Abstract
Purpose
Spontaneous subchondral osteonecrosis of the knee joint confined to a localized area of one condyle can occur after arthroscopic procedures. Meniscal tears, arthroscopic meniscectomy, and radiofrequency chondroplasty are aetiological factors in the development of osteonecrosis. The aim of this study was to investigate whether the incidence of osteonecrosis increased when mechanical or radiofrequency chondroplasty was used in conjunction with arthroscopic meniscectomy.
Methods
In this prospective clinical trial, arthroscopic meniscectomy was the primary treatment in 75 patients (mean age 40 ± 13) with stage II and III degenerative changes on the articular cartilage. Patients had to meet the following criteria: 1) have preoperative MRI and plain film radiographs showing no evidence of osteonecrosis; 2) be symptomatic for at least 6 weeks before the preoperative MRI; and 3) have arthroscopically confirmed stage II or III chondral lesion. A preoperative MRI was performed for all patients. For treatment of chondral lesions, debridement with a shaver or chondroplasty with a monopolar RF energy system was used. Patients were divided into three treatment groups. Partial meniscectomy of the medial or lateral (or both) menisci was performed on all patients, but patients in group 2 additionally received mechanical debridement of the chondral lesion, and those in group 3 were additionally treated with RF chondroplasty. Patients in group 1 were treated with partial meniscectomy alone. Patients were re-examined after 6 months, at which time a repeat MRI was performed.
Results
Development of osteonecrosis was detected during the postoperative MRIs of five patients: two in group 1, two in group 2, and one in group 3.
Conclusion
The addition of mechanical or RF chondroplasty to meniscectomy did not increase the number of patients with osteonecrosis. Also, RF chondroplasty, which is commonly proposed to be an aetiological factor, resulted in a decrease in the number of patients that developed osteonecrosis.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous osteonecrosis of the knee joint is a disease characterized by ischaemic necrosis of bone marrow and the trabecular cortex of the subchondral bone [8]. Osteonecrosis of the knee joint has been reported to occur after arthroscopic procedures [1, 6, 7, 16, 20, 21, 23]. It has been suggested that several arthroscopic interventions can result in the development of osteonecrosis, including meniscectomy and radiofrequency (RF) chondroplasty [2, 4, 5, 7, 12, 15]. Although these and other causes have been proposed, the exact aetiology of osteonecrosis is not certain.
Arthroscopic meniscectomy has long been considered to be a causative intervention in the development of osteonecrosis [1, 4, 7]. However, many studies have more recently focused on the possible effects of radiofrequency chondroplasty. It has been suggested that the thermal heating effect of radiofrequency is a causative factor in the development of osteonecrosis [10, 12, 13]. Also, the presence of meniscal tears, which alter the load distribution in the knee, has been associated with osteonecrosis [4]. Whether the meniscectomy procedure alone results in osteonecrosis or whether the addition of mechanical and radiofrequency chondroplasty contributes to the condition is still unknown.
The aim of this study was to investigate whether there was an increased incidence of osteonecrosis when a mechanical or radiofrequency chondroplasty was performed in addition to arthroscopic meniscectomy. It was hypothesized that neither mechanical nor radiofrequency chondroplasty would increase the incidence of osteonecrosis of the knee joint more than arthroscopic meniscectomy.
Materials and methods
In this prospective clinical study, arthroscopic meniscectomy was the main treatment modality. Meniscectomy was carried out on 75 patients: 41 females and 34 males, with a mean age of 40 ± 13 years. All patients had a preoperative diagnosis of a meniscal tear and underwent arthroscopic meniscectomy. During arthroscopic intervention, patients who had a single stage II or III lesion on their femoral condylar (according to the Outerbridge classification) received further chondroplasty debridement, either mechanically with a shaver or through radiofrequency ablation [18].
Patient enrolment criteria were as follows: (1) a preoperative MRI showing a meniscal tear; (2) clinical examination findings consistent with a meniscal tear; (3) no evidence of osteonecrosis on preoperative MRI; (4) symptoms lasting for at least 6 weeks before the preoperative MRI; and (5) an arthroscopically confirmed meniscal tear and an Outerbridge stage II or III femoral chondral lesion. Patients with findings of osteonecrosis on preoperative MRI, abnormal lower extremity mechanical axis, ligamentous instability, osteochondritis dissecans, rheumatoid arthritis, metabolic diseases, and those with a history of steroid use and alcohol abuse were excluded from the study.
Qualifying patients were consecutively enrolled into three treatment groups until the each group contained 25 subjects. Patients in the three treatment groups received the following interventions: group 1—only arthroscopic meniscectomy; group 2—arthroscopic meniscectomy plus mechanical debridement with a shaver; and group 3—arthroscopic meniscectomy plus radiofrequency ablation.
In group 2, the chondral fibrillations and loosened cartilage were debrided with a shaver used in oscillating mode at a speed of 2,400 rpm. In group 3, chondral lesions were debrided and sealed with the monopolar RF energy system (Lightwave Suction Ablator-2000 S, Conmed, FL, USA) with a side effect probe. Based on the recommendation by the manufacturer, the power of the monopolar equipment was set at the 75 W soft tissue ablation mode. The system was used in non-contact mode and in the paintbrush manner.
Patients were re-examined after 6 months, and MRIs (using 1.5 T scanners, PHILIPS, Intera) were performed to assess the presence of postoperative osteonecrosis. The criteria for the diagnosis of osteonecrosis on an MRI included a discrete area of low-intensity signal on the femoral condyle in the T1-weighted images, a low-signal intensity area in the centre of the lesion, plus a high-intensity signal around the margins in the T2-weighted images, presumably due to oedema [8, 9, 14, 19]. Using the method of Lotke, the size of the osteonecrotic lesion was measured on the T1-weighted images as the area of low-signal intensity (referred to as a percentage of the diameter of the medial femoral condyle) [12].
This study was approved by the Kırıkkale University Medical Faculty Committee of Research Ethics.
Statistical analysis
Power analysis and sample size calculations were computed before this study was initiated. A total sample size of 75 subjects with 25 in each treatment group achieve a power of at least 0.80 based on an assumption of 2 % incidence of postarthroscopy meniscectomy reported in previous studies [3, 5].
A Kruskal–Wallis (nonparametric one-way analysis of variance) test was applied to assess the interaction between treatment modality and development of osteonecrosis. If an effect was noted, Mann–Whitney tests were performed to assess the differences between the three treatment groups. P values lower than 0.05 were used to determine significance. All tests were performed using the statistical evaluation software package SPSS, version 17 (SPSS Inc., Chicago, IL).
Results
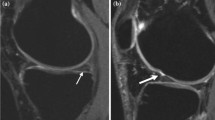
Seventy-five patients were treated arthroscopically in this study. The primary end-point of this study was the visualization of an area suggestive of osteonecrosis on postoperative MRI that was not evident on preoperative MRI. Postoperative osteonecrosis was detected in two patients in group 1, two patients in group 2, and only one patient in group 3 (Fig. 1). The mean size of the osteonecrosis (as visualized on the MRI), with regard to the whole femoral condyle, was measured as 25 % for group 1 and 30 % for groups 2 and 3. No statistically significant differences were found between groups in regard to the development of osteonecrosis.
Postoperative magnetic resonance images of a 49-year-old woman operated for an complex tear of the posterior horn of the medial meniscus. a T1-weighted magnetic resonance image depicts the subchondral lesion demonstrating a low-signal intensity area at the medial femoral condyle. b T2-weighted magnetic resonance image depicts the same lesion above with a low-signal intensity in the centre surrounded with a high-signal intensity area. The surrounding high-signal intensity area is actually the bone marrow oedema surrounding the necrotic subchondral tissue
The intra-articular characteristics of the affected patients are reported in Table 1. Patients who developed osteonecrosis had either a complex or a horizontal meniscal tear. None of the patients with radial and longitudinal meniscal tears developed osteonecrosis. Only one patient had osteonecrosis at a site other than the chondral lesion, and this patient had increasing pain at the time of the first MRI. The other four patients were satisfied with the treatment of their diseases. They had no worsening pain after the operation and experienced no activity-related pain within 8 months of the procedure.
Discussion
The most important finding of this study is that the addition of either mechanical or radiofrequency chondroplasty to arthroscopic meniscectomy did not increase the incidence of subchondral osteonecrosis. Postmeniscectomy osteonecrosis develops independently from the surgical procedure applied.
Since the suggestion was made of a relationship between meniscal tears and osteonecrosis [17], the problem continues to be unsolved. Previous case reports of osteonecrosis related this pathology with meniscal tears [11, 17] and with meniscectomy [1, 7, 9, 15, 20, 23]; thereafter, research focused on the causative effect of laser and RF chondroplasty and meniscectomy [4, 6, 21]. More recently, clinical reports have determined that RF chondroplasty is not a causative factor [3, 5].
To date, studies have not clarified the aetiology of osteonecrosis that develops after arthroscopic surgery. Although still unproven, it has been hypothesized that osteonecrosis in the presence of meniscal tears is due to the altered load distribution in the knee joint [4]. This alteration results in increased tibiofemoral contact pressure, leading to micro-fracturing and fissuring of the chondral tissue, which results in subchondral intraosseous leakage of synovial fluid [21]. There is an increased incidence of meniscal tears in the presence of osteonecrosis [8, 11, 14, 17], but it is not clear whether the incidence of osteonecrosis increases when there are meniscal tears. As there is no increased incidence of osteonecrosis in any of the treatment groups in this study, and also no proof of any correlation between meniscal tears, meniscectomy, chondroplasty, and osteonecrosis, we can speculate that osteonecrosis is the end result of the same mechanism initiated by various factors in all patients [5].
Of the patients who developed osteonecrosis, four had complex meniscal tears and one had a horizontal meniscal tear. Both types of tears occur as a result of repetitive trauma and degenerative changes. They occupy a larger portion of the meniscus and commonly necessitate wider meniscal resections. Complex and horizontal meniscal tears and their treatment alter the load distribution more than radial and longitudinal tears. This further suggests that altered load distribution may be the underlying causative factor.
Barber and Iwasko [3], in their randomized, controlled trial, compared patients treated with mechanical and monopolar RF chondroplasty. Of the 60 patients treated for grade III femoral chondral lesions, no cases of osteonecrosis were seen during a postoperative MRI at 12 months. The only abnormality was subchondral oedema in four patients (two in each treatment group). Meniscal tears were detected in 41 of their patients; 38 were treated by meniscectomy; and three were treated by repair.
The findings of the present study contradict those of the work by Barber et al. with respect to the timing of the postoperative MRI. The timing of the postoperative MRI may be the reason why they have not observed osteonecrosis in their series. It is possible that subchondral bone changes could have occurred during the early postoperative period and subsided between 6 and 12 months. If so, it is probable that subchondral osteonecrosis occurs after arthroscopic knee procedures and heals without intervention, leaving only bone marrow oedema at 12 months.
The heat effect on the fluid medium and the direct transfer of energy to subchondral bone were previously thought to be the explanatory mechanism of RF treatment causing osteonecrosis [2, 4, 5, 10, 12, 13, 15]. Our results do not support this claim and instead suggest that stopping or decreasing the use of RF is not warranted. RF chondroplasty can be used for shrinking, smoothing of the joint surface, sealing, and debridement by controlled application of heat for the treatment of grade II and III chondromalacia [22]. RF provides advantages over mechanical chondroplasty, as it results in smoother surface architecture, limited injury to adjacent untreated cartilage tissue, and easier avoidance of iatrogenic damage. In addition, defective cartilage can be more rapidly and easily countered, which results in shortened operative time [10, 13]. Compared to mechanical shaving, debridement with RF results in less chondrocyte death [24], and patients report fewer clinical symptoms at the postoperative period [25].
There is one limitation to this study. A monopolar RF probe was used for treatment; treatment results with a bipolar RF probe may be different. However, we consider that the use of a monopolar RF probe is in accordance with our aim as it delivers more energy to the subchondral bone [22].
The aetiology of postarthroscopy osteonecrosis is probably multifactorial. The addition of mechanical debridement and RF chondroplasty to arthroscopic partial meniscectomy did not increase the number of patients who developed osteonecrosis. The results of this study demonstrated that the presence of a meniscal tear and performing an arthroscopic meniscectomy may have more impact than above two factors on the development of postoperative osteonecrosis.
Conclusion
Postarthroscopy osteonecrosis is probably an end result of several impending factors. The addition of two of these factors, mechanical and RF chondroplasty, to arthroscopic meniscectomy did not increase the number of patients who developed postoperative osteonecrosis. Further in vivo studies must be planned to understand the aetiology, pathology, and natural course of osteonecrosis.
References
Al-Kaar M, Garcia J, Fritschy D, Bonvin JC (1997) Aseptic osteonecrosis of the femoral condyle after meniscectomy by the arthroscopic approach. J Radiol 78:283–288
Balcarek P, Walde TA, Sturmer KM, Kuhn A, Weigel A, Ferlemann KG, Frosch KH (2010) Impact of monopolar radiofrequency energy on subchondral bone viability. Knee Surg Sports Traumatol Arthrosc 18:673–680
Barber FA, Iwasko NG (2006) Treatment of grade III femoral chondral lesions: mechanical chondroplasty versus monopolar radiofrequency probe. Arthroscopy 22:1312–1317
Bonutti PM, Seyler TM, Delanois RE, McMahon M, McCarthy JC, Mont MA (2006) Osteonecrosis of the knee after laser or radiofrequency-assisted arthroscopy: treatment with minimally invasive knee arthroplasty. J Bone Jt Surg 88A:69–75
Çetik Ö, Çift H, Cömert B, Çırpar M (2009) Risk of osteonecrosis of the femoral condyle after arthroscopic chondroplasty using radiofrequency: a prospective clinical series. Knee Surg Sports Traumatol Arthrosc 17:24–29
Encalada I, Richmond JC (2004) Osteonecrosis after arthroscopic meniscectomy using radiofrequency. Arthroscopy 20:632–636
Faletti CMD, Robba T, De Petro P (2002) Postmeniscectomy osteonecrosis. Arthroscopy 18:91–94
Hofmann S, Kramer J, Vakil-Adli A, Aigner N, Breitenseher M (2004) Painful bone marrow edema of the knee: differential diagnosis and therapeutic concepts. Orthop Clin North Am 35:321–333
Johnson TC, Evans JA, Gilley JA, DeLee JC (2000) Osteonecrosis of the knee after arthroscopic surgery for meniscal tears and chondral lesions. Arthroscopy 16:254–261
Kosy JD, Schranz PJ, Toms AD, Eyres KS, Mandalia VI (2011) The use of radiofrequency energy for arthroscopic chondroplasty in the knee. Arthroscopy 27:695–703
Lotke PA, Ecker ML (1988) Osteonecrosis of the knee. J Bone Jt Surg 70A:470–473
Lotto ML, Wright EJ, Appleby D, Zelicof SB, Lemos MJ, Lubowitz JH (2008) Ex vivo comparison of mechanical versus thermal chondroplasty: assessment of tissue effect at the surgical endpoint. Arthroscopy 24:410–415
Lu Y, Edwards RB 3rd, Nho S, Cole BJ, Markel MD (2002) Lavage solution temperature influences depth of chondrocyte death and surface contouring during thermal chondroplasty with temperature-controlled monopolar radiofrequency energy. Am J Sports Med 30:667–673
Marti CB, Rodriguez M, Zanetti M, Romero J (2000) Spontaneous osteonecrosis of the medial compartment of the knee: a MRI follow-up after conservative and operative treatment, preliminary results. Knee Surg Sports Traumatol Arthrosc 8:83–88
Muscolo DL, Costa-Paz M, Makino A, Ayerza MA (1996) Osteonecrosis of the knee following arthroscopic meniscectomy in patients over 50-years old. Arthroscopy 12:273–279
Nakamura N, Horibe S, Nakamura S, Mitsuoka T (2002) Subchondral microfracture of the knee without osteonecrosis after arthroscopic medial meniscectomy. Arthroscopy 18:538–541
Norman A, Baker N (1978) Spontaneous osteonecrosis of the knee and medial meniscal tears. Radiology 129:653–656
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Jt Surg 43B:752–757
Pape D, Seil R, Kohn D, Schneider G (2004) Imaging of early stages of osteonecrosis of the knee. Orthop Clin North Am 35:293–303
Prues-Latour V, Bonvin J, Fritschy D (1998) Nine cases of osteonecrosis in elderly patients following arthroscopic meniscectomy. Knee Surg Sports Traumatol Arthrosc 6:142–147
Rozbruch SR, Wickiewicz TL, DiCarlo EF, Potter HG (1996) Osteonecrosis of the knee following arthroscopic laser meniscectomy. Arthroscopy 12:245–250
Shellock FG (2001) Radiofrequency energy induced heating of bovine articular cartilage: comparison between temperature controlled, monopolar, and bipolar system. Knee Surg Sports Traumatol Arthrosc 9:392–397
Spahn G, Klinger HM, Mückley T, Hofmann GO (2010) Four-year results from a randomized controlled study of knee chondroplasty with concomitant medial meniscectomy: mechanical debridement versus radiofrequency chondroplasty. Arthroscopy 26(9 Suppl):S73–S80
Turner AS, Tippett JW, Powers BE, Dewell RD, Mallinckrodt CH (1998) Radiofrequency (electrosurgical) ablation of articular cartilage: a study in sheep. Arthroscopy 14:585–591
Uribe JW, Markarian G, Kaplan L, Sasken H (1998) Use of coblation in articular cartilage surgery. Res Outcomes Arthrosc Surg 3:1–4
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Türker, M., Çetik, Ö., Çırpar, M. et al. Postarthroscopy osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc 23, 246–250 (2015). https://doi.org/10.1007/s00167-013-2450-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2450-y