Abstract
Purpose
The purpose was to prospectively evaluate the two-year results after implantation of the Journey PFJ® (Smith & Nephew, Andover, MA). The authors hypothesized that patellofemoral arthroplasty would result in improved outcomes after 24 months in patients treated with an isolated procedure as well as in patients demonstrating concomitant patellofemoral instability (PFI), which were treated with a combined surgical procedure.
Methods
Patients were included between 02/2006 and 08/2008. According to the history and clinical findings, patients were grouped into group I with no history or clinical signs of PFI, and patients with concomitant PFI were assorted to group II. Patients were then treated with an isolated (group I) or a combined (group II) surgical procedure to additionally treat the PFI. Visual analogue scale (VAS), Lysholm score and WOMAC score were recorded preoperatively, 6, 12 and 24 months postoperatively. Patellar height was evaluated according to the index of Caton-Deschamps (CDI), and osteoarthritic changes were evaluated according to Kellgren and Lawrence.
Results
A total of 25 patients were enrolled, of them three discontinued interventions and were excluded from final analysis. An isolated implantation of the Journey PFJ® was performed in 14 patients (group I) and a combined procedure in 8 (group II). Daily pain and clinical scores significantly improved at 6, 12 and 24 months compared to preoperative values (P < 0.05). Significant decrease (P = 0.02) of mean CDI could be noticed. Significant increase in tibiofemoral OA within the medial but not in the lateral tibiofemoral joint was assessed (P = 0.011; n.s.).
Conclusions
Patellofemoral arthroplasty using the Journey® PFJ for treatment of significant patellofemoral OA demonstrated improved clinical scores at the 2-year follow-up in both groups. Comparing the primary OA (I) and OA + instability (II) groups, patients with patellofemoral OA treated with a combined procedure for concomitant stabilization of patellofemoral instability may benefit more from such a combined procedure, than patients treated with an isolated procedure for treatment of isolated patellofemoral OA.
Level of evidence
Prospective case series, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of isolated patellofemoral osteoarthritis (OA) still remains challenging, and various modalities have been developed [16, 19, 22]. Today, no general “gold standard” of treatment can be defined. Non-operative treatment (e.g., strengthening exercises, braces, medications and activity modification) may provide sufficient pain relief in early stages of disease. However, some patients with severe disease may still require operative management [14, 17]. Out of these surgical options, previous unicompartmental arthroplasties for the patellofemoral joint demonstrated variable results [14, 16, 18, 21, 23]. The challenges to PFJ arthroplasty lie in its complex anatomy and kinematics, both of which have to be respected in order to obtain optimal results [16, 17, 22, 23]. However, patellofemoral arthroplasty has regained importance in clinical practice due to the recent emergence of more anatomical implant designs and increasing knowledge of pathomorphology as well as how to avoid surgical failures [17]. Current implant designs incorporated in the Journey PFJ® (Smith & Nephew, Andover, MA, USA) may allow for anatomical patellofemoral kinematics, such as an asymmetric trochlear groove, which is deepened and lateralized as well as fixation pegs, which allow for changes in all implant sizes throughout trialling.
Special emphasis has to be laid on the differentiation of causative factors for the development of patellofemoral OA, such as chronic patellofemoral instability (PFI). Most cases of PFI are due to dysplasia of the trochlea, with subsequent insufficiency of the medial passive stabilizers [1]. In situations of persisting instability and non-physiological kinematics (patellar mal-tracking), key pathologies have to be evaluated and a combined surgical approach should be undertaken to reproduce physiological patellar tracking following the arthroplasty [9, 29]. According to the recent literature as well as the authors’ clinical experience, techniques such as anatomical reconstruction of the medial patellofemoral ligament (MPFL) and/or tibio-femoral osteotomies to correct malalignment may be beneficial for this purpose [1, 6, 11, 27, 29]. Underscoring this point, several previously published studies on patellofemoral arthroplasty have shown that the best results are obtained in patients with patellofemoral OA due to trochlea dysplasia and after restitution of the previous patellofemoral instability [2, 4, 7].
The purpose of this study was to prospectively evaluate the clinical and radiological two-year results after implantation of the Journey PFJ® in patients with patellofemoral OA. We hypothesized that PFJ arthroplasty would result in improved clinical outcomes after 24 months in patients treated with an isolated procedure as well as in patients demonstrating concomitant PFI, which were treated with a combined surgical procedure for patellar stabilization.
Materials and methods
Patients
Between February 2006 and August 2008, 25 patients were treated with implantation of the Journey PFJ® in the Department of Orthopedic Sports Medicine of the Technische Universität München (Munich, Germany). Inclusion criteria were symptomatic high-grade OA of the patellofemoral compartment (grades III–IV according to the Kellgren classification) and failed conservative treatment (anti-inflammatory drugs/-injections, stretching of quadriceps muscle and functional training of leg axis) [15]. Exclusion criteria were high-grade tibiofemoral OA, inflammatory or systemic diseases, autoimmune diseases, psychiatric conditions, imprisonment or pregnancy. All patients gave their written informed consent before being included in the study. According to the patient’s history and clinical findings, they were grouped into group I with no history or clinical signs of patellofemoral instability. Patients with a history of patellofemoral instability and clinical symptoms of PFI (such as: persisting clinical signs of positive apprehension spontaneously or when the patellar was lateralized) were assorted to group II. Patients were assorted to each group due to the individual decision for treatment made by the attending surgeon. A group of 4 surgeons performed the procedures and all were done in ischaemia (tourniquet).
Implant and surgical technique
If no additional surgery was performed, a lateral standardized minimal invasive surgical approach without eversion of the patellar was used to protect the medial soft tissue structures. In short, after accessing the joint, the bony resection of the anterior portion of the trochlea was performed using the manufacturer’s intramedullary guiding instrument. Then, the trochlea was deepened by guided reaming. Special care was taken to ensure a proper fit of the implant without femoral notching or over-stuffing. After satisfying patellar alignment, which was tested with the trial implant, the final implant is inserted and fixed with bone cement (Figs. 1, 2). The undersurface of the patella was visually inspected. If a high-grade deformity was present, a resurfacing of the undersurface was added [24]. Postoperatively, the patients perform partial weight bearing (20 kg) for 2 weeks, followed by progression of weight bearing with ca. 20 kg per week. Full range of motion is allowed immediately postoperatively.
Combined surgical procedures
According to the patient’s history and clinical findings, they were treated with an isolated (group I) or combined (group II) procedure. This decision was based on the senior author’s routinely used clinical algorithm for treatment of symptomatic patellofemoral instability. Briefly, PFI was addressed with a concomitant soft tissue procedure if the patient’s history and clinical examination (positive apprehension sign in 0–30° of flexion) were consistent with instability in early degrees of flexion. This was done via double bundle MPFL reconstruction [27]. If valgus malalignment and/or increased femoral internal torsion was ascertained via radiographic (CT scan) imaging, supracondylar osteotomy was performed to either straighten the leg axis or/and perform a de-torsion of the femur [6]. In cases of TTTG > 20 mm, a tibial tubercle osteotomy and medialization were performed [13]. Due to the specific design of the implant (creates deepened trochlea groove), any kind of trochlea dysplasia was addressed. Therefore, this factor for instability was not necessary to be addressed with an additional procedure, such as trochleoplasty.
Clinical follow-up and evaluation
All patients were analysed using the Lysholm and the WOMAC scores preoperatively, and 6, 12 and 24 months after the surgical procedure [5, 20]. All clinical data were collected by one of the authors (not a participating surgeon). Additionally, the pain self-evaluation was measured with the use of a visual analogue scale (VAS score) at all time points (score of 0 indicated no pain and 10 indicated an extreme amount). Range of motion (ROM) was assessed with a standard goniometer with the arms aligned along the long axes of the femur and tibia on the lateral side of the knee joint.
Radiological follow-up and scoring
All radiological data were evaluated and calculated digitally (PACS, Philips Medical Systems, Sectra Imtec AB, Sweden) by one single author (not a participating surgeon). Radiological evaluation included weight-bearing antero-posterior (AP) and lateral radiographs as well a tangential view of the patellofemoral joint taken at 30° using the Merchant technique. The AP radiograph and the tangential view were scored for the severity of osteoarthritis within the tibiofemoral and patellofemoral joint using the systems described by Kellgren and Lawrence [15]. The lateral radiograph was scored for the patellar height according to Caton et al. [8]. This method has been used in previous studies and has been proven for its accuracy and reliability [12].
Statistical analysis
Data were analysed using SPSS for Windows version 19.0 (SPSS Inc., Chicago, IL, USA). Mean values ± standard deviation and range were reported for quantitative normal distributed measurements. Non-normal data distribution, median value with interquartile range (IQR: from 25th to the 75th percentile), was reported. For VAS-, Lysholm- and WOMAC-score evaluation, the nonparametric Friedman test for related samples was used pairwise to evaluate changes about time in each group as well as in the whole study population. If the test showed significant differences over time, the nonparametric Wilcoxon test for two related samples was used in each group to compare between two different time points. On graphs, median values with 95 % confidence intervals were displayed by error bars. Statistical analyses were performed two sided. A P value of <0.05 was considered significant. An a priori power analysis was calculated with a difference to detect 25 points and a standard deviation of 20 points in the Lysholm score. It established a sample size of 10 patients for a power of 80 %.
Results
Patients and surgical procedures
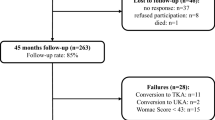
Within the time of enrolment, no patient had to be excluded due to the exclusion criteria. For enrolment, 25 patients were involved, of them three discontinued interventions and were excluded (1× late infection, 1× transfer to total joint, and 1× denied further participation in study due to prostate cancer). For analysis, 22 patients were followed through all evaluations and the final 24-month follow-up (Fig. 3). An isolated implantation of the Journey PFJ® (Smith & Nephew) was performed in 14 patients (group I). Eight patients of group I had a history of previous patellofemoral surgeries (6× retro-patellar debridement/shaving, 1× microfracture, 1× OATS), and previous patellar fractures were found in 2 patients. A combined procedure was performed in the remaining 8 patients [Group II] (three reconstructions of the MPFL, two medial tightening, one distal femur osteotomy, one distal femur osteotomy in combination with a reconstruction of the MPFL and one distal femur osteotomy). Previous surgeries of group II included 2× retro-patellar debridement/shaving, 1× transfer of the tibial tubercle, and 1 patient had a history of previous patellar fracture. No intraoperative complications such as intra-articular fracture, nerve or vessel damage were noted. In 6 cases of group I, patellar resurfacing was performed in contrast to none in group II. Patient characteristics are summarized in Table 1.
Clinical scores
Daily pain significantly decreased at 6, 12 and 24 months compared to preoperative values (P < 0.05). Furthermore, significant differences were found between 6 and 12 (P = 0.002) months after surgery. Compared to preoperative values, subjective knee function scores (Lysholm) were also improved at 6, 12, and 24 months after surgery (P < 0.05). Further significant increase was found only between 6 and 12 (P = 0.003) months after surgery. Also there were significant improvements in the WOMAC score at 6, 12 and 24 months after surgery (P < 0.05). Additional significant improvement was only found comparing 6 and 12 months after surgery (P < 0.001). The maximum passive flexion 24 months after surgery showed no significant difference compared to preoperative status.
Group I
Evaluating the VAS score, significant decreases in daily pain at 6, 12 and 24 months compared to preoperative status were found at all time points (Fig. 4). Concerning subjective knee function, compared to preoperative values, significant improvements could be detected 6, 12 and 24 months after surgery using the Lysholm scoring system (6, 12 and 24 months, P < 0.05). Further significant increase was found between 6 and 12 (P = 0.035) but not between 12 and 24 months after surgery (Fig. 5). Compared to preoperative osteoarthritic index (WOMAC), there were significant improvements at 6, 12 and 24 months after surgery (6, 12 and 24 months, P < 0.05). Further significant improvements were found between 6 and 12 (P = 0.002) but not between 12 and 24 months after surgery (Fig. 6). It has to be regarded that all three clinical scores demonstrated a reverse tendency from the 12 months to the 24 months follow-up; however, they were still better than the preoperative measures.
Group II
Daily pain was significantly decreased at 6, 12 and 24 months compared to preoperative status (P < 0.05) (Fig. 2). Concerning subjective knee function, significant improvements could be detected 12 and 24 months after surgery using the Lysholm scoring system compared to preoperative values (P < 0.05). Further significant increase was only found between 6 and 12 (P = 0.043) months after surgery (Fig. 3). The WOMAC score demonstrated significant improvements at 12 and 24 months after surgery (P < 0.05). Further significant improvements were found between 6 and 12 (P = 0.018) months after surgery (Fig. 5). The maximum passive flexion 24 months after surgery showed no significant difference compared to preoperative status.
Radiological evaluation
No loosening of the implant or signs of osteolysis were recorded by the time of data collection for this report (24 months postoperatively). A significant decrease in mean Caton-Dechamps Index could be noticed on postoperative radiographs compared with those taken preoperatively (P = 0.02). Significant increase in tibiofemoral osteoarthritis within the medial but not in the lateral tibiofemoral joint could be assessed (P = 0.011 and n.s. respectively).
Group I
Significant decrease (P = 0.013) of mean Caton-Dechamps Index could be noticed on postoperative radiographs compared with those taken preoperatively. Furthermore significant increase in osteoarthritis within the medial and in the lateral tibiofemoral joint could be assessed (P = 0.034 and P = 0.034 respectively). See Table 2 for details.
Group II
No significant decrease in mean Caton-Dechamps Index could be noticed on postoperative radiographs compared with those taken preoperatively. No further significant differences in the radiological evaluation in this group were found. See Table 2 for details.
Discussion
The most important finding of the present study was an overall significant improvement in all evaluated scores at the 2-year follow-up after patellofemoral arthroplasty performed with the Journey PFJ®. Patients presenting with primary patellofemoral OA (group I) and treated with an isolated procedure showed no further improvement of clinical scores after significant improvement at the 1-year follow-up. However, patients presenting with patellofemoral OA and concomitant PFI (group II) were treated with a combined procedure and showed continuous improvement at 2 years compared to the 1-year follow-up. The Journey PFJ® is designed to be more anatomical due to its asymmetric trochlear groove, which is deepened and lateralized. Individual evaluation of each of the different implants for patellofemoral arthroplasty seems to be of importance since PF implants show significant differences in their anatomical design. Previous authors have published results with different prosthesis and varying follow-up times [2, 3, 7, 16, 23]. A common theme amongst these reports is that isolated patellofemoral arthroplasty demonstrated variable results [2, 3, 7, 16, 17, 22]. Reasons for suboptimal outcomes were seen in implant design, progress of osteoarthritis and specifically degenerations in conjoining parts of the joint (tibiofemoral) [16, 17].
Our study divided patients into two groups based on the causing factors for their patellofemoral OA. Patients were treated according to these factors with a specific focus on restoring physiological and restabilized patellofemoral motion. The instability group (II) showed a steady improvement in clinical scores even at the 24-month follow-up. No data exists on the results of such combined procedures; however, it can be assumed that combined treatments helped these patients to regain PF stability and consequently improved PF motion [1, 6, 9, 11, 13, 27, 28]. Other authors have reported similar improved results in patients with patellofemoral osteoarthritis due to trochlea dysplasia and in cases of realigned patellofemoral instability [2, 3, 7]. In contrast, outcomes in patients treated for primary degenerative patellofemoral OA have been shown to be inferior compared to patients treated for patellofemoral OA due to trochlea dysplasia or soft tissue mal-alignment [2, 4, 16, 17].
Failure of patellofemoral arthroplasty occurs primarily due to malalignment of the implant and progression of tibiofemoral OA [16, 17]. Patients presenting with primary osteoarthritis of the PF joint, not caused by patellofemoral instability, may also have degenerative changes of the other compartments as part of the joint’s osteoarthritic reaction [16]. Comparing the two groups in our study showed significant differences of tibiofemoral OA before and after surgery in group I. This could be seen as an important factor for the stagnation of further clinical improvement in this group. Besides this, a significant decrease in patellar height measured by CD index was observed in group I. Although these changes had no influence on total range of motion in this group, changes of patellar height might result in persisting pain and decreased functionality within a longer follow-up. Additionally one patient was lost to follow-up due to conversion to a total joint after 18 months and has to be regarded as a failure. However, there is still no overall consensus on how to define the clinically important extent of tibiofemoral OA and how to include these findings into the process of surgical indication in middle age patients [25]. This may be a reason explaining why total joint arthroplasty is also considered a treatment option for patellofemoral OA in current literature [14, 17, 22]. However, this option has to be assessed very cautiously, as for the relative young age of these patients and the expected wear of the prostheses [10].
There are several limitations in this study. One has to be seen in the short follow-up only reporting on 2-year data. Despite this, our early reports point to a trend in improving patient outcomes that we believe to be of valuable clinical importance. Furthermore, our sample size in each group was relatively small; however, this is explained by the relative infrequency of patients requiring isolated patellofemoral arthroplasty. Nevertheless, we have sufficient patients to achieve statistical significance as determined by our prestudy power analysis. Though patellofemoral OA as a clinical finding is known to be frequent, it can be tolerated for a prolonged time by the patients since activities of daily living are first limited at a situation of progressed disease. Data presented in this study reflects a limited case series, and further studies with a higher number of cases and a longer follow-up have to be performed to draw final conclusions on the optimal therapy for patellofemoral OA [26]. No overall consensus exists on treatment of patellofemoral OA and especially in patients with additional signs of PFI. The algorithm for surgical treatment used in this study is therefore subject to discussion. However, it reflects the authors’ current clinical practice and is based on current literature [1, 6, 13, 27, 29]. An additional limitation of this study is the lack of a non-operative control group. This would have strengthened the study; however, the included patients demonstrated symptomatic progressive patellofemoral OA and already failed conservative treatment options.
The clinical relevance of the present study is that patellofemoral arthroplasty may be an effective procedure for the treatment of isolated patellofemoral OA. Patients should be chosen carefully, additional signs of PFI should be regarded, and if necessary, procedures for stabilizing the patella added. However, more prospective studies are needed to estimate the long-term outcome of current implants.
Conclusion
Patellofemoral arthroplasty using the Journey® PFJ for treatment of significant patellofemoral OA demonstrated improved clinical scores at the 2-year follow-up in both groups. Comparing the primary OA (I) and OA + instability (II) group, patients with patellofemoral OA treated with a combined procedure for concomitant stabilization of patellofemoral instability may benefit more from such a combined procedure, than patients treated with an isolated procedure for treatment of isolated patellofemoral OA.
References
Amis AA (2007) Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc 15(2):48–56
Arciero RA, Toomey HE (1988) Patellofemoral arthroplasty. A three- to nine-year follow-up study. Clin Orthop Relat Res 236:60–71
Argenson JN, Flecher X, Parratte S, Aubaniac JM (2005) Patellofemoral arthroplasty: an update. Clin Orthop Relat Res 440:50–53
Argenson JN, Guillaume JM, Aubaniac JM (1995) Is there a place for patellofemoral arthroplasty? Clin Orthop Relat Res 321:162–167
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15(12):1833–1840
Biedert RM (2008) Osteotomies. Orthopade 37(9):872, 874–876, 878–880
Cartier P, Sanouiller JL, Khefacha A (2005) Long-term results with the first patellofemoral prosthesis. Clin Orthop Relat Res 436:47–54
Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H (1982) Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot 68(5):317–325
Colvin AC, West RV (2008) Patellar instability. J Bone Joint Surg Am 90(12):2751–2762
Dahm DL, Al-Rayashi W, Dajani K, Shah JP, Levy BA, Stuart MJ (2010) Patellofemoral arthroplasty versus total knee arthroplasty in patients with isolated patellofemoral osteoarthritis. Am J Orthop (Belle Mead NJ) 39(10):487–491
Dejour D, Le Coultre B (2007) Osteotomies in patello-femoral instabilities. Sports Med Arthrosc 15(1):39–46
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S (2010) Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med 38(2):323–329
Fulkerson JP (2007) The effects of medialization and anteromedialization of the tibial tubercle on patellofemoral mechanics and kinematics. Am J Sports Med 35(1):147 (author reply 148)
Grelsamer RP, Stein DA (2006) Patellofemoral arthritis. J Bone Joint Surg Am 88(8):1849–1860
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Leadbetter WB (2008) Patellofemoral arthroplasty in the treatment of patellofemoral arthritis: rationale and outcomes in younger patients. Orthop Clin North Am 39(3):363–380, vii
Leadbetter WB, Seyler TM, Ragland PS, Mont MA (2006) Indications, contraindications, and pitfalls of patellofemoral arthroplasty. J Bone Joint Surg Am 88(Suppl 4):122–137
Lustig S, Magnussen RA, Dahm DL, Parker D (2012) Patellofemoral arthroplasty, where are we today? Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-1948-z
Lustig S, Servien E, Biedert R, Neyret P (2008) Isolated arthrosis of the patellofemoral joint in younger patients (<50 years). Orthopade 37(9):848, 850–842, 854–847
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154
McKeever DC (1955) Patellar prosthesis. J Bone Joint Surg Am 37(5):1074–1084
Mihalko WM, Boachie-Adjei Y, Spang JT, Fulkerson JP, Arendt EA, Saleh KJ (2007) Controversies and techniques in the surgical management of patellofemoral arthritis. J Bone Joint Surg Am 89(12):2788–2802
Mihalko WM, Boachie-Adjei Y, Spang JT, Fulkerson JP, Arendt EA, Saleh KJ (2008) Controversies and techniques in the surgical management of patellofemoral arthritis. Instr Course Lect 57:365–380
Munoz-Mahamud E, Popescu D, Nunez E, Lozano LM, Nunez M, Sastre S, Torner P, Segur JM, Macule F (2011) Secondary patellar resurfacing in the treatment of patellofemoral pain after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(9):1467–1472
Nicol SG, Loveridge JM, Weale AE, Ackroyd CE, Newman JH (2006) Arthritis progression after patellofemoral joint replacement. Knee 13(4):290–295
Odumenya M, McGuinness K, Achten J, Parsons N, Spalding T, Costa M (2011) The Warwick patellofemoral arthroplasty trial: a randomised clinical trial of total knee arthroplasty versus patellofemoral arthroplasty in patients with severe arthritis of the patellofemoral joint. BMC Musculoskelet Disord 12:265
Schottle P, Schmeling A, Romero J, Weiler A (2009) Anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 129(3):305–309
Schottle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J (2005) Trochleaplasty for patellar instability due to trochlear dysplasia: a minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop 76(5):693–698
Seitlinger G, Beitzel K, Scheurecker G, Imhoff A, Hofmann S (2011) The painful patellofemoral joint. Biomechanics, diagnosis and therapy. Orthopade 40(4):353–368; quiz 369–370
Acknowledgment
The authors would like to thank Tibor Schuster, statistician at the Institute of Medical Statistics and Epidemiology, Technische Universität München, Munich, Germany, for his statistical advice.
Conflict of interest
The Department of Orthopedic Sports Medicine received funding from Smith & Nephew (Smith & Nephew, Andover, MA, USA). The company had no influence on study design, data collection and interpretation of the results or the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beitzel, K., Schöttle, P.B., Cotic, M. et al. Prospective clinical and radiological two-year results after patellofemoral arthroplasty using an implant with an asymmetric trochlea design. Knee Surg Sports Traumatol Arthrosc 21, 332–339 (2013). https://doi.org/10.1007/s00167-012-2022-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-2022-6