Abstract
Purpose
The purpose of this study was to report the survival analysis of partial lateral facetectomy and Insall’s procedure in patients with isolated patellofemoral osteoarthritis, and to assess the risk and protective factors for failure of this procedure.
Methods
From 1992 to 2004, all subjects with isolated patellofemoral osteoarthritis who met the inclusion criteria and underwent this procedure were enrolled. Risk and protective factors for failure (failure considered as the need for total knee arthroplasty) were assessed by comparing obtained baseline data between failed and non-failed cases. Eighty-seven cases (mean (SD) age 61.8 (7.7) years, mean (SD) follow-up 9.6 (3.2) years) were included.
Results
Twenty-three failed cases were found. Mean (SD) survival time was 13.6 (0.5) years. At 13 years (last failure case), the cumulative survival was 59.3 %. Baseline medial tibiofemoral pain, genu flexum, and worst grade of tibiofemoral osteoarthritis were significant risk factors for failure (p < 0.0001, p = 0.02, p < 0.0001, respectively). In contrast, higher anatomical (p = 0.02) and total (p = 0.03) knee society score (KSS) scores, absence of knee effusion (p = 0.03), higher value of the Caton–Deschamps index (p = 0.03), and lateral position of the patella (p = 0.01) were all protective factors against failure.
Conclusion
The treatment for isolated patellofemoral osteoarthritis through partial lateral facetectomy and Insall’s procedure demonstrated good long-term survival. The presence of preoperative medial tibiofemoral pain, genu flexum, and incipient tibiofemoral osteoarthritis increased the risk of failure of this procedure. In contrast, higher anatomical and total KSS scores, absence of knee effusion, higher value of the Caton–Deschamps index, and lateral position of the patella were found to protect against failure.
Level of evidence
Prospective case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Isolated patellofemoral osteoarthritis (IPFOA) is a common disorder of multifactorial aetiology but in many cases related to an impairment of the extensor mechanism evidenced by the presence of trochlear dysplasia [2, 4], or disorders of the patellar tilt and shift [4, 7, 10]. When conservative treatment fails, surgical options may be considered taking into account the cause of IPFOA [25]. The isolated advancement (Maquet’s procedure) [20] or the advancement and medialization (Fulkerson’s osteotomy) [6] of the anterior tibial tubercle are distal procedures that have been employed expecting to decrease the load on the patellofemoral joint. Autologous chondrocyte implantation has been used in patellar and/or trochlear chondral defects in young patients, but not in old subjects with joint space narrowing [23, 29]. Patellofemoral arthroplasty may elicit good outcomes, especially when no tibiofemoral osteoarthritis is present and extensor mechanism disorders are corrected [15, 18, 28]. Total knee arthroplasty (TKA) may only be adequate as the first surgical option in old patients with at the most an incipient tibiofemoral osteoarthritis [17, 24]. Nonetheless, TKA for IPFOA is considered to sacrifice too much of healthy tissue and is thus believed to be a too aggressive procedure for disorders affecting only one compartment [25]. Total patellectomy is not a first option to treat IPFOA because it causes significant impairment in kinetics and kinematics of the knee joint and is mainly reserved to other conditions (fractures, infections, tumours) [25]. In addition, patellar removal may worsen the outcomes of subsequent knee replacement surgery [11].
Soft tissue procedures over the extensor mechanism have been mostly employed for patellofemoral instability but not osteoarthritis. Although the lateral retinaculum release (Ficat’s procedure) was initially described for the treatment of lateral hypertension syndrome of the patella [5], it has been mainly used for patellar pain syndrome and instability [5, 25]. The vastus medialis advancement to the middle free edge of the patella (West and Soto-Hall’s procedure) [31], the proximal “tube” realignment (Insall’s procedure) [8], and the reconstruction of the patellofemoral ligament have been mostly employed for patellofemoral instability due to malalignment of the extensor mechanism but not for IPFOA. Lateral facetectomy was initially proposed to treat IPFOA by Martens and De Rycke [21]. Some authors have employed this technique alone [27, 32, 33] or in combination with medialization of the tibial tubercle [1]. To the best of our knowledge, there are no studies that have performed proximal soft-tissue realignment (Insall’s procedure) associated with partial lateral facetectomy, even though most cases of IPFOA are related to altered patellar shift and/or tilt [25].
The purpose of this study was twofold: first, to report the survival of partial lateral facetectomy and Insall’s procedure in patients with IPFOA; second, to assess the risk and protective factors for failure (defined as need for TKA) of this surgical procedure. It was hypothesized that the use of both facetectomy and proximal soft-tissue realignment would result in long survivorship.
Materials and methods
A prospective case series study was conducted to report the survival of partial lateral facetectomy and soft-tissue proximal realignment (Insall’s procedure) for the treatment of IPFOA. Failure of this technique was considered to be the need for TKA. Risk and protective factors for failure of this surgical treatment were also assessed by comparing baseline data between failed and non-failed cases. From 1992 to 2004, all consecutive patients undergoing this procedure were approached for eligibility. All subjects with IPFOA and absence of previous patellar dislocation, patellar fracture, and tibiofemoral osteoarthritis (or only grade I of the Kellgren–Lawrence classification) were enrolled in this study. All patients underwent conservative treatment for at least 6 months before surgery. All surgical procedures were performed by the same senior surgeon (FM). Patients were required to give informed consent before participating in this study, and this study has been approved by Institutional Review Board.
The history of symptoms and data on physical and radiological examination were collected in each patient during the first (baseline) visit. Knee function was assessed through specific questions (asking about pain when going upstairs and downstairs, uphill and downhill, distance able to walk with no pain, need of crutches, and range of motion) and through the Knee Society Score (KSS) [9] and Kujala score [16].
Imaging studies were carried out with radiographs and computed tomography (CT) scans. Radiographs included full-length, weight-bearing, anterior–posterior view, true lateral view, 45° knee flexion posterior–anterior weight-bearing view (Rosenberg’s view), and a 30° patellar axial view. The height of patella was measured by the Caton–Deschamps index. The Kellgren–Lawrence classification was used to assess the tibiofemoral osteoarthritis [13]. CT scans were employed to measure the sulcus angle, the tibial tubercle–trochlear groove (TT-TG) distance, the patellar tilt angle, and the patellar shift (using a Merchant’s congruence angle-like measurement) [22]. In addition, imaging studies were also used to obtain information about the type (first Dejour’s classification) [4], bump, and depth of trochlea. The Iwano radiological classification was used to evaluate the patellofemoral joint [10].
Surgical technique
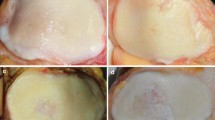
The surgical technique was standardized for all patients. All patients were placed in supine position, and leg ischaemia was employed. Centred anterior skin incision with subcutaneous dissection was conducted until the development of a medial capsule–synovial plane. Medial capsule and vastus medialis were then isolated in the same plane (Fig. 1). It is important to assure that the medial synovial membrane remains intact (avoiding medial arthrotomy). Through the same skin incision, the lateral capsule–synovial plane was also exposed (Fig. 2a). The lateral retinaculum and synovial membrane were then sectioned (lateral arthrotomy) (Fig. 2b). Horizontal dissection of lateral and anterior soft tissues was carried out, exposing the osteophyte and lateral facet of the patella (Fig. 3a). Longitudinal excision of both the lateral osteophyte and the most lateral part of the patella were performed with an oscillating saw (Fig. 3b), as described by Martens and De Rycke [21]. A lateral condyle and proximal trochlear debridement was performed, including excision of all osteophytes. The anterior aspect of the lateral capsule was sutured to the posterior aspect of the synovial membrane (closure of the lateral arthrotomy) without tightening of the lateral soft tissue structures (Fig. 4a). At this point, the ischaemia is released and a thorough haemostasis is carried out. Finally, a proximal soft-tissue realignment through the Insall’s procedure was performed (Fig. 4b) [8]. This is a critical moment because care must be taken to avoid hypercorrection of the patellar tilt and shift and assure adequate patellar tracking from 0° to 90° without suture failure. Figure 5 shows the pre- and postoperative position of the patella assessed through bone CT scan (Fig. 5).
The postoperative rehabilitation protocol began with continuous passive motion 12 h after surgery, with 2-h session twice a day starting at 30° with progression of 10° per session. Rehabilitation was aimed to achieve complete weight-bearing 2 days, 90° of knee flexion 5 days, isometric quadriceps exercises 7 days, and going upstairs or downstairs and walking without crutches 1 month after surgery.
Statistical analysis
Descriptive statistics were used to summarize the demographic, surgical, anatomical, functional, physical examination, and radiological characteristics of the sample, using frequencies and percentages to describe categorical variables and mean and standard deviation for quantitative variables. A survival analysis was conducted to determine the time to failure (need for TKA) during the follow-up of the sample. A Kaplan–Meier curve was used to represent graphically the results of the survival analysis. Univariate Cox regression analysis was used to identify the risk and protective factors for failure of the surgical procedure. Statistically significant factors in the univariate analysis were further placed in a multivariate Cox regression analysis. A stepwise procedure was then manually realized (removing or including these significant factors depending on their significance and influence on other variables) to obtain the best explicative model. P values less than 0.05 were considered statistically significant. Statistical analysis was conducted with the SPSS, v.16 (Chicago, IL, USA).
Results
A total of 87 cases of partial lateral facetectomy and Insall’s procedure for the treatment for IPFOA were included in this study. Mean (SD) age and follow-up of the sample were 61.8 years (7.7) and 9.6 years (3.2), respectively. The baseline demographic, surgical, anatomical, functional, physical examination, and radiological characteristics of the sample are summarized in Table 1.
The survival analysis is shown with the Kaplan–Meier curve (Fig. 6). A total of 23 cases of failure (need for TKA) were found. No surgical procedures other than TKA were performed after the partial lateral facetectomy plus Insall’s procedure. Mean (SD) survival time was 13.6 (0.5) years (95 % confidence interval 12.6–14.6). At 13 years (the last failure case presented), the cumulative survival was 59.3 %. Maximum follow-up was 16.6 years.
Table 2 shows both risk and protective factors for failure of this surgical procedure for both the univariate and multivariate analyses. For the univariate analysis, baseline medial tibiofemoral pain, genu flexum, and worst grade of tibiofemoral osteoarthritis were significant risk factors for failure of this procedure. In contrast, higher anatomical and total KSS scores, absence of knee effusion, higher value of the Caton–Deschamps index, and lateral position of the patella were all protective factors against failure of the reported surgical procedure. The most important risk factors for failure that remained in the final model (multivariate analysis) were medial tibiofemoral pain and the presence of tibiofemoral osteoarthritis, whereas anatomical KSS score was the most important protective factor against failure of this procedure.
Discussion
The most important finding of the present study was the good long-term survival of partial lateral facetectomy and Insall’s procedure for the treatment of IPFOA. The presence of preoperative medial tibiofemoral pain, genu flexum, and incipient tibiofemoral osteoarthritis increased the risk of failure of this procedure. In contrast, higher anatomical and total KSS scores, absence of knee effusion, higher value of the Caton–Deschamps index, and lateral position of the patella were found to protect against failure. These results have been obtained in a homogeneous sample with IPFOA with no previous patellar dislocation. To our knowledge, this is the first study reporting the treatment of IPFOA through a combination of partial lateral facetectomy and Insall’s procedure.
Total patellectomy or replacement of patellofemoral joint (either TKA or patellofemoral arthroplasty) has certain limitations. Patellectomy induces more impairment of the extensor mechanism and makes further reconstructive surgery difficult [11, 12, 14, 19, 20, 30]. Replacement procedures have been demonstrated to significantly improve pain and function [17, 24, 26]. Differing results of patellofemoral arthroplasty may be explained by failure to identify present or incipient tibiofemoral osteoarthritis or failure to correct extensor apparatus impairment [25]. In addition, it is important to take into account the economic costs of implants, time spent in surgery, and time and discomfort with the rehabilitation programme.
Some authors have employed lateral facetectomy to treat IPFOA [1, 21, 27, 32, 33]. This technique has been used in combination with lateral retinaculum release alone [21, 27, 32, 33] or in association with medialization of the tibial tubercle [1]. Martens et al. [21] performed lateral facetectomy in 20 subjects with IPFOA associated with lateral retinaculum release because of extensor mechanism malalignment. The authors reported good-to-moderate results in 90 % of subjects with a follow-up of only 2 years [21]. They found that the most important factor associated with failure was the presence of tibiofemoral osteoarthritis. The first failed case in the present sample was found at 3.5 years of follow-up. It was observed in the present investigation that tibiofemoral osteoarthritis was a significant risk factor for failure, which agrees with the findings reported by Martens et al. [21]. Yercan et al. reported the results of lateral facetectomy and lateral retinaculum release in 11 middle-aged to elderly (mean age of 62 years) patients with IPFOA at a mean follow-up of 8 years (range 3–14) [33]. The pain, KSS, and walking function significantly improved at latest follow-up [33]. The authors reported no cases of failure although the study only involved 11 subjects. As tibiofemoral and patellofemoral osteoarthritis progressed in 6 (55 %) and 4 patients (36 %), respectively, it might be possible that a longer follow-up and greater sample size would have elicited the need for revision surgery in some patients. In addition, the authors reported that 55 % of patients had trochlear dysplasia compared with 71.2 and 78 % in the present sample and in the study by Dejour and Allain [3], respectively. Yercan et al. [33] found a lateral subluxation rate of 63 % of patients, which is similar to the present investigation. They found that lateral position of the patella was only corrected in 2 of the 7 patients (28 %). This may indicate that lateral retinaculum release may not be enough to correct patellar position. Risk and protective factors for failure could not be evaluated by Yercan et al. because no patients needed revision surgery. Paulos et al. [27] also performed lateral facetectomy and lateral retinaculum release to treat 63 patients (66 knees) with stage III and IV IPFOA. The cumulative failure (need for TKA) for a mean of 60 months of follow-up was 17 %, as compared to a 3.5 % in the present investigation. Paulos et al. were not able to find differences in any of the employed questionnaires, physical examination, and radiographs between satisfied and non-satisfied (mostly those who needed revision surgery) patients. Therefore, no risk or protective factors could be reported although the authors found more tibiofemoral osteoarthritis in those subjects with need for revision surgery, which corresponded to the findings reported in the present investigation. Recently, Wetzels and Bellemans reported their results of lateral facetectomy and lateral retinaculum release in 155 consecutive patients (168 knees) followed up to 25 years (mean 10.9 years) [32]. The authors reported a percentage of failed cases (need for TKA, patellofemoral arthroplasty, or total patellectomy) of 36.9 % (26.4 % in the present study) and a cumulative survival of 85 % at 5 years, 67.2 % at 10 years, and 55 % at 15 years of follow-up [32] (96.4, 72.6, and 59.3 % in the present study, respectively). No patients from the present study were revised with patellofemoral arthroplasty because the cause of failure was the progression of tibiofemoral osteoarthritis. The average time to need TKA in the present study was similar to that reported by Wetzels and Bellemans (8 years) [32]. They found that revision surgery was higher in women compared with men. However, the survivorship was not significantly influenced by gender, weight, body mass index, height, age, or associated procedures at any stage of follow-up [32]. Surprisingly, Wetzels and Bellemans reported no information on important potential causes of failure such as progression of patellofemoral or tibiofemoral osteoarthritis. In contrast, the present study was able to establish several risk and protective factors against failure. The presence of patients with patellar dislocation was not reported by Paulos et al. [27] and Wetzels and Bellemans [32]. Becker et al. [1] carried out lateral facetectomy associated with lateral retinaculum release and medialization of the tibial tubercle for treatment of 50 patients with IPFOA. Importantly, as it was done in the present study, Becker et al. did not include patients with patellar dislocation. The authors found no failed cases after a mean of 20.2 months (range 7–32 months), and no risk or protective factors against failure could be, therefore, reported [1]. However, the authors did not recommend the addition of medialization of the tibial tubercle because results were not better, or even worst, compared to the existing literature. Disappointing outcomes by Becker et al. may be explained by the fact that the TT-TG distance was not reported by the authors. The knowledge of this measure is mandatory to avoid a wrong position of the tibial tubercle (hypercorrection of the TT-TG distance). Given that patients in the present study had normal values of TT-TG measure (mean 8.6 ± 4.6) and disorders of the patellar tilt and shift, the authors believe there was no need for distal realignment procedures but instead soft-tissue proximal realignment associated with partial lateral facetectomy.
In the present study, the IPFOA has been treated in a similar way to how the patellofemoral instability is treated because trochlear dysplasia and disorders of the patellar tilt and shift are present in most of these patients. Most of the previous treatments (total patellectomy, tibial tubercle advancement, lateral facetectomy, autologous chondrocyte implantation, patellofemoral arthroplasty, or TKA) have not considered these factors as potential causes of IPFOA. In fact, some of the series using patellofemoral arthroplasty and autologous chondrocyte implantation for the treatment of IPFOA have achieved best results when they corrected the disorders of extensor mechanism [2, 29]. Therefore, it is necessary to keep in mind the extensor mechanism anomalies for an adequate treatment of IPFOA.
This study has strengths and limitations. The principal value of this investigation is the mean survival time (need for TKA as endpoint) for this surgical procedure of 13.5 years. Although patellofemoral arthroplasty and TKA has demonstrated good results in patients with IPFOA [17, 24], lateral facetectomy and Insall’s procedure is a less aggressive surgery with no implant use that would delay the need for joint replacement for several years. Also, this technique does not make the revision surgery difficult with TKA or patellofemoral arthroplasty. The major limitation of this study is the lack of a control or comparative group. This fact prevented us to determine whether the present results may be attributed to the use of this surgical technique itself instead of the natural history of the disease. Prospective comparative level I- or II-evidence studies are needed to investigate the role of lateral facetectomy and Insall’s procedure at delaying joint replacement surgery in patients with IPFOA. A second limitation of this study is the lack of intra- and inter-observer reliability of the assessment methods. However, all measurements were conducted by a highly experienced surgeon in patellofemoral disorders.
The clinical implications of this study are twofold. First, partial lateral facetectomy associated with an Insall’s procedure can be an adequate treatment for middle-aged to elderly patients presenting with IPFOA. This technique may be less aggressive and cheaper compared to other procedures, and in addition, it is a joint-preserving technique that may leave TKA as a salvage procedure for the future. Second, the determination of risk and protective factors against failure presented in this investigation has clear clinical implications because patients not adequate for this procedure may be identified and managed in a different way.
Conclusion
The treatment of IPFOA through partial lateral facetectomy and Insall’s procedure demonstrated good long-term survival. The presence of preoperative medial tibiofemoral pain, genu flexum, and incipient tibiofemoral osteoarthritis increased the risk of failure of this procedure. In contrast, higher anatomical and total KSS scores, absence of knee effusion, higher value of the Caton–Deschamps index, and lateral position of the patella were found to protect against failure.
References
Becker R, Röpke M, Krull A, Musahl V, Nebelung W (2008) Surgical treatment of isolated patellofemoral osteoarthritis. Clin Orthop Relat Res 466:443–449
Cartier P, Sanouiller JL, Grelsamer RP (1990) Patellofemoral arthroplasty. 2–12-year follow-up. J Arthroplasty 5:49–55
Dejour D, Allain J (2004) Histoire naturelle de l’arthrose fémoro-patellaire isolée. Rev Chir Orthop 90:1S69–1S129
Dejour H, Walch G, Neyret P, Adeleine P (1990) Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 76:45–54
Ficat P, Ficat C, Bailleux A (1975) External hypertension syndrome of the patella. Its significance in the recognition of arthrosis. Rev Chir Orthop Reparatrice Appar Mot 61:39–59
Fulkerson JP, Becker GJ, Meaney JA, Miranda M, Folcik MA (1990) Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med 18:490–497
Galtier B, Buillot M, Vanneuville G (1995) Anatomical basis of the role of vastus medialis muscle in femoro-patellar degenerative arthroplasty. Surg Radiol Anat 17:7–11
Insall JN, Bullough PG, Burstein AH (1979) Proximal “tube” realignment of the patella for chondromalacia patellae. Clin Orthop Relat Res 144:63–69
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y (1990) Roentgenographic and clinical findings of patellofemoral osteoarthritis. Clin Orthop Relat Res 252:190–197
Joshi AB, Lee CM, Markovic L, Murphy JC, Hardinge K (1994) Total knee arthroplasty after patellectomy. J Bone Joint Surg Br 76:926–929
Kang JD, Papas SN, Rubash HE, McClain EJ (1993) Total knee arthroplasty in patelectomized patients. J Arthroplasty 8:489–501
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kelly MA, Insall JN (1986) Patellectomy. Orthop Clin North Am 17:289–295
Kooijman HJ, Driessen AP, van Horn JR (2003) Long-term results of patellofemoral arthroplasty. A report of 56 arthroplasties with 17 years of follow-up. J Bone Joint Surg Br 85:836–840
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Laskin RS, van Steijn M (1999) Total knee replacement for patients with patellofemoral arthritis. Clin Orthop Relat Res 367:89–95
Leadbetter WB, Ragland PS, Mont MA (2005) The appropriate use of patellofemoral arthroplasty: an analysis of reported indications, contraindications and failures. Clin Orthop Relat Res 436:91–99
Lennox DW, Hungerford DS, Krackow KA (1987) Total knee arthroplasty following patellectomy. Clin Orthop Relat Res 223:220–224
Maquet P (1963) Considerations biomechaniques sur l’arthrose de genou. Un traitement biomechanique de l’arthrose femoropatellaire: l’avancement du tendon rotulien. Rev Rhum Mal Osteoartic 30:779–783
Martens M, De Rycke J (1990) Facetectomy of the patella in patellofemoral osteoarthritis. Acta Orthop Belg 56:563–567
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56:1391–1396
Minas T, Bryant T (2005) The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res 436:30–39
Mont MA, Haas S, Mullick T, Hungerford DS (2002) Total knee arthroplasty for patellofemoral arthritis. J Bone Joint Surg Am 84:1977–1981
Montserrat F (2010) Isolated patellofemoral osteoarthritis. European Instructional Lectures 11th EFORT congress 10:163–183
Parvizi J, Stuart MJ, Pagnano MW, Hanssen AD (2001) Total knee arthroplasty in patients with isolated patellofemoral arthritis. Clin Orthop Relat Res 392:147–152
Paulos LE, O’Connor DL, Karistinos A (2008) Partial lateral patellar facetectomy for treatment of arthritis due to lateral patellar compression syndrome. Arthroscopy 24:547–553
van Jonbergen HP, Werkman DM, Barnaart LF, van Kampen A (2010) Long-term outcomes of patellofemoral arthroplasty. J Arthroplasty 25:1066–1071
Vasiliadis HS, Lindahl A, Georgoulis AD, Peterson L (2011) Malalignment and cartilage lesions in the patellofemoral joint treated with autologous chondrocyte implantation. Knee Surg Sports Traum Arthrosc 19:452–457
Watkins MP, Harris BA, Wender S, Zarins B, Rowe CR (1983) Effect of patellectomy on the function of the quadriceps and hamstrings. J Bone Joint Surg Am 65:390–395
West F, Soto-Hall R (1958) Recurrent dislocation of the patella in the adult: end results of patellectomy with quadricepsplasty. J Bone Joint Surg Am 40:386–394
Wetzels T, Bellemans J (2012) Patellofemoral osteoarthritis treated by partial lateral facetectomy: results at long-term follow-up. Knee 19:411–415
Yercan H, Selmi T, Neyret P (2005) The treatment of patellofemoral osteoarthritis with partial lateral facetectomy. Clin Orthop Relat Res 436:14–19
Acknowledgments
We thank Sergi Mojal (PhD) for the excellence of his statistical analysis and methodological advices.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Montserrat, F., Alentorn-Geli, E., León, V. et al. Partial lateral facetectomy plus Insall’s procedure for the treatment of isolated patellofemoral osteoarthritis: survival analysis. Knee Surg Sports Traumatol Arthrosc 22, 88–96 (2014). https://doi.org/10.1007/s00167-012-2286-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2286-x