Abstract
Purpose
Reduction in blood loss during surgery stabilizes hemodynamic status and aids in recovery after total knee arthroplasty (TKA). In this study, the authors examined whether different administration routes of tranexamic acid (TNA) might affect the amount of blood loss after TKA.
Methods
A total of 150 patients were prospectively allocated to each of the three groups (intravenous, intra-articular, and placebo group) and underwent unilateral TKA. During closing the operative wound, TNA (1.5 g mixed in 100 cc of saline) was administered intravenously or intra-articularly according to the enrolled group, and an equivalent volume of normal saline was administered into the knee joint cavity and intravenously in the placebo group, respectively. The amount of blood loss and transfusion, and changes in haemoglobin levels were documented accordingly.
Results
The mean blood loss in the intravenous, intra-articular, and placebo groups were 528 ± 227, 426 ± 197, and 833 ± 412 ml, respectively. About 66 % (intravenous), 80 % (intra-articular), and 6 % (placebo) of each group did not require transfusion for any reason, and the mean amount of transfusion was 273.6, 129.6, and 920.8 ml, respectively. Preoperative haemoglobin values decreased by 1.6 ± 0.8, 1.8 ± 0.8, and 2.0 ± 0.9 mg/dl, respectively.
Conclusion
Compared to intravenous administration, intra-articular administration of TNA seems to be more effective in terms of reducing blood loss and transfusion frequency. TNA may improve the general conditions of patients given TKA by maintaining a hemodynamically stable state, aiding in recovery, and reducing the chance of transfusion-associated side effects and complications.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies reported that as much as 1,000–1,790 ml of blood was lost during total knee arthroplasty (TKA) [5, 6, 20] and that 10–38 % of patients required 1–2 units of allogenic blood transfusion accordingly [3, 12, 14, 19]. Since the side effects and complications are rather common after transfusion, maintaining hemodynamic stability seems to be important and aids in fast recovery after TKA [7].
In order to reduce blood loss during TKA, many methods have been introduced, such as, autologous transfusion [26], hypotensive anaesthesia [17], drain clamping [25, 26], the application of fibrin tissue adhesive [21] or a compression bandage, and cryotherapy [10, 16]. Additionally, intravenous (IV) or intra-articular administration of tranexamic acid (TNA) is known to reduce transfusion frequency and bleeding before and after surgery [11, 13, 14, 16, 19, 23, 30, 31, 33].
Tranexamic acid is an antifibrinolytic agent that activates plasminogen and stops bleeding by inducing blood clot formation [4, 14, 20, 29, 30]. At present, TNA is used to stop excessive bleeding during dental [29], cardiac [1, 9], spine [32], and hip surgeries [5, 20]. However, little information is available regarding the comparative efficacy of TNA according to the administration route. Thus, this study was prospectively designed to determine which administration route of TNA is more efficacious hemodynamically after TKA. It was hypothesized that intra-articular administration of TNA would significantly reduce the blood loss and help maintaining hemodynamical stability.
Materials and methods
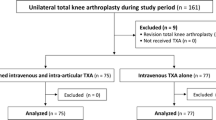
This prospective, randomized, placebo-controlled study was performed on 150 patients who underwent unilateral TKA from 1 May 2011 to 31 September 2011. Before starting this trial, the study protocol was approved by our institutional review board.
The inclusion criterion was patients aged between 55 and 80 years who planned to undergo TKA due to degenerative arthritis on a knee joint. Exclusion criteria were as follows: patients with any cardiovascular problems (such as myocardiac infarction history, atrial fibrillation, angina), patients with cerebrovascular conditions (such as previous stroke or vascular surgery history), patients with thromboembolic disorders, or those exhibiting a deteriorating general condition.
Patients were randomly allocated to each of the intravenous, intra-articular, and placebo groups using a random number list. There were no differences in the demographic factors among groups (Table 1).
Operation procedures and postoperative protocol
All patients underwent TKA using extramedullary alignment technique by a single surgeon (JGS). After applying a pneumatic tourniquet, approaches were made using a modified antero-medial parapatellar incision. After soft tissue balancing, extramedullary minimal invasive surgery (EM-MIS) technique was used to resect femoral and tibial bones [28], and same types of prosthesis (Scorpio® NRG, Stryker, NJ) were fitted for all patients. Meticulous electric cauterization of soft tissue bleeding was performed during surgery.
For patients in the intravenous group, 1.5 g of TNA in 100 cc of saline was administered immediately after closing surgical sites. In intra-articular group, patients were given 1.5 g of TNA in 100 cc of saline directly into the knee joint cavity while suturing. Patients in placebo group were administered an equivalent volume of normal saline into the joint space and intravenously.
Tourniquets were not released until finishing skin closure. Two intra-articular drains were left in situ for 24 h for postoperative bleeding. After removal of drains, ROM exercise and walker-aided ambulation were encouraged. All the patients were followed up postoperatively after 2 months.
Outcome measures
The amount of drainage was recorded in order to estimate the blood loss during TKA, and the difference in haemoglobin levels between the preoperative and the postoperative lowest one was also calculated. The frequency of transfusion, the number of blood units transfused, any perioperative complications or events such as infection, deep vein thrombosis (DVT), and pulmonary embolism were also recorded accordingly.
The necessity for transfusion was determined based on the guidelines for perioperative transfusion by the National Institutes of Health Consensus Conference, which suggested that decision should be made based on the clinical assessment aided by laboratory data, patients’ symptoms and anaemic signs. Thus, transfusion was allowed only for the patients whose haemoglobin level was less than 8.0 g/dl or whose haemoglobin level was less than 10.0 g/dl with concomitant intolerable anaemic symptoms or any anaemia-related organ dysfunctions.
Statistical analysis
The Kruskal–Wallis test was used to analyse the amount of blood loss, difference in haemoglobin levels, the amount and frequency of transfusion. Post hoc analysis was conducted with the multiple comparison Tukey’s test using ranks to test the null hypothesis. All analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC, USA), and statistical significance was accepted for p values of <0.05.
Results
Mean blood losses during surgery in the intravenous, intra-articular, and placebo groups were 528 ± 227, 426 ± 197, and 833 ± 412 ml, respectively, with significant intergroup differences (p value <0.001) (Fig. 1). Both TNA groups resulted in significantly less amount of blood loss compared to the placebo group, and among the TNA groups, intra-articular administration of TNA yielded less blood loss than intravenous injection.
Among 50 patients in each group, 33 (66 %) in intravenous, 40 (80 %) in intra-articular, and 3 (6 %) in placebo did not require transfusion (p value <0.001) (Fig. 2).
The average amounts of transfusion (packed RBCs) were also significantly different among groups and were 273.6 ml in intravenous, 129.6 ml in intra-articular, and 920.8 ml in placebo, respectively (p value <0.001) (Table 2).
Compared to preoperative haemoglobin level, postoperative one decreased by 1.6 ± 0.8, 1.8 ± 0.8, and by 2.0 ± 0.9 mg/dl in the intravenous, intra-articular, and placebo groups, respectively (Table 2).
Postoperative complications included 5 cases of DVT and 2 cases of atrial fibrillation. Two cases of DVT developed in the placebo group and 3 in the intravenous group, and one case of atrial fibrillation was encountered in each of the placebo and intravenous group. The frequency of complications in each group was not statistically significant. No fatal complication, such as pulmonary embolism, occurred among study groups. Patients with DVT or atrial fibrillation were discharged from hospital after symptomatic improvement (Table 3).
The average range of motion (ROM) at 2 months were 2.6°–123.3°, 2.5°–120.4°, and 2.9°–124.1° in the intravenous, intra-articular, and placebo groups with no significant statistical difference in intergroup analysis.
Discussion
The most important finding of the present study is that TNA reduces blood loss in TKA and the need for transfusion accordingly. Comparing two TNA groups, intra-articular injection of TNA seems to be more effective than intravenous injection in terms of the amount of blood loss and the need for transfusion.
Intra-articular injection at the surgical site provides direct and straightforward means of application before tourniquet releasing [16, 33]. In addition, intra-articular TNA injection has the advantage of inducing partial microvascular haemostasis by stopping fibrin clot dissolution in the affected area. Once injected intra-articularly, TNA is rapidly absorbed and maintains a biological half-time of approximately 3 h within joint fluid [13, 19, 20, 23].
A concern exists on the use of TNA that antifibrinolytic effect of TNA may cause thromboembolic complications in patients given TKA [2, 18, 25, 30]. Due to the concern, patients with a history of a cardiac problem or with a thromboembolic disease were excluded from this study enrolment, and a relatively low dose of TNA was administered based on the review of previous studies. We suspect that the complication rate following TNA administration is small because systemic absorption is low when administered intra-articularly. Furthermore, no thromboembolic complications such as DVT or pulmonary embolism have been encountered after intra-articular injection of TNA in the present or in the previous studies [1, 15, 33]. However, our results lacked statistical significance, and thus, a larger-scale study is required. According to the meta-analyses conducted on the topic, the risk of venous thromboembolism is not increased by TNA, but great care is mandatory in patient selection and in the choice of administration route and dosage because of the antifibrinolytic effect of TNA [4, 12, 18].
Previous relevant studies have been conducted in various protocols including different TNA dosages to reduce blood loss and transfusion frequency [2, 13, 30, 32, 33]. The results revealed that high TNA dosages did not increase the frequency of thromboembolic complications. Despite the promising results of use of high TNA doses, the lowest effective dosage seems to be desirable to minimize the potential thromboembolic complications after TNA administration. Others have argued that TNA is effective for reducing blood loss but does not reduce transfusion amounts or frequencies since, although TNA decreases over 50 % of drainage and reduces blood loss. TNA still cannot reduce hidden blood loss [12, 27].
In the present study, intra-articular and intravenous use of TNA resulted in less blood loss through drainage and reduced transfusion frequencies and amounts. Thus, TNA seems to improve the general conditions of patients given TKA by maintaining a hemodynamically stable state and by reducing the transfusion-associated side effects and complications. In particular, TNA use may aid early rehabilitation and functional recovery, and reduce hospital stay by reducing the risk of an anaemic status [8, 24].
The overall blood loss in this study was also less compared to the blood loss in general conventional TKA. As explained in the “Materials and methods” section, all TKAs were performed using less invasive EM-MIS technique, which, we believe, caused overall less blood loss. Since the severity of medullary canal injury is reduced by the EM method and soft tissue injury is reduced by MIS, perhaps over 1,000 ml of blood loss could be prevented [16]. According to Lin et al. [22], blood loss of up to 1,453 ml (733–2,537 ml) occurs during MIS-TKA, and about 20 % of blood loss was prevented when intravenous TNA administration was applied to MIS-TKA group. Wong et al. [33] also reported that intra-articular TNA use achieved more than 400 ml reduction in blood loss compared to 1,610 ml (1,480–1,738) loss observed in the placebo group, with 1,208 ml (1,078–1,339 ml) in the 3.0 g TNA group and 1,295 ml (1,167–1,422 ml) in 1.5 g TNA group. Compared to Wong’s study, our results demonstrated reduction in blood loss by at least 400 ml in all groups, and the blood loss in placebo group was even less than conventional TKA group with TNA use.
Several limitations should be considered in this study. First, although the present study was conducted with a relatively larger number of patients than previous studies, its statistical power was not high enough, and thus, further studies are required to confirm our findings. Second, because all surgeries were performed using the EM-MIS technique, we were unable to compare our findings with conventional TKA under the same circumstance. Third, ultrasonographic study on asymptomatic DVT occurrence and study on blood concentration of TNA after surgery were not progressed. Forth, the effects of TNA on rehabilitation and recovery were not investigated. Despite the potential limitations, the advantage of this study is that it is the most extensive study to date conducted in prospective randomized controlled design [12, 16, 20, 30].
The intra-articular use of TNA in TKA patients showed less blood loss through drainage and reduced transfusion frequencies and amounts. Furthermore, intra-articular TNA injection is easy to perform and cost-effective as compared with topical sealants. Thus, TNA may play a part in improving the general conditions of patients given TKA by maintaining a hemodynamically stable state and reducing the chance of transfusion-associated side effects and complications.
Conclusion
This prospective comparative study showed that during TKA, TNA reduced blood loss and helped reducing transfusion amounts and frequencies with negligible side effects. With regard to administration route, intra-articular administration of TNA seemed to be more effective than intravenous injection in terms of blood loss and transfusion frequency.
References
Abrishami A, Chung F, Wong J (2009) Topical application of antifibrinolytic drugs for on-pump cardiac surgery: a systematic review and meta-analysis. Can J Anaesth 56:202–212
Álvarez JC, Santiveri FX, Ramos I, Vela E, Puig L, Escolano F (2008) Tranexamic acid reduces blood transfusion in total knee arthroplasty even when a blood conservation program is applied. Transfusion 48:519–525
Barsoum WK, Klika AK, Murray TG, Higuera C, Lee HH, Krebs VE (2011) Prospective randomized evaluation of the need for blood transfusion during primary total hip arthroplasty with use of a bipolar sealer. J Bone Joint Surg Am 93:513–518
Benoni G, Fredin H (1996) Fibrinolytic inhibition with tranexamic acid reduces blood loss and blood transfusion after knee arthroplasty: a prospective, randomised, double-blind study of 86 patients. J Bone Joint Surg Br 78:434–440
Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB (1999) An analysis of blood management in patients having a total hip or knee. J Bone Joint Surg Am 81:2–10
Bong M, Patel V, Chang E, Issack P, Hebert R, Di Cesare P (2004) Risks associated with blood transfusion after total knee arthroplasty. J Arthroplasty 19:281–287
Camarasa MA (2006) Efficacy of aminocaproic, tranexamic acids in the control of bleeding during total knee replacement: a randomized clinical trial. Br J Anaesth 96:576–582
Diamond PT, Conaway MR, Mody SH, Bhirangi K (2006) Influence of hemoglobin levels on inpatient rehabilitation outcomes after total knee arthroplasty. J Arthroplasty 21:636–641
Fawzy H, Elmistekawy E, Bonneau D, Latter D, Errett L (2009) Can local application of tranexamic acid reduce post-coronary bypass surgery blood loss? A randomized controlled trial. J Cardiothorac Surg 4:25
Gibbons CE, Solan MC, Ricketts DM, Patterson M (2001) Cryotherapy compared with Robert Jones bandage after total knee replacement: a prospective randomized trial. Int Orthop 25:250–252
Gill JB, Chin Y, Levin A, Feng D (2008) The use of antifibrinolytic agents in spine surgery. A meta-analysis. J Bone Joint Surg Am 90:2399–2407
Good L, Peterson E, Lisander B (2003) Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br J Anaesth 90:596–599
Hiippala ST, Strid LJ, Wennerstrand MI, Arvela JV, Niemela HM, Mantyla SK, Kuisma RP, Ylinen JE (1997) Tranexamic acid radically decreases blood loss and transfusions associated with total knee arthroplasty. Anesth Analg 84:839–844
Hippala S, Strid L, Wennerstrand M, Arvela V, Mantyla S, Ylinen J (1995) Tranexamic acid (Cyklokapron) reduces perioperative blood loss. Br J Anaesth 74:534–537
Ishida K, Matsumoto T, Tsumura N, Kubo S, Kitagawa A, Chin T, Iguchi T, Kurosaka M, Kuroda R (2011) Mid-term outcomes of computer-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1107–1112
Ishida K, Tsumura N, Kitagawa A, Hamamura S, Fukuda K, Dogaki Y, Kubo S, Matsumoto T, Matsushita T, Chin T, Iguchi T, Kurosaka M, Kuroda R (2011) Intra-articular injection of tranexamic acid reduces not only blood loss but also knee joint swelling after total knee arthroplasty. Int Orthop 35:1639–1645
Juelsgaard P, Larsen UT, Sorensen JV, Madsen F, Soballe K (2001) Hypotensive epidural anesthesia in total knee replacement without tourniquet: reduced blood loss and transfusion. Reg Anesth Pain Med 26:105–110
Kagoma YK, Crowther MA, Douketis J, Bhandari M, Eikelboom J, Lim W (2009) Use of antifibrinolytic therapy to reduce transfusion in patients undergoing orthopedic surgery: a systematic review of randomized trials. Thromb Res 123:687–696
Kalairajah Y, Simpson D, Cossey AJ, Verrall GM, Spriggins AJ (2005) Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br 87:1480–1482
Krohn CD, Sorensen R, Lange JE, Riise R, Bjornsen S, Brosstad F (2003) Tranexamic acid given into the wound reduces postoperative blood loss by half in major orthopaedic surgery. Eur J Surg 588:57–61
Levy O, Martinowitz U, Oran A, Tauber C, Horoszowski H (1999) The use of fibrin tissue adhesive to reduce blood loss and the need for blood transfusion after total knee arthroplasty. A prospective, randomized, multicenter study. J Bone Joint Surg Am 81:1580–1588
Lin PC, Hsu CH, Chen WS, Wang JW (2011) Does tranexamic acid save blood in minimally invasive total knee arthroplasty? Clin Orthop Relat Res 469:1995–2002
Molloy DO, Archbold HA, Ogonda L, McConway J, Wilson RK, Beverland DE (2007) Comparison of topical fibrin spray and tranexamic acid on blood loss after total knee replacement: a prospective, randomised controlled trial. J Bone Joint Surg Br 89:306–309
Napolitano LM (2005) Perioperative anemia. Surg Clin N Am 85:1215–1227
Onodera T, Majima T, Sawaguchi N, Kasahara Y, Ishigaki T, Minami A (2012) Risk of deep venous thrombosis in drain clamping with tranexamic acid and carbazochrome sodium sulfonate hydrate in total knee arthroplasty. J Arthroplasty 27:105–108
Parvizi J, Chaudhry S, Rasouli MR, Pulido L, Joshi A, Herman JH, Rothman RH (2011) Who needs autologous blood donation in joint replacement? J Knee Surg 24:25–31
Sasanuma H, Sekiya H, Takatoku K, Takada H, Sugimoto N, Hoshino Y (2011) Efficient strategy for controlling postoperative hemorrhage in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:921–925
Seo JG, Moon YW, Lim JS, Park SJ, Kim SM (2011) Mechanical axis-derived femoral component rotation in extramedullary total knee arthroplasty: a comparison between femoral transverse axis and transepicondylar axis. Knee Surg Sports Traumatol Arthrosc 20:538–545
Sindet-Pedersen S, Ramström G, Bernvil S, Blombäck M (1989) Hemostatic effect of tranexamic acid mouthwash in anticoagulant-treated patients undergoing oral surgery. N Engl J Med 320:840–843
Sukeik M, Alshryda S, Haddad FS, Mason JM (2011) Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br 93:39–46
Tanaka N, Sakahashi H, Sato E, Hirose K, Ishima T, Ishii S (2001) Timing of the administration of tranexamic acid for maximum reduction in blood loss in arthroplasty of the knee. J Bone Joint Surg Br 83:702–705
Tse E, Cheung W, Ng K, Luk K (2011) Reducing perioperative blood loss and allogeneic blood transfusion in patients undergoing major spine surgery. J Bone Joint Surg Am 93:1268–1277
Wong J, Abrishami A, El Beheiry H, Mahomed NN, Roderick Davey J, Gandhi R, Syed KA, Muhammad Ovais Hasan S, De Silva Y, Chung F (2010) Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: a randomized, controlled trial. J Bone Joint Surg Am 92:2503–2513
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seo, JG., Moon, YW., Park, SH. et al. The comparative efficacies of intra-articular and IV tranexamic acid for reducing blood loss during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21, 1869–1874 (2013). https://doi.org/10.1007/s00167-012-2079-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2079-2