Abstract
Purpose
It was reported that not only ACL but also the synovium may be the major regulator of matrix metalloproteinases (MMPs) in synovial fluids after ACL injury. In order to further confirm whether synovium is capable of regulating the microenvironment in the process of ACL injury, the complicated microenvironment of joint cavity after ACL injury was mimicked and the combined effects of mechanical injury and inflammatory factor [tumour necrosis factor-α (TNF-α)] on expressions of lysyl oxidases (LOXs) and MMPs in synovial fibroblasts derived from normal human synovium were studied.
Methods
Human normal knee joint synovial fibroblasts were stimulated for 1–6 h with mechanical stretch and inflammatory factor (TNF-α). Total RNA was harvested, reverse transcribed and assessed by real-time polymerase chain reaction for the expression of LOXs and MMP-1, 2, 3 messenger RNAs. MMP-2 activity was assayed from the collected culture media samples using zymography.
Results
Compared to control group, our results showed that 6 % physiological stretch increased MMP-2 and LOXs (except LOXL-3), decreased MMP-1 and MMP-3; injurious stretch (12 %) decreased LOXs (except LOXL-2)and increased MMP-1, 2 and 3; the combination of injurious stretch and TNF-α decreased LOXs and increased MMP-1, 2 and 3 in synovial fibroblasts in a synergistical manner.
Conclusion
This study demonstrated that combination of mechanical injury and inflammatory factors up-regulated the expressions of MMPs and down-regulated the expressions of LOXs in synovial fibroblasts, eventually alter the balance of tissue healing. Thus, synovium may be involved in regulating the microenvironment of joint cavity. Based on the mechanism, early interventions to inhibit the production of MMPs or promote the production of LOXs in the synovial fibroblasts should be performed to facilitate the healing of tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because of increasing sport activities, injury to the anterior cruciate ligament (ACL) and medial collateral ligament (MCL) has risen during the last years. Healing after injury is structure specific. It is known that after a complete rupture, the MCL has a relatively good healing capacity. In contrast, the adult ACL fails to heal after complete rupture [3]. Injuries to the ACL predispose the knee to further degradation that can lead to joint instability, which in turn can result in secondary osteoarthritis (OA) [23]. Consequently, reconstructive surgery is the preferred choice of treatment. Unfortunately, revision surgery of reconstructed ACL is frequently reported because the operative techniques still do not satisfactorily stabilize the ligament [12].
Apart from several experimental factors including location, blood supply and nutrition, previous studies have shown that several intrinsic properties such as adhesion, proliferation, migration and collagen synthesis also may be important contributing factors to the dissimilar healing potential of ACL and MCL cells [26, 33, 42]. The different characteristic mentioned above between ACL and MCL may explain why the posterior cruciate ligament (PCL) also has a poor healing ability. During early remodelling phase of ligament, old ECM molecules are gradually degraded by proteolytic enzyme and new ECM molecules undergo aggregation and cross-linking to form fibres [7]. This protein degradation and synthesis in the ligaments is an intricately modulated process. Regulation of this process will greatly affect the healing ability of ligaments.
Matrix metalloproteinases (MMPs) are a group of collagen cleaving enzymes that participated in matrix formation, remodelling and homeostasis. Numerous researchers demonstrated that the MMPs are involved in the unbalanced matrix degradation process that initiates cartilage degeneration in OA and rheumatoid arthritis (RA) [29]. Lysyl oxidases (LOXs), a copper-dependent amine oxidase, play an important role in the ECM synthesis, by catalysing lysine-derived cross-links formation of the collagen and elastin [19]. The presence of 0.1 Schiff-base cross-links per collagen molecule results in twofold to threefold resistance to human collagenase when compared with non-cross-linked controls or samples [38].
Previous study reported that poor healing ability of ACL was associated with MMPs secreted by inflammation cells such as neutrophil and macrophages which migrated rapidly into the ACL stumps after injury [6]. With an equi-biaxial stretch chamber which could mimic the loading forces applied to the ACL, previous in vitro studies reported that the higher level and activity of MMP-2 seen in mechanically injured ACL fibroblasts than MCL fibroblasts may disrupt the delicate balance of ECM remodelling process, which may could be an important reason responsible for their differential healing ability [22, 48]. Another in vivo model study also proved that injured ACL releases large amounts of MMP-2 into synovial fluids [36]. Irie et al. [17] found increased amount of TNF-α, IL-1β and IL-6 in the joint fluid during the acute inflammation phase after ACL injury. These cytokines are also considered important chemical mediators in the acute inflammatory phase of wound healing. With the same stretch chamber, Wang et al. [40] revealed that ACL fibroblasts are very sensitive to mechanical factor and inflammation cytokine in terms of releasing of MMP-2. Based on the results, Xie et al. [45] found that combination of injured stretch and IL-1β induced lower expressions of LOXs and higher expressions of other MMPs in ACL fibroblasts than MCL fibroblasts with the same stretch chamber. The data further suggest that the imbalance of ECM regulated by LOXs and MMPs in ACL fibroblasts might be another intrinsic property of ACL for its poor healing ability.
It is reported that synovial fibroblasts are mechanosensitive [1]. With the equi-biaxial stretch chamber, a previous in vitro study by Wang et al. [41] revealed that the increase of MMP-2 expression and activity in synovial fibroblasts induced by mechanical injury and inflammation cytokines and suggested that synovial fibroblasts play an important role in the regulating microenvironment of joint cavity in the process of ACL injury.
In order to further determine whether synovial fibroblasts are capable of regulating microenvironment of joint cavity, or whether poor healing ability of ACL is associated with the imbalance of MMPs and LOXs produced by synovial fibroblasts during remodelling process, we used an equi-biaxial stretch chamber to study the expressions of MMPs and LOXs in synovial fibroblasts under mechanical stretch and inflammatory factors. The findings would provide help for looking for therapeutic targets to improve ACL healing. Our hypothesis in this study was that combination of injurious stretch and TNF-α may synergistically increased the gene expressions of MMPs and decreased gene expressions of LOXs from human knee joint synovial fibroblasts.
Materials and methods
Cell culture
Human synovial fibroblasts were harvested from four donor tissues (age range 30–60, two male and two female subjects) undergoing limb amputation at First Affiliated Hospital of Chongqing Medical University, Chongqing, China. Patient consent was obtained prior to the surgery. All procedures were followed according to ethical principles and protocols as approved by Chongqing University and Chongqing Medical University. None of the patients had any underlying diseases. The donor ligament tissue was obtained from patients after surgery. The standard operating procedure of synovial fibroblasts culturing has been described by previous study [21].
Cytokine treatment
For each experiment, cells were trypsinized and seeded at a density of 5 × 105 cells per 25 cm2 flasks (Corning, USA). Cells were allowed 48 h to seed and equilibrate. The culture media was removed and replaced by 2 % foetal bovine serum (FBS) media for 16 h for starvation. The media was removed and replaced with fresh 1 % FBS media containing recombinant human TNF-α (1, 5, 10 and 20 ng/ml) (PeproTech, NJ) and incubated for 3 h. Reported concentrations of TNF-α in synovial fluid range from 40 to 250 pg/ml in RA patients. Based on the data, we choose 5 ng/ml TNF-α for time-course experiments, and this concentration was used throughout the current study [28].
Mechanical injury
With equi-biaxial stretch chamber (Country Machines and Plastics, San Diego, CA, USA) [22], we study the effects of mechanical stretch on synovial fibroblasts. The operating procedure has been described by previous study [41, 48].
Quantitative real-time polymerase chain reaction (qRT-PCR)
Quantitative real-time polymerase chain reaction was used to compare the levels of steady-state mRNA for several genes in conditioned and control cultures of human knee synovial fibroblasts. The BLAST was used to search for all the primer sequences to ensure gene specificity. Selected sets of primers are shown in Table 1. This operating procedure has been described by previous study [45].
Zymography
MMP-2 activity was assayed from the collected culture media samples using 0.05 % gelatin zymography as described previously [41].
Statistical analysis
Data are expressed as mean ± SD. Statistical analysis was performed by one-way analysis of variance (ANOVA). Post hoc analysis utilized Fisher LSD. In each analysis, critical significance level was set at p < 0.05. The average thermal cycles (Ct) value of genes in synovial fibroblasts induced by mechanical stretch and TNF-α is presented in appendix of the supplementary material.
Results
Effects of physiological stretch on the expression of mRNA for LOX family and MMP family in normal human knee synovial fibroblasts
The expressions of the LOXs except LOXL-3 in synovial fibroblasts were up-regulated after 1–6 h of 6 % physiological stretch compared to the control. Levels of LOX, LOXL-1 and LOXL-4 mRNA reached a maximum at 3 h (2.14-, 1.36- and 2.23-fold, respectively). LOXL-2 mRNA level increases in a time-dependent manner and increases 3.5-fold at 6 h (Fig. 1). However, the expression levels of MMP-1, 2 and 3 in synovial fibroblasts were down-regulated after a 6 h 6 % physiological loading compared to the 0 % control (Fig. 2).
Effects of physiological and injurious stretch on the expressions of mRNA for LOX family in normal human knee synovial fibroblasts. a The LOX expression. b The LOXL-1 expression. c The LOXL-2 expression. d The LOXL-3 expression. e The LOXL-4 expression. Data (mean ± SD, n = 3) were represented as the fold change in expression compared to control. Statistic analysis was done by ANOVA. *Significant difference with respect to control (p < 0.05)
Effects of physiological and injurious stretch on the expressions of mRNA for MMP family in normal human knee synovial fibroblasts. a The MMP-1 expression. b The MMP-2 expression. c The MMP-3 expression. Data (mean ± SD, n = 3) were represented as the fold change in expression compared to control. Statistic analysis was done by ANOVA. *Significant difference with respect to control (p < 0.05)
Effects of TNF-α on the expression of mRNA for LOX family and MMP family in normal human knee synovial fibroblasts
To examine TNF-α responsiveness of synovial fibroblasts, these cells were treated with 0–20 ng/ml of human TNF-α and RNA analysed by real-time PCR (Fig. 3). Addition of TNF-α (0–20 ng/ml) led to a decreasing of LOXs expressions. The inhibitory effect of LOX and LOXL-3 by TNF-α was concentration-dependent. The inhibitory effect reached a maximum (0.67-fold) at 5 ng/ml TNF-α for LOXL-1. The expressions of LOXL-2 and LOXL-4 reached a maximum (1.21- and 0.94-fold, respectively) at 5 ng/ml TNF-α and subsequently declined below the control values in response to increasing TNF-α concentration (Fig. 3a).
Effects of TNF-α with different concentrations (0–20 ng/ml) on the expressions of mRNA for LOX family and MMP family in normal human knee synovial fibroblasts. a The LOX family expressions. b The MMP family expressions. Data (mean ± SD, n = 3) were represented as the fold change in expression compared to control. Statistic analysis was done by ANOVA. *Significant difference with respect to control (p < 0.05)
TNF-α at all concentrations (from 1 to 20 ng/ml) significantly increased MMP-1, 2 and 3 expressions. The stimulation effect reached a maximum (3.83- and 2.19-fold, respectively) at 5 ng/ml TNF-α for MMP-1 and 2. For MMP-3, there was a concentration-dependent increase with increasing TNF-α concentration to a maximum (13.8-fold) (Fig. 3b). An effective dose of 5 ng/ml was chosen for further experiments.
Treatment of synovial fibroblasts with 5 ng/ml TNF-α significantly inhibited the expression of LOXs; this inhibitory effect decreased to a minimum (1.14- and 1.18-fold, 0.77- and 0.9-fold, respectively) after 3 h for LOX, LOXL-2, LOXL-3 and LOXL-4, but only after 2 h for LOXL-1 (0.87-fold) compared with control values (Fig. 4a). Addition of 5 ng/ml TNF-α, however, increased the expressions of MMP-1, 2 and 3 (Fig. 4b). This stimulating effect was significant after 1 h, reaching maximal levels of 4.44- and 2.73-fold increases at 2 h for MMP-1 and 2, maximizing at 8.57-fold after 3 h for MMP-3, and then slowly decreasing. These results collectively indicate that TNF-α suppressed the expressions of LOXs but stimulates the expressions of MMPs at the transcriptional level.
Effects of 5 ng/ml TNF-α on the expressions of mRNA for LOX family and MMP family in normal human knee synovial fibroblasts. a The LOX family expressions. b The MMP family expressions. Data (mean ± SD, n = 3) were represented as the fold change in expression compared to control. Statistic analysis was done by ANOVA. *Significant difference with respect to control (p < 0.05)
Effects of injurious stretch and TNF-α on the expression of mRNA for LOX family and MMP family and MMP-2 activity in normal human knee synovial fibroblasts
Injurious stretch alone induced a decrease of LOXs mRNA except LOXL-2 in synovial fibroblasts compared to the control. Level of LOX and LOXL-3 mRNA peaked at 2 h (increase 3.03- and 1.88-fold, respectively), all others at 3 h (increase 2.31-fold in LOXL-1; increase 7.75-fold in LOXL-2; increase 3.54-fold in LOXL-4), then progressively decreased to a lower level than the control group except for LOXL-2 (Fig. 1). However, in the presence of TNF-α, the 12 % injurious stretch-induced up-regulation of LOXs at 1, 2 and 3 h was significantly inhibited and decreased further below control after 6 h (Fig. 5).
Effects of injurious stretch and TNF-α on the expressions of mRNA for LOX family in normal human knee synovial fibroblasts. a The LOX expression. b The LOXL-1 expression. c The LOXL-2 expression. d The LOXL-3 expression. e The LOXL-4 expression. Data (mean ± SD, n = 3) were represented as the fold change in expression compared to control. Statistic analysis was done by ANOVA. *Significant difference with respect to control (p < 0.05)
Levels of MMP-1, 2 and 3 mRNA increased significantly after 12 % injurious stretch alone (Fig. 2). Level of MMP-1 and 3 mRNA peaked at 3 h (increase 3.15- and 4.21-fold, respectively) and MMP-2 at 2 h (increase 3.48-fold). In the presence of TNF-α, injurious stretch had an enhanced effect on inducing MMP-1, 2 and 3 expressions. Levels of MMP-1 and 2 mRNA reached a maximum at 2 h (increase 5.37- and 4.65-fold, respectively) and MMP-3 at 3 h (increase 10.67-fold) (Fig. 6).
Effects of injurious stretch and TNF-α on the expressions of mRNA for MMP family in normal human knee synovial fibroblasts. a The MMP-1 expression. b The MMP-2 expression. c The MMP-3 expression. Data (mean ± SD, n = 3) were represented as the fold change in expression compared to control. Statistic analysis was done by ANOVA. * Significant difference with respect to control (p < 0.05)
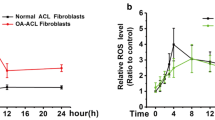
Gelatin zymography showed that the synovial fibroblasts increased the MMP-2 expression and showed a noticeable stepwise, time-dependent conversion of 72–62 kD MMP-2 from 12 to 48 h in 12 % stretch group and stretch + TNF-α group compared to the control. In addition, the stretch + TNF-α group significantly enhanced MMP-2 activity relative to mechanical injury or TNF-α alone (Fig. 7).
Effects of injurious stretch and TNF-α on MMP-2 activity in normal human knee synovial fibroblasts. a Zymographic analysis of the conditioned media collected from cells treated without (control) and with injurious stretch (12 %) and TNF-α (5 ng/ml) for different times 12, 24, 48 and 72 h. The gels shown are representative of three different experiments. b Quantification of MMP-2 activities showed time-dependent increases of MMP-2 activities in both 12 % stretch group and stretch + TNF-α group. Quantification was done with Quantity One 4.6.3 software. Besides, the band 62 kDa active form MMP-2 was calculated as 10 times density of the 72 kDa pro-MMP-2 band as described previously. The data were mean of three different experiments (mean ± SD, n = 3)
Discussion
The most important finding of the present study was that injurious stretch and TNF-α decreased LOXs and increased MMP-1, 2 and 3 in synovial fibroblasts in a synergistical manner.
The equi-biaxial stretch chamber has been used in our laboratory for numerous years, enabling the application of two-dimensional mechanical strains at 5–15 %, to synovial fibroblasts [39, 41]. This stretch apparatus also has been used widely by other laboratories for many years and many results have been published using this system [15, 16, 21]. Biomechanical studies that quantify strains in ACL and MCL have shown that these ligaments are subjected to 4–5 % stretch during normal activities and can be strained to 7.7 % during external application of loads to the knee joint [48]. Therefore, the 6 % level was used to model normal physiologic strain in this in vitro model. The 0 % strain served as the control baseline group. Based on previous reports, we considered pathologic strains (traumatic rupture) to approach 12–19 % [11, 48]. Therefore, the 12 % level was used to model pathologic strain in this in vitro model. In this system, the seeded synovial fibroblasts will attach to the membrane, proliferate and release ECM components into the surrounding environment in which the cells interact either with other cells or with other ECM components. It hence mimics the stretching forces applied to the synovial tissue in the knee joint.
The increase of LOXs expressions (except LOXL-3) by 6 % physiological stretch may be a part of the synovial fibroblasts physiological adaptation process. This adaptation allows the synovium to improve the mechanical strength and withstand the mechanical loads imposed on it during normal activities of daily living. The observed inhibitory effects of physiological stimuli on MMPs in normal synovial fibroblasts are consistent with other in vitro studies in various types of connective tissues and cells such as MCL, tendon, menisci, chondrocytes and RA synovial fibroblasts [2, 34, 47]. The consistency proved that moderate exercise may be beneficial to maintain connective tissues homeostasis and treat arthritis.
Contrary to LOXs, the expression levels of MMP-1, 2 and 3 in human normal synovial fibroblasts were down-regulated after 6 % physiological loading compared to the 0 % control. However, a previous study by Wang et al. [39] demonstrated that the expression level of MMP-3 was unchanged in synovial fibroblasts from RA patients after 6 % physiological loading. The discrepancy was attributed to phenotypical alterations in RA synovial fibroblasts. In RA synovial fibroblasts, these changes might include morphology, signalling pathways and apoptosis [27]. In addition, the study by Breshears et al. [4] demonstrated no change in MMP-3 expression after 4 % physiological loading, but these cells were harvested from canine cranial cruciate ligaments (CCL). In addition, Breshears et al. used uniaxial cyclic loading, while we used static equi-biaxial loading. It is also possible that the 4 % loading is no more a sufficient stimulus for regulating the MMP-3 expression in CCL cells.
The observation of up-regulation of MMP-1, 2 and 3 in synovial fibroblasts after 12 % stretch is not consistent with a previous study by Spindler et al. [32] which described the lack of expressions of MMP-1 and 2 with an in situ hybridization technique in a ruptured ACL. A possible explanation for this confliction is the difference in the sensitivity of the techniques and cell type used in these two studies.
Inflammation is the initial response to any tissue injury. Previous studies showed that TNF-α could inhibit ACL healing through various ways, including inhibition of ACL fibroblast migration [43], suppression of type I collagen synthesis [13], stimulation of ACL fibroblast apoptosis [25] and promotion of MMP-2 expression and activities in ACL fibroblast and synovial fibroblasts [40, 45]. This study revealed that TNF-α not only increased the expressions of MMP-1, 2 and 3 but also decreased the expressions of LOXs in synovial fibroblasts. These results revealed that synovial fibroblasts are very sensitive to inflammatory cytokines in regulating the expressions of MMPs and LOXs; the pro-inflammatory factors were involved in the healing process of knee joint tissues. Multiple studies have described the promotion of TNF-α to expressions of MMPs in other tissues and cells, which contributes to the development of inflammatory disease such as chronic wounds, RA and asthma. The most successful approaches so far in the treatment of inflammatory diseases are anti-TNF-α strategies. The signal transduction pathways activated when TNF-α binds to their cognate receptors on cells are potential drug targets. Based on the mechanism, the three currently biological anti-TNF-α drugs, etanercept, infliximab and adalimumab, have been clearly shown to have high clinical efficacy [5, 9, 31].
In the real physiological situation, the stretching force may exert its effect together with other factors to induce the injurious cascade. We report here that combination of injurious stretch and TNF-α synergistically increased the expression of MMP-1, 2 and 3 which are secreted into the knee joint cavity from synovial fibroblasts compared to the control. The increase of MMP-1, 2 and 3 expressions and activity could activate other members of the family. For example, MMP-1 can activate latent MMP-2, MMP-2 can activate latent MMP-13 and MMP-3 can activate MMP-1, 9 and 13 [20]. Thus, the ability of MMPs to activate each other creates a complex network of proteases in the synovial fluids. Moreover, as the knee joint cavity is a relatively isolated fluid-containing space surrounded by synovial membrane, which facilitates the accumulation of MMPs in synovial fluids. The high levels of MMPs in synovial fibroblasts induced by injurious stretch and TNF-α may provide an explanation of poor self-healing ability of ACL.
However, the stretch stimulations and TNF-α caused a significant reduction in the mRNA levels for LOXs compared to the stretch groups. This inhibition decreased LOXs concentrations in synovial fluids and therefore results in decreased degree of cross-linking, which weaken the mechanical properties of ECM and thereby increased the degradation susceptibility of ECM by MMPs, thus destroyed the balance between the degradative and biosynthetic arms of ACL tissue remodelling process. This result may provide another explanation concerning the poor healing ability of ACL. Based on these results, we postulate that synovial fibroblasts are sensitive to mechanical injury and inflammatory factors and play an important role in regulating the production of MMPs and LOXs in joint fluids in the real physiological situation and must be considered seriously.
Limitations of this study must be considered when interpreting the results. First, we only examined mRNA expression. The LOXs and MMPs are tightly regulated after expression, requiring additional activation and may be inhibited by other proteins. Examination of protein levels and enzyme activity should be conducted to confirm the findings in this study. Second, we present only a correlation between the increase of a proteinase (MMPs) in synovial fibroblasts and poor healing ability of ACL. In connective tissues, such as ligament, the degradation of ECM involves participation of a variety of other proteinases including cysteine proteinases, serine proteinases and aspartic proteinases [30]. Besides MMPs, cysteine proteinases (such as cathepsins) have also gained attention for their ability to degrade collagen. For example, cathepsin K has been found in RA synovial fibroblasts, suggesting a role for the enzyme in RA [14]. Tartrate-resistant acid phosphatase (TRAP), although not a cysteine protease (but is associated with many cysteine proteases), has also the ability to degrade type I collagen and was found in canine ligamentous tissue [24]. Based on the results, we postulated these proteinases also participate in the ACL healing as important mediators. Third, we did not examine the expression of tissue inhibitors of metalloproteinases (TIMPs). This family consists of four protease inhibitors, which function to block MMP activity at a 1:1 molar ratio by forming a complex with the activated catalytic zinc in the MMPs [48]. A previous study by Tchetverikov showed that patients with ACL injury have a persistent increase in pro-MMP-1 and 3 in synovial fluid and an increase in activated MMPs, coincided with a significant decrease in TIMP-1 [37]. In addition, a previous study by Ishiguro and Amiel et al. showed that the total catabolic effects of MMPs in ruptured human and rabbit ACL might be superior to the inhibition of TIMPs. Anderson et al. reported that an increase in MMPs activity relative to TIMP activity was found at sites of cartilage destruction when compared with normal cartilage [18]. The same situation may apply in ruptured synovium in humans. Fourth, the model system in this study utilizes monolayer culture with injurious stretching, and TNF-α only partially mimicked the real forces and cytokines applied to synovium after ACL injury, and not fully represents the in vivo situation. Inside the knee joint fluid surrounding the injured ACL, MMPs and LOXs may come from other sources other than synovium and ACL. For instance, they may also come from PCL fibroblast, chondrocyte or meniscal cells. It is well known that in the knee joint fluids the levels of TNF-α, IL-1β and TGF-β are all elevated [17]. These factors may further modulate the levels of MMPs and LOXs from other sources. In addition, the microenvironment of the wound is devoid of oxygen shortly after tissue injury because of the vascular disruption and the high oxygen consumption caused by high immune cell density and cell activity in granulation tissue [35]. Previous study has indicated that hypoxia increased the MMP-2 release as well as its conversion to active form and suggested that it is another major component that contributes to the microenvironment [40]. It is possible that the hypoxia, as a microenvironment factor, may also affect the levels of other MMPs and LOXs in synovial fibroblasts.
This study is significant in that we provided evidence suggesting a possible therapeutic strategy for suppressing MMPs production and promoting LOXs production in synovial fibroblasts after ACL injury. Researches indicated that the AP-1, JNK and NF-kB pathways can significantly affect MMPs expression [44, 46]. This may help develop the MMP inhibitors to block the MMP production in joint fluids after knee injury. Besides, a number of MMPs molecule inhibitors (MMPi) have been designed including cipemastat, rebimastat, doxycycline, ilomastat, tetracyclines and bisphosphonates [10]. Previous studies have shown that transforming growth factor-β (TGF-β) could promote cell proliferation, as well as synthesis of small proteoglycan and collagen [8]. On the basis of these studies, we speculated that TGF-β may be a good candidate for stimulating LOXs expression in synovial fibroblasts. This work will be performed in the future.
Conclusion
In summary, the present in vitro study demonstrated that synovial fibroblasts are sensitive to mechanical injury and inflammatory factors, and may be involved in regulating the microenvironment of joint cavity. The results showed that the mechanical injury and inflammatory factors collectively decreased LOXs expressions and increased MMP-1, 2 and 3 expressions in synovial fibroblasts, which are always injured accompanied by the injury of ACL. The differential effects of microenvironmental factors on LOXs and MMPs expressions in injured synovial fibroblasts would lead to the accumulation of MMPs in the synovial fluids, eventually alter the balance of tissue healing. Thus, early interventions to inhibit the production of MMPs or promote the production of LOXs in the synovial fibroblasts should be performed to facilitate the healing of ACL.
References
Anitua E, Sanchez M, De la Fuente M et al (2012) Plasma rich in growth factors (PRGF-Endoret) stimulates tendon and synovial fibroblasts migration and improves the biological properties of hyaluronic acid. Knee Surg Sports Traumatol Arthrosc 20:1657–1665
Asundi KR, Rempel DM (2008) Cyclic loading inhibits expression of MMP-3 but not MMP-1 in an in vitro rabbit flexor tendon model. Clin Biomech 23:117–121
Bray RC, Leonard CA, Salo PT (2002) Vascular physiology and long-term healing of partial ligament tears. J Orthop Res 20:984–989
Breshears LA, Cook JL, Stoker AM et al (2010) The effect of uniaxial cyclic tensile load on gene expression in canine cranial cruciate ligamentocytes. Vet Surg 39:433–443
Catrina AI, Lampa J, Ernestam S et al (2002) TNF-α as a promising therapeutic target in chronic asthma: a lesson from rheumatoid arthritis. Rheumatology 41:484–489
Chamberlain CS, Brounts SH, Sterken DG et al (2011) Gene profiling of the rat medial collateral ligament during early healing using microarray analysis. J Appl Physiol 111:552–565
Chithra P, Sajithlal GB, Chandrakasan G (1998) Influence of Aloe vera on collagen characteristics in healing dermal wounds in rats. Mol Cell Biochem 181:71–76
DesRosiers EA, Yahia L, Rivard CH (1996) Proliferative and matrix synthesis response of canine anterior cruciate ligament fibroblasts submitted to combined growth factors. J Orthop Res 14:200–208
Di Sabatino A, Pender SL, Jackson CL et al (2007) Functional modulation of Crohn’s disease myofibroblasts by anti-tumor necrosis factor antibodies. Gastroenterology 133:137–149
Fisher JF, Mobashery S (2006) Recent advances in MMP inhibitor design. Cancer Metastasis Rev 25:115–136
Fleming BC, Beynnon BD (2004) In vivo measurement of ligament/tendon strains and forces: a review. Ann Biomed Eng 32:318–328
Fu FH, Bennett CH, Lattermann C et al (2000) Current trends in anterior cruciate ligament reconstruction. Am J Sports Med 28:124–130
Greenwel P, Tanaka S, Penkov D et al (2000) Tumor necrosis factor alpha inhibits type I collagen synthesis through repressive CCAAT/enhancer-binding proteins. Mol Cell Biol 20:912–918
Hou WS, Li Z, Gordon RE et al (2001) Cathepsin K is a critical protease in synovial fibroblast-mediated collagen degradation. Am J Pathol 159:2167–2177
Hsieh AH, Sah RL, Sung KL (2002) Biomechanical regulation of type I collagen gene expression in ACLs in organ culture. J Orthop Res 20:325–331
Hsieh AH, Tsai CMH, Ma QJ et al (2000) Time-dependent increase in type-III collagen gene expression in medial collateral ligament fibroblasts under cyclic strains. J Bone Joint Surg 18:220–227
Irie K, Uchiyama E, Iwaso H (2003) Intraarticular inflammatory cytokines in acute anterior cruciate ligament injured knee. Knee 10:93–96
Ishiguro N, Shimizu T, Ito T et al (2000) The expression of matrix metalloproteinases and inhibitors in acute rupture of the anterior cruciate ligament. Mod Rheumatol 10:95–102
Kagan HM, Li W (2003) Lysyl oxidase: properties, specificity, and biological roles inside and outside of the cell. J Cell Biochem 88:660–672
Kerrigan JJ, Mansell JP, Sandy JR (2000) Matrix turnover. J Orthod 27:227–233
Lee AA, Delhaas T, McCulloch AD et al (1999) Differential responses of adult rat cardiac fibroblasts to in vitro biaxial strain patterns. J Mol Cell Cardiol 31:1833–1843
Lee AA, Delhaas T, Waldman LK et al (1996) An equibiaxial strain system for cultured cells. Am J Physiol 271:C1400–C1408
Lohmander LS, Englund PM, Dahl LL, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries. Am J Sports Med 35:1756–1769
Muir P, Danova NA, Argyle DJ et al (2005) Collagenolytic protease expression in cranial cruciate ligament and stifle synovial fluid in dogs with cranial cruciate ligament rupture. Vet Surg 34:482–490
Murakami H, Shinomiya N, Kikuchi T et al (2006) Upregulated expression of inducible nitric oxide synthase plays a key role in early apoptosis after anterior cruciate ligament injury. J Orthop Res 24:1521–1534
Nagineni CN, Amiel D, Green MH et al (1992) Characterization of the intrinsic properties of the anterior cruciate and medial collateral ligament cells: an in vitro cell culture study. J Orthop Res 10:465–475
Pap T, Müller-Ladner U, Gay RE et al (2000) Fibroblast biology. Role of synovial fibroblasts in the pathogenesis of rheumatoid arthritis. Arthritis Res 2:361–367
Patwari P, Cook MN, DiMicco MA et al (2003) Proteoglycan degradation after injurious compression of bovine and human articular cartilage in vitro: interaction with exogenous cytokines. Arthritis Rheum 48:1292–1301
Poole AR (1997) Cartilage in health and disease. In: Koopman WJ (ed) Arthritis and allied conditions, 13th edn. Williams and Wilkins, Baltimore
Powers JC, Asgian JL, Ekici OD et al (2002) Irreversible Inhibitors of Serine, Cysteine, and Threonine Proteases. Chem Rev 102:4639–4750
Russo C, Polosa R (2005) Anti-tumor necrosis factor (TNF)-α therapy (etanercept) down-regulates serum matrix metalloproteinase (MMP)-3 and MMP-1 in rheumatoid arthritis. Clin Sci 109:135–142
Spindler KP, Clark SW, Nanney LB et al (1996) Expression of collagen and matrix metalloproteinases in ruptured human anterior cruciate ligament: an in situ hybridization study. J Orthop Res 14:857–861
Sung KL, Yang L, Whittemore DE et al (1996) The differential adhesion forces of anterior cruciate ligament and medial collateral ligament fibroblasts: effects of tropomodulin, talin, vinculin, and alpha-actinin. Proc Natl Acad Sci USA 93:9182–9187
Sun HB, Yokota H (2001) Messenger-RNA expression of matrix metalloproteinases, tissue inhibitors of metalloproteinases, and transcription factors in rheumatic synovial cells under mechanical stimuli. Bone 28:303–309
Tandara AA, Mustoe TA (2004) Oxygen in wound healing—more than a nutrient. World J Surg 28:294–300
Tang Z, Yang L, Wang Y et al (2009) Contributions of different intraarticular tissues to the acute phase elevation of synovial fluid MMP-2 following rat ACL rupture. J Orthop Res 27:243–248
Tchetverikov I, Lohmander LS, Verzijl N et al (2005) MMP protein and activity levels in synovial fluid from patients with joint injury, inflammatory arthritis, and osteoarthritis. Ann Rheum Dis 64:694–698
Vater CA, Harris ED Jr, Siegel RC (1979) Native cross-links in collagen fibrils induce resistance to human synovial collagenase. Biochem J 181:639–645
Wang P, Yang L, You X et al (2009) Mechanical stretch regulates the expression of matrix metalloproteinases in rheumatoid arthritis fibroblast-like synoviocytes. Connect Tissue Res 50:98–109
Wang Y, Tang Z, Xue R et al (2011) Combined effects of TNF-α, IL-1β, and HIF-1α on MMP-2 production in ACL fibroblasts under mechanical stretch: an in vitro study. J Orthop Res 29:1008–1014
Wang Y, Yang L, Zhang J et al (2009) Differential MMP-2 activity induced by mechanical compression and inflammatory factors in human synoviocytes. Mol Cell Biomech 7:105–114
Wiig ME, Amiel D, Ivarsson M et al (1991) Type I procollagen gene expression in normal and early healing of the medial collateral and anterior cruciate ligaments in rabbits: an in situ hybridization study. J Orthop Res 9:374–382
Witkowski J, Yang L, Wood DJ et al (1997) Migration and healing of ligament cells under inflammatory conditions. J Orthop Res 15:269–277
Xie J, Jiang J, Zhang Y et al (2012) Up-regulation expressions of lysyl oxidase family in ACL and MCL fibroblasts induced by TGF-β1. Int Orthop 36:207–213
Xie J, Wang C, Yin L et al (2012) IL-1β influences on lysyl oxidases and matrix metalloproteinases profile of injured anterior cruciate ligament and medial collateral ligament fibroblasts. Int Orthop. PMID: 22588690
Yan C, Boyd DD (2007) Regulation of matrix metalloproteinase gene expression. J Cell Physiol 211:19–26
Yokota H, Goldring MB, Sun HB (2003) CITED2-mediated regulation of MMP-1 and MMP-13 in human chondrocytes under flow shear. J Biol Chem 278:47275
Zhou D, Lee HS, Villarreal F et al (2005) Differential MMP-2 activity of ligament cells under mechanical stretch injury: an in vitro study on human ACL and MCL fibroblasts. J Orthop Res 23:949–957
Acknowledgments
This study was supported by the Innovation and Attracting Talents Program for College and University (“111” Project) (B06023), NSF Projects (10672195, 30870607), CSTC2008BB5192, Sharing fund of Chongqing university’s large-scale equipment (2009063038) and by NIH AR45635 (USA).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Y., Huang, W., Jiang, J. et al. Influence of TNF-α and biomechanical stress on matrix metalloproteinases and lysyl oxidases expressions in human knee synovial fibroblasts. Knee Surg Sports Traumatol Arthrosc 22, 1997–2006 (2014). https://doi.org/10.1007/s00167-013-2425-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2425-z