Abstract
Purpose
To investigate the congruency of the articular cartilage surface of the knee between the recipient and donor site during autogenous osteochondral grafting using a three-dimensional (3D) laser scanning.
Methods
Six cadaveric knees were included in this study. The 3D profiles of the articular surface were obtained by a 3D laser scanner (FastSCAN®, Polhemus). We divided each of the donor and recipient sites into 6 areas in each. The 2 central areas of the donor site were excluded from evaluation because of the trochlear groove. In the donor site, the peripheral and the middle one-third of the femoral articular surface in the medial and lateral patellofemoral joint were extracted. In the recipient site, the peripheral and the middle one-third of the articular surface in the medial and lateral femoral condyle were assessed. In each recipient area, vertical intervals (VIs) of grafts of 6, 8, and 10 mm diameter, showing the distance between highest and lowest point of articular surface were calculated from the data obtained and to the donor sites for matching.
Results
ϕ6- and ϕ8-mm grafts The VI of the middle area of the donor site did not differ significantly from that of either the peripheral or the middle area of the recipient site. The VI of the peripheral area of the donor site was significantly higher than that of the peripheral area of the recipient site (p < 0.01). ϕ10-mm grafts The VI of the middle area of the donor site was significantly lower than that of the peripheral area of the recipient site. The VI of the peripheral area of the donor site was significantly higher than that of the middle area of the recipient site (p < 0.01).
Conclusions
An osteochondral graft harvested from the peripheral area of the patellofemoral joint might protrude into the middle area in the recipient site, whereas a ϕ10-mm osteochondral graft harvested from the middle area might be depressed from the peripheral area into the recipient site.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Focal chondral and osteochondral defects of the loading surfaces often cause problems for patients including pain, swelling, clicking and instability, and may lead to early degenerative changes [14, 26]. Cartilage defects gradually lead to the degeneration of the articular cartilage and osteoarthritis. Several investigators have been searching for an ideal method to repair the articular defects and thereby recreate or restore the normal articular cartilage surface. Common repair techniques for these lesions are microfracture [6], autogenous chondrocyte implantation (ACI) [4, 5, 10, 22] and autogenous osteochondral grafting [3, 13]. Of these techniques, autogenous osteochondral grafting has been widely cited for its advantages for hyaline or hyaline-like cartilage repair in the damaged area because this technique is usually a 1-stage procedure of direct transplantation at the mature present hyaline cartilage defect site [1, 8, 11, 12].
In this procedure, surgeons match the shape of the articular surface between the recipient and the donor site to reproduce the original articular surface of the femoral condyle [7, 16, 17, 20, 25]. Koh et al. [16] reported that peak contact pressures were significantly elevated by approximately 20 % after defect creation and were reduced to normal when plugs were flush. Large and significant increases in pressure were encountered when plugs were elevated 1 and 0.5 mm above the adjacent cartilage. Contact pressures with plugs sunk to a depth of 0.5 and 1 mm were significantly higher than the pressure in the intact cartilage but were significantly lower than the pressure in an empty defect. However, surgeons may sometimes encounter mismatching of the articular surface between the recipient and the donor while using this technique. Thus, the selection of the donor site should be based on the size and shape of the recipient site.
In autogenous osteochondral grafting, small cylindrical grafts are harvested from the non-weight-bearing periphery of the patellofemoral joint and implanted into the focal cartilage defect of the weight-bearing condylar surface [14]. However, the shape of the articular cartilage surface of the femoral condyle may be round, flat, convex or concave, and may vary between the donor and recipient site. Therefore, a mismatch between the shapes at the articular cartilage surface is possible while performing this technique. Some authors assessed graft matching of this technique [2, 27]. However, the previous studies were evaluated in a two-dimensional plane or the location of the donor sites and the recipient site regarding the margin of articular cartilage were not clearly addressed. To overcome this problem, we analysed the articular cartilage surface shape of the knee joint in more detail using this three-dimensional (3D) laser scanner and clearly classified the location of the donor and the recipient sites. Hence, we investigated the ideal donor site depending on the location of the articular cartilage lesion.
It was hypothesized that a convex osteochondral graft would match a convex recipient area and a flat graft to a flat recipient site. Therefore, the purpose of this study was to investigate matching of the articular surface between the recipient and the donor site by using the 3D laser scanning method and clarify the matching pattern that leads to an ideal transplantation at the recipient site.
Materials and methods
Specimens were obtained from cadavers donated at the Clinical Anatomical Course at the Division of Developmental Neurobiology, Department of Physiology and Cell Biology, Kobe University Graduate School of Medicine. The cause of death and medical history of the donors were deemed to have no bearing on the musculoskeletal system. The cadaveric tissue was perfusion-fixed in embalming fluid containing 10 % formaldehyde, 10 % phenol and 40 % ethanol. Six femoral condyles (3 left and 3 right) were taken from the knee joint, which appeared to be structurally normal on visual inspection. Knees with the evidence of chondromalacia, prior knee surgery, osteoarthritis or osteophytes, or damage to the articular cartilage were excluded in this study and remaining 6 knees were included in this study. The age at death was 70–84 years (average age of 75.8 years). The skin and soft tissues around the knee joint were removed from each specimen without damage to the articular cartilage surface of the femoral condyle. The proximal side of the femur was osteotomized at the mid-femur level. After the preparation, the specimens were fixed using an acrylic resin with a specially made polyvinyl chloride tube for data acquisition. Institutional Review Board approval was obtained before proceeding with this study, and our protocol was approved by the ethical committee of our institution.
Data acquisition
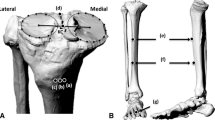
A 3D laser scanner (Fast SCAN Cobra®, Polhemus, VT, USA) was used to obtain a 3D profile of the knee [9, 21, 23]. The configuration of this device is shown in Fig. 1. The device consists of a receiver with laser scanner, transmitter and signal-processing unit. A broad-ranging beam, generated from the laser indicator, was distorted by the target object, and the surface profile of the object was captured by a camera with manual handling of the receiver. The transmitter produced a magnetic wave so that the receiver could calculate the position and pose of the space. The transmitter was placed on a tripod near a cadaveric specimen in a metal-free area. The effective area of the transmitter was 1,000 mm. Resolution of this device is as good as 0.1 mm and the absolute accuracy is 0.75 mm. Practical accuracy determined by scanning a bowling ball and calculating the variation in radius over the point cloud surface was 0.13 mm. The data were recorded 3 times, and the reproducibility of the measurements was checked. The test–retest reliability of these three measurements was excellent (intraclass correlation coefficient = 0.93). The median data of 3 measurements were used for analysis. Because a laser scanner regard a target object as one mesh data of the surface profile, the knee shape obtained cannot show the boundary of the articular cartilage and the cortical bone. To detect these boundaries, the margin between the articular cartilage area and the cortical bone area was demarcated using the stylus, and the articular cartilage area was identified.
Data analysis
The analysis method aims to calculate the height difference of the cylindrical graft surface. In the autogenous osteochondral grafting surgery, a cylindrical graft of diameter 6, 8 and 10 mm is often harvested. Because the surface in the axis direction is convex because of the hemisphere of the femoral condyle, the vertical interval (VI) of the convex was considered target information. The analysis method consists of the following 4 steps (Fig. 2a).
-
1.
Indicate a point in the joint surface from the mesh data obtained.
-
2.
Calculate the normal vector of the indicated point.
-
3.
Determine an analysis area of a constant diameter from the normal vector.
-
4.
Calculate the VI from the highest and lowest points along the normal vector within the analysis area (Fig. 2b).
Measurement data were 3D numerical data that represented the mesh structure of the target profile. The primitive mesh shape was triangular. The proposed method was applied to the mesh data obtained.
For the data analysis, we divided the donor and recipient sites into 2 areas (Fig. 3). In this technique, small cylindrical grafts are harvested from the non-weight-bearing periphery of the patellofemoral joint. To evaluate the donor site, we divided the patellar surface of the femur into 6 areas. The peripheral one-third (peripheral) and the middle one-third of the femoral articular surface in medial and lateral patellofemoral joint were extracted. The inside one-third areas in the medial and lateral patellofemoral joint (the trochlear groove) were excluded from this study, because these areas directly articulate patella and should not be used as a donor site in this technique. In the recipient site, the peripheral one-third and the middle one-third of the articular surface in the medial and lateral femoral condyle (weight-bearing area) were assessed. VIs were calculated in each area of the femoral condyle in the donor and recipient sites. In each area, 3 points were extracted and the mean and standard deviation values were calculated. The peripheral area and the middle area were compared around the VIs.
Statistical analysis
One-way analysis of variance (ANOVA) was used for the comparison of the VIs in each area. The Scheffé post hoc test was used to assess the data considered significant by the ANOVA.
Results
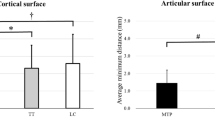
ϕ6-mm graft (Fig. 4) and ϕ8-mm graft (Fig. 5)
The VI of the middle area of the donor site did not differ significantly from that of either the peripheral or the middle area of the recipient site. However, the VI of the peripheral area of the donor site was significantly higher than that of the peripheral area of the recipient site (p < 0.01), indicating mismatch between the recipient site and donor sites.
The VIs in ϕ6-mm grafts. In the donor site, the VIs of the peripheral and the middle areas were 1.9 ± 0.5 mm and 1.3 ± 0.3 mm, respectively. In the recipient site, the VIs of the peripheral and the middle areas were 1.5 ± 0.3 mm and 1.2 ± 0.4 mm, respectively. The peripheral area of the donor site was significantly higher than the peripheral area of the recipient site (p < 0.01)
The VIs in ϕ8-mm grafts. In the donor site, the VIs of the peripheral and the middle areas were 2.6 ± 0.6 mm and 1.6 ± 0.3 mm, respectively. In the recipient site, the VIs of the peripheral and the middle areas were 2.1 ± 0.6 mm and 1.5 ± 0.4 mm, respectively. The peripheral area of the donor site was significantly higher than the peripheral area of the recipient site (p < 0.01)
ϕ10-mm graft (Fig. 6)
Of note, different from what was observed for the 6- and 8-mm grafts, the VIs of the middle area of the donor site were significantly lower than the peripheral area of the recipient site. Similar to what was observed for the 6- and 8-mm grafts, the peripheral area of the donor site was significantly higher than that of the middle area of the recipient site (p < 0.01).
The VIs in ϕ10-mm grafts. In the donor site, the VIs of the peripheral and the middle areas were 3.4 ± 0.8 mm and 2.0 ± 0.4 mm, respectively. In the recipient site, the VIs of the peripheral and the middle areas were 2.7 ± 0.8 mm and 1.8 ± 0.4 mm, respectively. The middle area of the donor site was significantly lower than the peripheral area of the recipient site. The peripheral area of the donor site was significantly higher than the middle area of the recipient site (p < 0.01)
Discussion
The most important finding of the present study was that the appropriate donor sites in autogenous osteochondral grafting were classified by the location of the injury site and the diameter of osteochondral grafts in terms of matching articular cartilage surface congruency. The goal of articular cartilage repair procedures is to restore the normal biologic and biomechanical properties of the intact articular cartilage, with the ultimate goal of restoring normal joint function [29]. Autogenous osteochondral grafting has been accepted as a procedure for the restoration of the cartilage defect with good clinical results after the first report by Wagner in 1972 [28].
Several authors have reported the importance of joint congruency and recovery from articular cartilage defect after this procedure. Lefkoe et al. reported that the acute treatment for articular step-off injuries was based largely on reduction criteria, because the presence of residual incongruity was correlated with the development of post-traumatic osteoarthritis [19]. Koulalis et al. also indicated key technical factors that affect the success of the procedure, including the overall surface coverage, size and shape of the osteochondral plugs, and congruity of the cartilage thickness between donor and recipient sites [18]. Thus, anatomical restoration of the articular cartilage surface is important. Koh et al. [17], in their study, applied an 80 N load for 120 s to the femoral condyles of 10 swine knees. They measured contact pressures using a prescale film by several conditions of the grafts. Peak contact pressures were significantly elevated by approximately 20 % after defect creation and were reduced to normal when plugs were flush. Large and significant increases in pressure were observed with plugs elevated to 1 and 0.5 mm. The contact pressures with plugs sunk 0.5 and 1 mm were significantly higher than the pressure with intact cartilage but were significantly lower than the pressure in an empty defect. Additionally, elevated angled grafts increased contact pressure [16]. These results suggest that it is preferable to leave an edge slightly sunken rather than elevated. Therefore, precise reconstruction of the original anatomical shape of the recipient region of the articular surface is an essential aspect of successful reconstruction of the joint surface.
Some authors attempted to assess graft matching using this technique. Bartz et al. [2] mounted the condyles of 7 fresh cadaveric femurs on the rotating stage of a laser-based coordinate-measuring machine and developed customized software to allow selection and topographic matching of osteochondral graft donor and recipient sites from any location on the surface of the condyles. They concluded that, for cartilage defects within the weight-bearing portions of the medial or lateral femoral condyles, grafts taken from sites within the most medial or lateral portions of the patellar groove provided a significantly better topographic match than grafts taken from the middle intercondylar notch did. In our previous study, Terukina et al. [27] analysed the curvature of the femoral condyle by performing a stereophotogrammetric examination to develop an optimal autogenous osteochondral transplantation technique. They concluded that the anterior portion of the lateral trochlea matches the weight-bearing area of the femoral condyle, which is often injured, for cartilage thickness and articular curvature. However, this experiment was performed by perpendicular cutting of the femoral condyle; moreover, during surgery, transplantation of the graft in the same plane is difficult. Additionally, the data in that study were evaluated in a two-dimensional plane. In contrast, the data in this study were obtained by 3D laser scanner and assessed by several matching trials.
In this study, the matching of the articular surface shape between the donor site and the recipient site in autogenous osteochondral grafting was assessed. First, the VIs of the osteochondral grafts harvested from the middle one-third area of medial and lateral patellofemoral joint did not differ significantly from the VIs of the ϕ6-mm and ϕ8-mm osteochondral grafts in either the middle one-third or the peripheral one-third area of the medial and lateral tibiofemoral joint. However, the VIs of the ϕ10-mm osteochondral grafts were significantly lower than the VIs of those in the peripheral one-third area of the medial and lateral tibiofemoral joint. These results indicate that the osteochondral graft harvested from the middle one-third area of the patellofemoral joint was a good match to both the middle and the peripheral one-third area in the recipient site, but the ϕ10-mm osteochondral graft harvested from the middle one-third area might be depressed from the peripheral one-third area in the recipient site. Second, the VI of all of the ϕ6-mm-, ϕ8-mm- and ϕ10-mm-diameter osteochondral grafts harvested from the peripheral one-third area of the medial and lateral patellofemoral joint did not differ significantly from the VIs of those harvested from the peripheral one-third area of the medial and lateral tibiofemoral joint. However, the VIs of all of the ϕ6-mm-, ϕ8-mm- and ϕ10-mm-diameter osteochondral grafts harvested from the peripheral one-third area were significantly higher than the VIs of those harvested from the middle one-third area of the medial and lateral tibiofemoral joint. These results imply that an osteochondral graft harvested from the peripheral one-third area of the patellofemoral joint might protrude from the middle one-third area into the recipient site. The scheme of these results is shown in Fig. 7. Therefore, surgeons should take the diameter and location of the graft into consideration to acquire the ideal smooth surface of the recipient site.
The scheme of matching congruency. The osteochondral graft harvested from the peripheral one-third area of the patellofemoral joint might protrude from the middle one-third area into recipient site and the ϕ10-mm osteochondral graft harvested from the middle one-third area might be depressed from the peripheral one-third area into the recipient site
The preferable area for donor site selection based on clinical decision-making was demonstrated in this study. However, the kinematics of a patellofemoral joint should be considered. This surgical technique involves obtaining small-sized cylindrical osteochondral grafts from the minimal weight-bearing periphery of the femoral condyles at the level of the patellofemoral joint and transplanting them to prepared defect sites on the weight-bearing surfaces [13]. The central area of the patellar groove should be avoided for donor site selection, because this area articulates the patella. We excluded this area as a donor site for this study. Additionally, the patella shifts laterally when knees are bent in a flexion position, because the tension on the quadriceps tends to produce a lateral movement of the patella [15, 24]. Therefore, care should be taken while harvesting an osteochondral graft from the lateral side of the patellofemoral joint and a donor graft should be harvested as peripheral as possible. However, our study demonstrated that the osteochondral graft might protrude from the middle area of the recipient site, if it is harvested from the extreme peripheral area. These elevated grafts may increase the contact pressure, as Koh et al. [17] previously reported. These controversial results indicate that the grafts should not be harvested from the lateral but rather the medial middle area of the patellofemoral joint with much regard to avoid the patellar groove area and then transferred into the middle area of the recipient site. Because the contour of the plugs that are harvested cannot be changed and the harvest region has been applied rather liberally for clinical comfort, our matching trial indicates that this technique may reduce the unfortunate selection of an unknown clinical donor region in clinical use.
This study has some limitations. First, we calculated the VIs of both the medial and lateral condyles together, because the number of specimens was small. However, the shape of the medial condyle differs from that of the lateral condyles. Further evaluation of matching in the medial and lateral condyles separately is required. Second, the number of specimens was small. A larger number of knees are needed to research accurate matching. Third, the ages of the cadavers were advanced. Although the knee joint of all cadavers appeared to be structurally normal and no osteoarthritic change was seen on visual inspection, the average age of the cadavers was 75.8 years, which is older than the average age of patients who require osteochondral graft transplantation. Finally, we evaluated the middle and the peripheral areas as donor areas and excluded the central area of the patellofemoral joint. The central area of the patellofemoral joint surface articulates the patella and the patella shifts laterally with knee flexion as we mentioned above. The matching congruencies of articular cartilage surface in autogenous osteochondral grafting between donor sites and recipient sites were demonstrated; however, the middle area in the patellofemoral joint might be an inappropriate area as a donor site. As a clinical relevance, this study will be useful for improving the donor site selection as a pre-operative planning in this technique by using data derived from CT and MRI scans of the knee.
Conclusion
The matching of the articular surface shape between the donor site and the recipient site in autogenous osteochondral grafting was assessed. The osteochondral graft harvested from the peripheral one-third area of the patellofemoral joint might protrude from the middle one-third area into the recipient site, and the ϕ10-mm osteochondral graft harvested from the middle one-third area of the patellofemoral joint might be depressed from the peripheral one-third area into the recipient site. However, the lateral middle one-third area of the patellofemoral joint in the donor site might be taken from the medial side, because patella shifts laterally with knee flexion.
References
Bader S, Miniaci A (2011) Mosaicplasty. Orthopedics 34(9):e491–e493
Bartz RL, Kamaric E, Noble PC, Lintner D, Bocell J (2001) Topographic matching of selected donor and recipient sites for osteochondral autografting of the articular surface of the femoral condyles. Am J Sports Med 29(2):207–212
Bekkers JE, Inklaar M, Saris DB (2009) Treatment selection in articular cartilage lesions of the knee: a systematic review. Am J Sports Med 37(Suppl 1):148S–155S
Beris AE, Lykissas MG, Kostas-Agnantis I, Manoudis GN (2012) Treatment of full-thickness chondral defects of the knee with autologous chondrocyte implantation: a functional evaluation with long-term follow-up. Am J Sports Med 40(3):562–567
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331(14):889–895
Cain EL, Clancy WG (2001) Treatment algorithm for osteochondral injuries of the knee. Clin Sports Med 20(2):321–342
Caplan AI, Elyaderani M, Mochizuki Y, Wakitani S, Goldberg VM (1997) Principles of cartilage repair and regeneration. Clin Orthop Relat Res 342:254–269
Chow JC, Hantes ME, Houle JB, Zalavras CG (2004) Arthroscopic autogenous osteochondral transplantation for treating knee cartilage defects: a 2- to 5-year follow-up study. Arthroscopy 20(7):681–690
Edgar D, Day R, Briffa NK, Cole J, Wood F (2008) Volume measurement using the Polhemus FastSCAN 3D laser scanning: a novel application for burns clinical research. J Burn Care Res 29(6):994–1000
Gilbert JE (1998) Current treatment options for the restoration of articular cartilage. Am J Knee Surg 11(1):42–46
Gudas R, Kalesinskas RJ, Kimtys V, Stankevicius E, Toliusis V, Bernotavicius G, Smailys A (2005) A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 21(9):1066–1075
Hangody L, Dobos J, Balo E, Panics G, Hangody LR, Berkes I (2010) Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study. Am J Sports Med 38(6):1125–1133
Hangody L, Rathonyi GK, Duska Z, Vasarhelyi G, Fules P, Modis L (2004) Autologous osteochondral mosaicplasty. Surgical technique. J Bone Joint Surg Am 86-A(Suppl 1):65–72
Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, Bodo G (2008) Autologous osteochondral grafting–technique and long-term results. Injury 39(Suppl 1):S32–S39
Hungerford DS, Barry M (1979) Biomechanics of the patellofemoral joint. Clin Orthop Relat Res 144:9–15
Koh JL, Kowalski A, Lautenschlager E (2006) The effect of angled osteochondral grafting on contact pressure: a biomechanical study. Am J Sports Med 34(1):116–119
Koh JL, Wirsing K, Lautenschlager E, Zhang LO (2004) The effect of graft height mismatch on contact pressure following osteochondral grafting: a biomechanical study. Am J Sports Med 32(2):317–320
Koulalis D, Di Benedetto P, Citak M, O’Loughlin P, Pearle AD, Kendoff DO (2009) Comparative study of navigated versus freehand osteochondral graft transplantation of the knee. Am J Sports Med 37(4):803–807
Lefkoe TP, Trafton PG, Ehrlich MG, Walsh WR, Dennehy DT, Barrach HJ, Akelman E (1993) An experimental model of femoral condylar defect leading to osteoarthrosis. J Orthop Trauma 7(5):458–467
Lindholm TS, Osterman K, Kinnunen P, Lindholm TC, Osterman HK (1982) Reconstruction of the joint surface using osteochondral fragments. An experimental and clinical study. Scand J Rheumatol Suppl 44:5–46
Liu X, Kim W, Drerup B, Mahadev A (2005) Tibial torsion measurement by surface curvature. Clin Biomech (Bristol, Avon) 20(4):443–450
Mayhew TA, Williams GR, Senica MA, Kuniholm G, Du Moulin GC (1998) Validation of a quality assurance program for autologous cultured chondrocyte implantation. Tissue Eng 4(3):325–334
McKernan B, Bydder SA, Deans T, Nixon MA, Joseph DJ (2007) Surface laser scanning to routinely produce casts for patient immobilization during radiotherapy. Australas Radiol 51(2):150–153
Mizuno Y, Kumagai M, Mattessich SM, Elias JJ, Ramrattan N, Cosgarea AJ, Chao EY (2001) Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res 19(5):834–840
Nakagawa Y, Suzuki T, Kuroki H, Kobayashi M, Okamoto Y, Nakamura T (2007) The effect of surface incongruity of grafted plugs in osteochondral grafting: a report of five cases. Knee Surg Sports Traumatol Arthrosc 15(5):591–596
O’Driscoll SW, Keeley FW, Salter RB (1988) Durability of regenerated articular cartilage produced by free autogenous periosteal grafts in major full-thickness defects in joint surfaces under the influence of continuous passive motion. A follow-up report at one year. J Bone Joint Surg Am 70(4):595–606
Terukina M, Fujioka H, Yoshiya S, Kurosaka M, Makino T, Matsui N, Tanaka J (2003) Analysis of the thickness and curvature of articular cartilage of the femoral condyle. Arthroscopy 19(9):969–973
Wagner H (1972) Moglichkeitin und klinische Erfahrungen mit der Knorpletransplantation. Z Orthop 110:705–708
Yuan TY, Huang CY, Yong Gu W (2011) Novel technique for online characterization of cartilaginous tissue properties. J Biomech Eng 133(9):094504
Acknowledgments
We would like to thank Ms. Janina Tubby for her excellent editing assistance in preparing this manuscript, Nojigiku-Kai, the society that donated the cadavers to Kobe University and Professor Toshio Terashima, M.D., Ph.D., Division of Developmental Neurobiology, Department of Physiology and Cell Biology in Kobe University Graduate School of Medicine, for support in the analysis of the cadaveric knees.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Araki, D., Kuroda, R., Matsumoto, T. et al. An analysis of surface profile for cylindrical osteochondral grafts of the knee quantitative evaluation using a three-dimensional laser scanner. Knee Surg Sports Traumatol Arthrosc 21, 1794–1800 (2013). https://doi.org/10.1007/s00167-012-2106-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2106-3