Abstract
Purpose
The purpose of this analysis was to determine whether uncemented total knee arthroplasty performs as well as cemented total knee arthroplasty.
Methods
We searched PubMed, MEDLINE, and EMBASE, and major orthopaedic journals. This search was performed for the years from 1980 to the present. Randomised controlled trials and observational studies comparing cemented and uncemented fixation were identified. Effective data were pooled for meta-analysis. A systematic search was carried out using the EFORT website to identify the relevant arthroplasty registers.
Results
Nine studies were included in the meta-analysis. The combined odds ratio for failure of the implant due to aseptic loosening for the uncemented group over 5 and 10 years were 3.41 (p = 0.0001) and 4.73 (p = 0.0002), respectively. Subgroup analysis of data when design-related failed total knee arthroplasty (TKA)s were excluded showed no difference between the groups for odds of aseptic loosening (n.s.). There was no difference between the groups with respect to infection (n.s.). Pooled outcome of register data revealed that uncemented knees had a higher revision rate than cemented knees.
Conclusions
The important finding from the current study is that there is no evidence to support that fixation techniques alone affect the durability of a total knee arthroplasty when design-related failure in TKAs was excluded. The way of fixation is not relevant to the incidence of infection.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The durability of total knee prostheses after total knee arthroplasty (TKA) is affected by implant design, surgical technique, and patient selection [1]. Although uncemented fixation has been developed with an aim to increase the longevity of TKA implants, no clear clinical evidence has been accumulated for the benefit of uncemented TKA.
Previous meta-analysis [2] has reported a survival improvement of cemented implants compared with uncemented implants with a mean follow-up period of 2 years. It is known that aseptic loosening is one of the most common reasons for TKA failure after 5 years [3] and TKA failure after 5 years becomes common. Besides, experience has shown that non-cemented TKA is technically more demanding than cemented TKA and cemented fixation provides good initial fixation. Frequency in early failure in cementless TKA is higher compared with cemented TKA. Furthermore, national registers provide more information regarding comparative analysis of implant performance and the detection of revision rates following TKA. Bearing in mind that cementless fixation was introduced to improve the longevity of implants, we therefore conducted the meta-analysis to test the hypothesis that uncemented TKA performs as well as cemented TKA when technical failures in early stage as a bias were excluded and systematic comparative analysis using registers was employed.
Materials and methods
Search methods
In order to assemble as much relevant literature as possible, two of the authors (H.W., K.L.) independently completed comprehensive search in the most common databases of the published medical literature, including the electronic databases PubMed, MEDLINE (1980 to present), and EMBASE (from 1980 to present) using the following search terms for the initial literature search: total knee arthroplasty, knee prosthesis, cemented fixation, cementless fixation, hybrid fixation, cemented prosthesis, cementless prosthesis, hybrid prosthesis, hydroxyapatite. No language restriction was applied. The reviewers have screened the titles and abstracts of the identified studies. Furthermore, manual searching was carried out for 7 major orthopaedic journals published in from 1990 to 2012, which included Journal of Bone and Joint Surgery (American and British), Clinical Orthopaedics and Related Research, Acta Orthopaedica, the Knee, Knee Surgery Sports Traumatology Arthroscopy, and the Journal of Arthroplasty. The EFFORT Website for European Arthroplasty Registers was used to identify the existing registers [4]. In addition, we have performed a hand search using terms “(arthroplasty register) OR (knee arthroplasty register)” via Google.
Selection criteria
We confined this review to examination of fully cemented and uncemented TKA, consisting of adult patients undergoing primary TKA with a mean of 5-year follow-up or longer. Accepted study designs included randomized controlled trials, prospective and retrospective non-randomized controlled trials, and uncontrolled case series. Multiple publications of the same patient group were pooled together to avoid double-counting.
The primary outcome of this meta-analysis was survival of the implant free of aseptic loosening at over 5 and 10 years to determine whether uncemented TKA can improve the durability. The secondary outcome was a comparison of the two groups to determine whether the fixation method can affect the probability of deep infection.
Quality assessment
Each randomized control trial (RCT) was independently assessed by two of the authors (H.W. and K.L.) to grade the quality of study design using a 21-point study-quality-assessment Detsky score [5] which contained the following domains: eligibility criteria, adequacy of randomization, description of therapies, assessment of outcomes, and statistical analysis. Retrospective studies were graded on the 11-point study-quality-assessment Detsky score [5], which contained the following domains: eligibility criteria, comparison of demographic data between groups, description of a sample size calculation, outcome measures, assessment of outcomes, and statistical analysis.
Data extraction
Data were collected and extracted by one (H.W.) of us for each of the eligible meta-analyses and were re-checked for accuracy by another (K.L.), including first author, publication year, study type, the number of cases, demographic data, relevant outcomes data, follow-up, components, and survival rate. Any differences in opinion were resolved by discussion and consensus. The standard error or 95 % confidence intervals (CIs) were converted into the standard deviation.
In order to pin down factors that other than prosthetic design associated high-failure rate in early generation uncemented TKA systems, a subgroup meta-analysis was performed to investigate whether there is a difference between overall pooled reports with and without design-related failure in TKA systems.
Statistical analysis
Odds ratio for dichotomous outcome measures was employed for effect evaluation using the Mantel–Haenszel method [6]. The assessment of heterogeneity was performed. p value test and I 2 statistic were used to determine the appropriateness for meta-analysis. p < 0.1 was considered significant for homogeneity test [7]. If the results were heterogeneous (p < 0.1), a random-effects model was used. The impact of statistical heterogeneity was determined using the I 2 statistical test. A value of <25 % is considered to reflect low heterogeneity, whilst 50 % reflects moderate heterogeneity, and 75 % reflects high heterogeneity [7]. A funnel plot was used to identify publication bias. A kappa statistic was calculated to determine the level of agreement between reviewers. We chose a priori criterion of kappa = 0.6 or greater for adequate agreement [8].
The revision rates were analysed for each arthroplasty register in duplicate using a qualitative content analysis of the text and compared against one another.
Review Manager (RevMan) (version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011) was used for statistical analysis.
Results
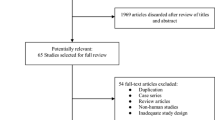
Of the 1,235 identified citations, 2,886 knees in total from 10 trials [9–18] were eligible for data extraction and meta-analysis. A same group of patients was reported by two studies [9, 15] for the two follow-ups. The latest follow-up [9] was excluded because of more clinical heterogeneity, leaving 9 studies (1,017 knees underwent cemented TKA, whilst 1,368 knees received uncemented TKA). All studies were published in English. Patient characteristics and study demographic information were noted (Table 1). The raw Detsky score for the included trials ranged from 7 to 18 points (Table 2). In the studies included in this meta-analysis, a variety of implants was used. Two [13, 18] studies have used the PCA knee system (Howmedica, Rutherford, NJ) for both the cemented and the uncemented groups. The tibial design of this system has achieved fixation with short pegs which was, however, inadequate to obtain sufficient mechanical stability to facilitate osseointegration, but instead promoted liftoff and subsidence and is known to have a high-failure rate (19 %) [19]. One [11] study has used the Kinemax prosthesis (Howmedica (UK), London, England). This system is a press-fit implant with smooth surfaces for insertion with or without cement which has been shown to increase bone density under the tibial component influence, and the rate of loosening of the uncemented tibial components is very high (20 %) [20]. Therefore, three studies [11, 13, 18] were excluded to conduct the subgroup analysis.
Durability
There was a significant difference in the survival of the implants over 5 years and 10 years follow-up (in favour of the cemented component) (p = 0.0001 and 0.0002, respectively) (Figs. 1, 4). Funnel plot indicated that the bias was minimal (Fig. 2). The survival of the implant when design-related failed TKAs have been excluded was reported in six studies, and the pooled OR was 2.2 (n.s.) (Fig. 3).
In addition to aseptic loosening of the tibial and/or femoral components, several studies [14–16] have reported on other complications. In the cemented group, common complications have included the need for subsequent patellar re-surfacing (1.1–1.2 %) [15, 16] and failure of the patellar component (39.1 %) [14]. In the non-cemented group, several patients required subsequent patellar re-surfacing (1.8–3.4 %) [15, 16] and developed failure of the patellar components (35.8 %) [14].
Infection
There was no difference between the groups with respect to infection (n.s.) (Fig. 5).
Register data
After initial identification of 28 national or regional arthroplasty registers, 3 registers (England and Wales, Sweden, New Zealand, Australia) offered sufficient data and were included in the final analysis [21–23]. The fixation method varied strongly between the registers, i.e. 90 % of totally cemented TKAs in England and Wales and New Zealand versus 54 % cemented fixation in Australia. Revision rates after cemented and uncemented TKA varied from 0.5 to 0.9 % as illustrated in Table 3. Pooled register data have revealed that uncemented knees had a higher revision rate compared with cemented knees [21–23]. However, the England and Wales Joint Replacement Registry has reported that the uncemented version performed similar to cemented version for the Scorpio and PFC brands, but not for the AGC brands [22].
Discussion
The most important finding from this meta-analysis was that uncemented TKA performs equally well with cemented TKA when design-related failure in TKAs was excluded. This is not in keeping with Gandhi’s conclusion [2]. In Gandhi’s study, the primary endpoint was survival of the implant that was free from aseptic loosening at a follow-up of 2 years, which contained the bias caused by the technical failures in early stage. Furthermore, Gandhi et al. did not conduct a subgroup analysis to exclude design-related failed TKAs. Therefore, we believe that our result is more reliable.
All of the investigated registers found that cemented prostheses offered better survival than uncemented ones, which is not consist with our finding when design-related failure in TKAs was exclude. Several causes might contribute to the discrepancy. Whilst the number of uncemented cases in the England and Wales and New Zealand registers is too small to perform meaningful comparisons, equally well performance in uncemented version versus cemented version for the Scorpio and PFC brands but not for the AGC brands [22] was reported in the England and Wales Joint Replacement Registry. The interesting aspect of the annul report is that the brand of implants relates to the survival rate. When we combined the data from just the six studies, the survivals were equivocal.
The similar incidence of infections after TKA of uncemented and cemented groups has suggested that the way of fixation is of no relevance to the occurrence of infection. An additional theoretical advantage for using uncemented fixation in TKA is the decrease in length of surgical procedure and therefore can help to minimise post-operative infection [24]. Jämsen et al. [25] pointed out that the initial boost of antibiotics release is sufficient to prevent the formation of bacterial biofilm on the implanted prosthesis and hence to prevent a post-operative infection. Prosthetic fixation with antibiotic-impregnated cement seems to be of value in total knee arthroplasty. However, none of the included studies has mentioned whether antibiotic-impregnated cement has been used. Nevertheless, it remains certain that asepsis, hygiene interventions, and antibiotic prophylaxis performed pre-, peri- as well as post-operatively are critical steps to achieve an optimal post-operative result.
The limitations of this analysis include the fact that only three studies were randomized in this meta-analysis, whilst most of the selected studies were retrospective in nature. This could have led to an effect of known and unknown confounding variables. Furthermore, surgical techniques have varied among the studies [26]. It has not been possible to conduct a subgroup analysis to account for the difference in surgical techniques, including alignment, posterior cruciate ligament management, patellar management, and ligament balancing, which are all surgeon-specific factors and may vary among individuals and centres. Since the current study included a majority of older-generation implants, it did not reflect the substantial improvements that might be observed in the currently available, newer uncemented implant with developed biomaterials. Despite the limitations inherent in this analysis, it is important to note that the studies evaluated here represent the best available in the literature, so far.
Several authors have shown that the mean age of patients undergoing TKA is decreasing and the proportion of the patients that younger than 65 years is increasing [27]. Since younger patients are more active and their life expectancy is longer, revision surgery is a likely consequence. The benefits of uncemented fixation include ease of revision, preservation of bone stock, and eliminating the requirement for cement. Our analysis therefore may be of particularly importance to the increasing number of younger patients electing for TKA.
Conclusion
The important finding from the current study is that there is no evidence to support that fixation techniques alone affect the durability of a total knee arthroplasty when design-related failure in TKAs was excluded. The way of fixation is not relevant to the incidence of infection. There is an urgent need for more higher quality studies that include newer-generation prostheses in this field to clarify which method of fixation may be of preferable for enhancing clinical outcomes.
References
Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS (2003) Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am 85:259–265
Gandhi R, Tsvetkov D, Davey JR, Mahomed NN (2009) Survival and clinical function of cemented and uncemented prostheses in total knee replacement: a meta-analysis. J Bone Joint Surg Br 91:889–895
Mulhall KJ, Ghomrawi HM, Scully S, Callaghan JJ, Saleh KJ (2006) Current etiologies and modes of failure in total knee arthroplasty revision. Clin Orthop Relat Res 446:45–50
European Arthroplasty Register (2011) EAR European arthroplasty register. http://www.ear.efort.org
Detsky AS, Naylor CD, O’Rourke K, McGeer AJ, L’Abbe KA (1992) Incorporating variations in the quality of individual randomized trials into meta-analysis. J Clin Epidemiol 45:255–265
Deeks MJ, Altman DG, Bradburn MJ (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman DG (eds). Systematic reviews in health care: meta-analysis in context. 2nd ed. London: BMJ:285-312
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2001) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Sackett DL, Haynes RB, Guyatt GH, Tugwell P (2001) Clinical epidemiology: a basic science for clinical medicine, 2nd edn. Little Brown, Boston, pp 30–31
Baker PN, Khaw FM, Kirk LM, Esler CN, Gregg PJ (2007) A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg Br 89:1608–1614
Bassett RW (1998) Results of 1,000 performance knees: cementless versus cemented fixation. J Arthroplast 13:409–413
Cloke DJ, Khatri M, Pinder IM, McCaskie AW, Lingard EA (2008) 284 press-fit Kinemax total knee arthroplasties followed for 10 years: poor survival of uncemented prostheses. Acta Orthop 79:28–33
Delaunay C, Blatter G, Canciani JP et al (2010) European “Natural Knee Group (TM)”. Survival analysis of an asymmetric primary total knee replacement: a European multicenter prospective study. Orthop Traumatol Surg Res 96:769–776
Dodd CA, Hungerford DS, Krackow KA (1990) Total knee arthroplasty fixation. Comparison of the early results of paired cemented versus uncemented porous coated anatomic knee prostheses. Clin Orthop Relat Res 260:66–70
Duffy GP, Berry DJ, Rand JA (1998) Cement versus cementless fixation in total knee arthroplasty. Clin Orthop Relat Res 356:66–72
Khaw FM, Kirk LM, Morris RW, Gregg PJ (2002) A randomised, controlled trial of cemented versus cementless press-fit condylar total knee replacement: ten-year survival analysis. J Bone Joint Surg Br 84:658–666
McCaskie AW, Deehan DJ, Green TP et al (1998) Randomised, prospective study comparing cemented and cementless total knee replacement: results of press-fit condylar total knee replacement at five years. J Bone Joint Surg Br 80:971–975
Park JW, Kim YH (2011) Simultaneous cemented and cementless total knee replacement in the same patients: a prospective comparison of long-term outcomes using an identical design of NexGen prosthesis. J Bone Joint Surg Br 93:1479–1486
Pećina M, Djapić T, Haspl M (2000) Survival of cementless and cemented porous-coated anatomic knee replacements: retrospective cohort study. Croat Med J 41:168–172
Moran CG, Pinder IM, Lees TA, Midwinter MJ (1991) Survivorship analysis of the uncemented porous-coated anatomic knee replacement. J Bone Joint Surg Am 73:848–857
Nafei A, Nielsen S, Kristensen O, Hvid I (1992) The press-fit Kinemax knee arthroplasty. High failure rate of non-cemented implants. J Bone Joint Surg Br 74:243–246
Australian Orthopaedic Association National Joint Replacement Registry (2012) Annual Report. Available from https://aoanjrr.dmac.adelaide.edu.au/home
National Joint Registry (NJR) for England and Wales (2012) Annual Report. Available from http://www-new.njrcentre.org.uk/njrcentre/Default.aspx
New Zealand Joint Registry (2012) Annual Report. Available from http://www.cdhb.govt.nz/NJR/
Peersman G, Laskin R, Davis J, Peterson M (2001) Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res 392:15–23
Jämsen E, Huhtala H, Puolakka T (2009) Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J Bone Joint Surg Am 91:38–47
Keeney JA, Eunice S, Pashos G, Wright RW, Clohisy JC (2011) What is the evidence for total knee arthroplasty in young patients? A systematic review of the literature. Clin Orthop Relat Res 469:574–583
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ (2009) Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res 467(10):2606–2612
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, H., Lou, H., Zhang, H. et al. Similar survival between uncemented and cemented fixation prostheses in total knee arthroplasty: a meta-analysis and systematic comparative analysis using registers. Knee Surg Sports Traumatol Arthrosc 22, 3191–3197 (2014). https://doi.org/10.1007/s00167-013-2806-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2806-3