome scores (KOOS, KSS, UCLA activity scale, VAS for pain). Radiological outcome was assessed using MRI at 6, 12, and 24 months by evaluating scaffold morphology, scaffold integration, and additional joint injury, as well as joint inflammation.
Results
Eighteen patients with a median age of 32.5 years (range 17–49) were enrolled. Statistically significant improvements were present in all patients, but one at 2 years compared to baseline in all categories. Complete resorption of the scaffold occurred in one patient representing a failure to treatment. MRI showed abnormal signal intensity of the scaffold when compared to residual meniscal tissue but without synovitis or joint inflammation. Extrusion of the scaffold was present in four patients. No correlation between scaffold extrusion and clinical outcome was observed.
Conclusion
Arthroscopic implantation of a polyurethane meniscal scaffold in patients with chronic segmental medial meniscus deficiency is not only a safe procedure but leads to good clinical results at a 2-year follow-up. Scaffold extrusion did not appear to affect clinical outcome.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal tears are common as a result of both degenerative and traumatic knee joint conditions. An intact meniscus is necessary for normal knee joint function and in preventing osteoarthritis by reducing high peak stress of the articular cartilage by achieving homogeneous load distribution [23, 31]. Whilst repair of meniscal lesions is ideal, it is not always achievable, especially in tears localized in the avascular or “white zone” of the meniscus [23]. In these irreparable lesions, partial meniscectomy is the gold standard treatment. Unfortunately, this may result in near complete loss of meniscal function, thus representing a significant risk factor for the development of osteoarthritis [2, 6, 7]. A treatment option for these patients is tissue engineering, in which meniscal scaffolds serve as a template for tissue ingrowth [21].
The Actifit® meniscal implant (Orteq Sports Medicine, London, UK) is a biodegradable, synthetic, acellular scaffold composed of aliphatic polyurethane. Its purpose is to re-establish meniscal function by filling the resulting defect after partial meniscectomy. It is a highly porous structure that encourages tissue ingrowth, theoretically reducing the risk of osteoarthritis in the future. Verdonk et al. [30] demonstrated this result in a multicenter study with the same scaffold. Biopsies taken at 12 months showed tissue infiltration without signs of cell death or necrosis in 97 % of cases. Efe et al. [5] also confirmed its feasibility and efficacy and demonstrated the first favourable clinical results at 1-year post-surgery.
The aim of the present study was to report the clinical and MRI results in patients treated with a polyurethane scaffold for medial meniscus deficiency at 2-year follow-up. This follow-up period represents a longer follow-up than the previous publication from 2012 [5] and thus provides more information concerning not only the safety of the procedure but additionally concerning the clinical benefit for the treated patient.
Materials and methods
This is a case series of patients from the Department of Orthopaedics and Rheumatology of the University Hospital Marburg treated with a polyurethane meniscus scaffold as a result of segmental medial meniscus deficiency secondary to previous partial meniscectomy. All patients gave written informed consent before participation in the study. Inclusion criteria were as follows: (1) chronic, symptomatic, irreparable medial meniscus lesion or partial meniscal loss with an intact peripheral rim and anterior and posterior horns; (2) age 16–50 years; (3) stable knee joint or a joint which was stabilized within 12 weeks prior to surgery; (4) International Cartilage Repair Society (ICRS) articular cartilage classification ≤2 in the medial compartment; and (5) normal joint alignment (mechanical tibiofemoral angle ≤3°).
Implantation was performed arthroscopically via a standard anterolateral and anteromedial portal. The irreparable meniscus was trimmed back to the vascular zone. The defect was measured and the scaffold was cut to fit into the resulting defect including the recommended oversizing of the scaffold by 10 %. The implant was then sutured in place using a hybrid suture technique with a median of 3 Ultra Fast-Fix® implants (range 3–6; Smith and Nephew Endoscopy, Andover, MA) and a maximum of 2 outside-in sutures.
Patients were followed up at 6, 12, and 24 months. Clinical outcome was assessed using patient-reported outcome scores (KOOS [24, 25], KSS [17], UCLA activity scale [27], and VAS for pain [10]).
Radiological outcome was assessed using MRI performed at 6, 12, and 24 months. MRI scans were taken on a 1.5-Tesla MRI scanner (MAGNETOM Espree, Siemens, Erlangen, Germany) using gradient-echo T2-weighted, spin-echo T1-weighted, fat saturation fast spin-echo, and T2-weighted sequences in coronal, sagittal, and transverse slice orientations. The scaffold itself was described following Genovese [14] and the untreated contralateral meniscus of the same knee was evaluated using the classification of Reicher [22]. The reaction of the subchondral bone was assessed according to Lynch [19]. Meniscus extrusion was measured on coronal view as described by De Coninck et al. [3]. All scans were assessed by the same radiologist.
Data from a subgroup of this study cohort were previously published to assess the feasibility and safety of the procedure [5].
The study was performed in accordance with the Declaration of Helsinki and was authorized by the research and ethics committee of the University Hospital Marburg, Germany (ID number 194/09).
Statistical analysis
For a sample size of 18 patients, all data were inputted into Graphpad Prism 5 software package (Graphpad Inc. La Jolla, CA). Comparisons between mean scores were made using a paired Student’s t test with a significance level set at P < 0.05.
Results
All eighteen patients included (median age 32.5 years, range 17–49 years) completed follow-up to 24 months. No patients were lost to follow-up and no intra-operative complications were perceived. No concomitant ACL reconstructions or other stabilizing procedures were performed prior to surgery. One patient showed complete resorption of the scaffold and has to be considered a failure to treatment. Meniscal defect size and consecutive scaffold size ranged from 35 to 62 mm in length (mean length: 45 mm).
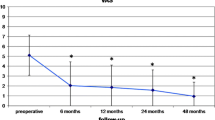
Patient-reported outcome
The complete summary of all clinical data is shown in Table 1. There was a constant improvement of the UCLA activity scale over time. But a statistically significant increase when compared to the preoperative baseline was only achieved concerning the UCLA activity scale at 2-year follow-up (P < 0.05; Fig. 1). Concerning the reduction in pain measured by means of the VAS, there was a statistically significant reduction in pain already at 6-month follow-up (P < 0.05) that continued over time and lasted until the 2-year follow-up point (P < 0.05; Fig. 2). The KSS showed statistically significant improvements in both subdomains of the scale beginning at 6 months until the last follow-up visit for both the functional score and the knee score (function score: P < 0.05 and knee score: P < 0.05; Fig. 3). Statistically significant improvements in all subdomains of the KOOS were observed from 6-month post-operatively until 2 years, compared with the preoperative baseline (P < 0.05; Fig. 4). But a continuous improvement over the whole follow-up period could only be observed in the “Activity of daily life” and the “pain” subscale. The other three subscales (symptom, sport, and quality of life) showed a comparable increase over time until 1-year post-operative and then showed a slight deterioration without statistical significance when comparing the results at 1 year and at 2-year follow-up (Table 1).
Magnetic resonance imaging
Three of the 18 implants showed a partial meniscal extrusion; another demonstrated complete extrusion on MRI. Complete resorption of the scaffold was observed in one patient between 12 and 24 months on MRI. Although no joint effusion, synovitis or other signs of inflammation were present in the joint, the patient with the complete scaffold resorption was the only one who was not satisfied with the procedure, despite achieving good clinical scores. MRI showed altered, hyperintense signal intensity of all scaffolds when compared to the residual meniscal tissue (Fig. 5). Diffuse bone bruising and subchondral oedema, observed in eight patients (44 %) at 6 months, completely resolved at 12 months and did not recur in any patient at 24 months. With regard to the changes of the articular cartilage in the affected medial compartment, MRI at 6 months and at 2 years showed a marked interval progression (one or more grades by the ICRS classification) in two patients. On the other hand, a relevant improvement in chondral wear was seen in five patients at 24 months. No statistically significant difference was found in overall chondral damage.
Discussion
The most important finding of the present study was that the Actifit® meniscal scaffold led to favourable clinical results at 2-year follow-up, with significant improvements from preoperative baseline beginning from 6 months after surgery. MRI showed an absence of inflammatory joint reactions, such as synovitis or effusion, which is considered a stable situation for the articular cartilage and scaffolds in 17 of 18 patients.
Since establishing the importance of an intact meniscus for physiological joint kinematics and knee function, surgeons aim to preserve as much meniscal tissue as possible [20]. A recently published meta-analysis has demonstrated that clinical results and activity level are significantly better after meniscal repair when compared to meniscectomy [32]. Fetzer et al. [9] reported that in 1,014 patients, only 35 % of medial meniscal tears and 55 % of lateral meniscal tears were eligible for scaffold replacement; although contemporary repair techniques were used, most tears in their cohort were not repairable.
Early results of meniscal replacement with a collagen-based scaffold, compared with meniscectomy, showed the first significant results at 10 years, which led to the conclusion that meniscal replacement may help to prevent osteoarthritis in the long term [33]. This led to the development of different scaffolding methods, with two currently in clinical use and others in animal models [8, 11, 13, 21].
The use of the polyurethane scaffold in this study has not only led to a significant improvement in reported pain level, (represented by ongoing improvements in VAS reaching statistical significance by 6 months), but also daily activities and sports represented by significant improvements in the UCLA activity scale and the sport subscale of the KOOS (27 preoperatively to 61 at 6 months). Interestingly, overall clinical results continued to improve after 1 year, reaching statistical significance in the UCLA activity scale at 2 years. These clinical results were consistent with that reported in the literature. Zaffagnini et al. [33] who used a collagen-based meniscal implant (Menaflex®—ReGen Biologics) reported favourable clinical results 6–8 years after surgery. Hirschmann et al. [16] used a collagen meniscus substitution and reported good clinical results despite significant remodelling, degradation, resorption, and extrusion of the implant in most of the patients. Kon et al. [18] and Verdonk et al. [28] who used the same polyurethane scaffold as in the present study reported favourable results using the IKDC and Tegner score (Kon et al.) and similar results for KOOS and VAS pain (Verdonk et al.) 2 years after surgery, respectively. Spencer et al. [26] compared both scaffolds at 1 year, reporting good clinical results in both groups with variable amount of meniscal tissue regeneration in a second-look arthroscopy. Recently, a series was published by Bouyarmane et al. [1] who used the same type of scaffold for the lateral meniscus in 54 patients and reported similar results when compared to the results of this study concerning pain reduction by means of the VAS and functional outcome by means of the KOOS, indicating that the scaffold as well as the surgical approach are also suitable for the challenging lateral compartment. The authors noted no progression of chondral wear, which was present at the time of surgery, within a follow-up period of 1 year [26]. These results may suggest a slow time to achieve maximal clinical improvements, which is consistent with many other biological procedures.
Another aspired advantage of meniscal scaffolds is a potential chondroprotective effect. This hypothesis cannot be assessed within the short follow-up interval of the present study. Especially, as we do recognize that there is no control group for comparison to make strong conclusions. But the fact that MRI demonstrated a stable chondral situation in most patients (16 of 18, 89 %) and showed no significant chondral changes overall after 24 months gives rise to the hope that longer follow-up periods might show this desired effect. Interestingly, the two patients who showed progression of chondral wear were those with high activity and no pain according to the VAS (VAS = 0). The KSS score showed 100/100 and 100/95, respectively; the KOOS subscale sport reached 90 and 95 in both patients, respectively.
One patient showed complete resorption of the scaffold, which took place between 12 and 24 months on MRI. This patient showed a relatively high pain level, as represented by a VAS of 5 and deterioration in all clinical scores. This patient changed his answer from “yes” at 12 months to “no” at 24 months with regard to satisfaction, representing the only real failure to treatment. No inflammatory joint reaction was present at 24 months on MRI in this patient. Longer follow-up periods are necessary to assess whether resorption happens over time in other patients, or if this is a single event.
Another important result was the fact that 22 % of patients (4 of 18) demonstrated scaffold extrusion to some extent, with complete extrusion in one patient. Extrusion or radial displacement of native menisci has already been reported and is considered pathologic if it equals or exceeds 3 mm [3]. As a displaced meniscus can no longer fulfil its purpose of reducing peak pressure and achieving balanced load distribution for the articular cartilage, meniscal extrusion is supposedly a prearthritic condition [12]. In native menisci, extrusion is mostly due to radial meniscal tears or degenerative root tears [3].
Little data are currently available concerning the mechanism that leads to extrusion of meniscal scaffolds or how to prevent it. De Coninck et al. [4], who implanted the same polyurethane scaffold, reported radial displacement of all medial meniscal scaffolds (15 patients) at 2 years. In the present cohort, only 4 of 18 patients showed meniscal extrusion at 2 years, but with an increasing tendency over time. De Coninck et al. [4] stated that radial displacement was observed preoperatively in the native but already injured meniscus, and increased in the medial menisci after scaffold implantation. Whether extrusion is due to a preoperatively existing ligamentous instability of the meniscus caused by a lesion of it’s fixation (i.e. rupture of meniscotibial ligaments and/or popliteomeniscal fascicles), or whether the scaffold itself is a risk factor for meniscal extrusion (due to overstuffing or scaffold consistency) requires further investigation [4, 29]. The results of the present study are consistent with the literature, in that no correlation between meniscal extrusion and clinical results after meniscal scaffold implantation was found at this short follow-up [4, 15, 29]. One theory is that extrusion does not impair the chondroprotective function of the menisci [15]. Verdonk et al. [29] explained the lack of correlation between extrusion and clinical results by overstuffing of the joint space, which results in a necessary extrusion but maintains meniscal function.
The primary limitations of this present study include a small sample size, the lack of a meniscectomy control group and short-term follow-up, which limits the evaluation of the chondroprotective effect of the meniscal scaffold. However, the results can be used to confirm the safety and efficacy of this scaffold at 2 years following surgery, with consistently improved patient-reported outcome and positive imaging findings being reported. If the long-term follow-up results can keep up with the current results, this scaffold could provide an excellent treatment option for chronic medial meniscus deficiency.
Conclusion
Arthroscopic implantation of a polyurethane meniscal scaffold in patients with chronic medial meniscus deficiency leads to good short-term clinical results. MRI showed a stable articular cartilage surface with a number of cases demonstrating scaffold extrusion. However, the observed extrusion did not result in deleterious clinical results.
References
Bouyarmane H, Beaufils P, Pujol N, Bellemans J, Roberts S, Spalding T, Zaffagnini S, Marcacci M, Verdonk P, Womack M, Verdonk R (2014) Polyurethane scaffold in lateral meniscus segmental defects: clinical outcomes at 24 months follow-up. Orthop Traumatol Surg Res 100:153–157
Burks RT, Metcalf MH, Metcalf RW (1997) Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy 13:673–679
Choi CJ, Choi YJ, Lee JJ, Choi CH (2010) Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26:1602–1606
De Coninck T, Huysse W, Willemot L, Verdonk R, Verstraete K, Verdonk P (2013) Two-year follow-up study on clinical and radiological outcomes of polyurethane meniscal scaffolds. Am J Sports Med 41:64–72
Efe T, Getgood A, Schofer MD, Fuchs-Winkelmann S, Mann D, Paletta JR, Heyse TJ (2012) The safety and short-term efficacy of a novel polyurethane meniscal scaffold for the treatment of segmental medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc 20:1822–1830
Englund M, Guermazi A, Lohmander LS (2009) The meniscus in knee osteoarthritis. Rheum Dis Clin North Am 35:579–590
Englund M, Roos EM, Lohmander LS (2003) Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum 48:2178–2187
Esposito AR, Moda M, Cattani SM, de Santana GM, Barbieri JA, Munhoz MM, Cardoso TP, Barbo ML, Russo T, D’Amora U, Gloria A, Ambrosio L, Duek EA (2013) PLDLA/PCL-T Scaffold for meniscus tissue engineering. Biores Open Access 2:138–147
Fetzer GB, Spindler KP, Amendola A, Andrish JT, Bergfeld JA, Dunn WR, Flanigan DC, Jones M, Kaeding CC, Marx RG, Matava MJ, McCarty EC, Parker RD, Wolcott M, Vidal A, Wolf BR, Wright RW (2009) Potential market for new meniscus repair strategies: evaluation of the MOON cohort. J Knee Surg 22:180–186
Flandry F, Hunt JP, Terry GC, Hughston JC (1991) Analysis of subjective knee complaints using visual analog scales. Am J Sports Med 19:112–118
Fox DB, Warnock JJ (2011) Cell-based meniscal tissue engineering: a case for synoviocytes. Clin Orthop Relat Res 469:2806–2816
Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D (1999) Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis Cartilage 7:526–532
Galley NK, Gleghorn JP, Rodeo S, Warren RF, Maher SA, Bonassar LJ (2011) Frictional properties of the meniscus improve after scaffold-augmented repair of partial meniscectomy: a pilot study. Clin Orthop Relat Res 469:2817–2823
Genovese E, Angeretti MG, Ronga M, Leonardi A, Novario R, Callegari L, Fugazzola C (2007) Follow-up of collagen meniscus implants by MRI. Radiol Med 112:1036–1048
Ha JK, Shim JC, Kim DW, Lee YS, Ra HJ, Kim JG (2010) Relationship between meniscal extrusion and various clinical findings after meniscus allograft transplantation. Am J Sports Med 38:2448–2455
Hirschmann MT, Keller L, Hirschmann A, Schenk L, Berbig R, Luthi U, Amsler F, Friederich NF, Arnold MP (2013) One-year clinical and MR imaging outcome after partial meniscal replacement in stabilized knees using a collagen meniscus implant. Knee Surg Sports Traumatol Arthrosc 21:740–747
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Kon E, Filardo G, Zaffagnini S, Di Martino A, Di Matteo B, Marcheggiani Muccioli GM, Busacca M, Marcacci M (2014) Biodegradable polyurethane meniscal scaffold for isolated partial lesions or as combined procedure for knees with multiple comorbidities: clinical results at 2 years. Knee Surg Sports Traumatol Arthrosc 22:128–134
Lynch TC, Crues JV 3rd, Morgan FW, Sheehan WE, Harter LP, Ryu R (1989) Bone abnormalities of the knee: prevalence and significance at MR imaging. Radiology 171:761–766
McDermott ID, Amis AA (2006) The consequences of meniscectomy. J Bone Joint Surg Br 88:1549–1556
Pereira H, Frias AM, Oliveira JM, Espregueira-Mendes J, Reis RL (2011) Tissue engineering and regenerative medicine strategies in meniscus lesions. Arthroscopy 27:1706–1719
Reicher MA, Hartzman S, Duckwiler GR, Bassett LW, Anderson LJ, Gold RH (1986) Meniscal injuries: detection using MR imaging. Radiology 159:753–757
Rodkey WG (2000) Basic biology of the meniscus and response to injury. Instr Course Lect 49:189–193
Roos EM, Lohmander LS (2003) The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64–71
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Spencer SJ, Saithna A, Carmont MR, Dhillon MS, Thompson P, Spalding T (2012) Meniscal scaffolds: early experience and review of the literature. Knee 19:760–765
Terwee CB, Bouwmeester W, van Elsland SL, de Vet HC, Dekker J (2011) Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis Cartilage 19:620–633
Verdonk P, Beaufils P, Bellemans J, Djian P, Heinrichs EL, Huysse W, Laprell H, Siebold R, Verdonk R (2012) Successful treatment of painful irreparable partial meniscal defects with a polyurethane scaffold: two-year safety and clinical outcomes. Am J Sports Med 40:844–853
Verdonk P, Depaepe Y, Desmyter S, De Muynck M, Almqvist KF, Verstraete K, Verdonk R (2004) Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc 12:411–419
Verdonk R (2011) The meniscus: past, present and future. Knee Surg Sports Traumatol Arthrosc 19:145–146
Verdonk R, Verdonk P, Huysse W, Forsyth R, Heinrichs EL (2011) Tissue ingrowth after implantation of a novel, biodegradable polyurethane scaffold for treatment of partial meniscal lesions. Am J Sports Med 39:774–782
Xu C, Zhao J (2013) A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: the more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-013-2528-6
Zaffagnini S, Giordano G, Vascellari A, Bruni D, Neri MP, Iacono F, Kon E, Presti ML, Marcacci M (2007) Arthroscopic collagen meniscus implant results at 6 to 8 years follow up. Knee Surg Sports Traumatol Arthrosc 15:175–183
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schüttler, K.F., Pöttgen, S., Getgood, A. et al. Improvement in outcomes after implantation of a novel polyurethane meniscal scaffold for the treatment of medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc 23, 1929–1935 (2015). https://doi.org/10.1007/s00167-014-2977-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-2977-6