Abstract
Purpose
Because of the multiple possible aetiologies of painful total knee arthroplasty (TKA), the diagnosis and treatment of such patients are challenging. In a considerable number of patients, an intraarticular pathology is present, although not verifiable with clinical and diagnostic imaging techniques as in cases of primary arthrofibrosis. In these patients, the differentiation between intra- and extraarticular causes of pain remains difficult. Until now, little attention has been paid to changes of the synovial fluid and tissue in these knees. The objective of this study was to analyse the changes of the synovial environment in patients suffering from arthrofibrosis after TKA in comparison with knees with referred pain suffering from hip arthritis. The changes of the synovial environment probably provide additional diagnostic information to verify an intraarticular pathology.
Methods
The synovial fluid of 10 consecutive knees in 10 patients presenting with a primary arthrofibrosis after TKA without signs of infection, instability, malalignment, or loosening was analysed and compared to the synovial fluid of 10 knees with referred pain serving as controls. The BMP-2 concentration was measured in the synovial fluid, and the presence of cytokines leading to an overexpression of BMP-2 was detected by measuring the change of BMP-2 expression in a synoviocyte cell line following exposing to the synovial fluid of the patients.
Results
The concentration of BMP-2 in the synovial fluid was significantly higher in arthrofibrotic TKA knees (24.3 ± 6.9 pg/mL), compared with the control group 5.9 ± 4.8 pg/mL (P < 0.001). Corresponding to this finding, BMP-2 expression in synoviocytes was upregulated 11.5-fold (P < 0.05) by synovial fluid of patients suffering from arthrofibrosis after TKA, compared with the control group with referred pain.
Conclusion
BMP-2 is overexpressed and its concentrations are consequently higher in patients suffering from arthrofibrosis after TKA. The synovial BMP-2 concentration may be a potential marker for differentiating between intra- and extraarticular causes of pain.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The past decades have brought continuous improvement in total knee arthroplasty (TKA). More sophisticated surgical techniques as well as new implant designs have led to more satisfactory outcomes [4, 26, 36]. However, the diagnosis of painful TKA continues to be a challenge, due to its multiple possible origins [43, 44]. The diagnostic algorithm includes different non-invasive and invasive examinations of the knee joint (e.g. X-ray, computed tomography, aspiration, arthroscopy). Therefore, causes of pain not related to the knee joint should be excluded first. The most common causes are spinal stenosis, coxalgia, neuroma, vascular diseases, and psychosomatic diseases [1, 6, 9, 13, 21, 24, 25, 27, 32, 33, 38]. Despite a knowledge of biological and mechanical causes of intraarticular cause of pain (e.g. infection, instability, loosening, malalignment, arthrofibrosis, allergy), the origin sometimes remains difficult to determine with clinical and diagnostic imaging techniques [44]. Especially the diagnosis of primary arthrofibrosis is due to its indistinct aetiology often confirmed only clinically. Although the differentiation between extra- and intraarticular causes of knee pain is crucial, appropriate diagnostic tools have not been available up to now. Treatment options of primary arthrofibrosis after TKA are physical therapy, manipulation under anaesthesia, arthroscopy or open arthrolysis [2, 10, 18]. These procedures mostly achieve an improvement in range of motion, but randomized studies regarding the outcome are missing [10, 18].
Transforming growth factor-ß (TGF-ß) plays a key role in the pathogenesis of arthrofibrosis due to an increased inflammatory reaction [11, 12, 48]. Bone morphogenetic protein 2 (BMP-2) is a low molecular weight glycoprotein that belongs to the TGF-β protein superfamily. It has versatile functions, like skeletal organogenesis, osteoinduction, and regeneration [35]. Of particular relevance to the present study hypothesis, BMP-2 is also known to be responsible for increased inflammatory tissue reactions [37, 50]. Several clinical reports have described excessive inflammatory reactions with long-lasting pain after vertebral fusion and application of BMP-2 [14, 30, 37]. The close connection between chronic painful inflammation and changes of the synovial tissue and fluid is well accepted in the pathogenesis of osteoarthritis and rheumatoid arthritis [16, 23, 42, 47].
In contrast to this, extraarticular diseases do not alter the synovial environment of the knee joint.
It seems plausible that changes in the synovial fluid identified as being typical for arthrofibrosis after TKA would be of diagnostic value. The hypothesis of this study was that patients suffering from primary arthrofibrosis after TKA present increased levels of inflammatory procytokines and cytokines in the synovial fluid.
Materials and methods
Patients with a painful knee of intra- or extraarticular origins were included in this comparative study. The study protocol was approved by the institutional review board, and all patients gave their informed consent. Clinical patient data were documented for each patient, including age, gender, side and time since implantation.
There is no consensus in the literature for a consistent definition of arthrofibrosis after TKA [39]. In our study, arthrofibrosis was defined as painful limitation of range of motion less than 90° including an extension deficit of more than 10° according to the classification of Yercan et al. [49]. Regarding pain inclusion criteria were persistent pain of more than 6 months’ duration after primary TKA and intensity of rest pain >5 on a visual analogue scale (VAS) and pain >7 under weight-bearing conditions on the VAS.
All knees showing signs of infection, loosening, instability, impingement, or malalignment were excluded.
Patients awaiting total hip replacement and with knee pain related to their hip pathology for more than 6 months were included in the group with an extraarticular cause of pain (group B). All patients in group B underwent radiographic examination of the involved knee. Patients suffering from osteoarthritis of this joint were excluded (defined as radiographic changes exceeding stadium 1 according to Kellgren and Lawrence).
Aspiration was performed in all knees once during the study and a minimum of 5 mL of synovial fluid was immediately cryoconserved and stored at −20°C until examination. The concentration of bone morphogenetic protein (BMP-2), as part of the TGF-β protein superfamily that plays a key role in the pathogenesis of arthrofibrosis [11, 12, 48], was measured with an ELISA.
BMP-2 ELISA
The concentration of BMP-2 was analysed in the synovial fluid of all knees with the “Quantikine BMP-2 Immunoassay Kit” according to the manufacturer’s protocol (R&D systems, Minnesota, USA). This assay works with a quantitative sandwich enzyme immunoassay technique. Extinction was measured in a microplate reader at a wavelength of 450 nm.
Gene expression analysis (rtPCR)
In order to detect all cytokines maintaining a vicious circle of inflammation, resulting in a change of BMP-2 concentration in the synovial fluid, a part of the aspirates was added to a synovial cell line and the change of BMP-2 mRNA expression pattern was determined.
Cell culture was done with immortalized human synovial cells (SW-982) deriving from a synovial sarcoma purchased from the American Type Culture Collection (Bethesda, MD) [8]. The synovial cells were cultured with Dulbecco’s modified Eagle’s medium (DMEM) (Gibco, Grand Island, NY) supplemented with 10% foetal calf serum (FCS) (Biochrom AG, Berlin) and 100 U/mL penicillin plus 100 lg/mL streptomycin (Expansion medium, EM). Cells were passaged at 70–80% confluence, and passages 10–15 were used for experiments [22]. Cells were incubated in a humidified incubator at 37°C and 5% CO2. For the experiments, 1.7 × 105 cells were seeded in 25 cm2 plastic flasks. After cell adherence, 2 mL of synovial fluid were added to the culture flasks and incubated for 48 h. The cells were then washed and immediately harvested for gene expression analysis.
Total RNA was isolated with the “RNeasy Mini Kit” (Qiagen, Maryland, USA). Digestion of residual amounts of DNA was performed with an additional step in the isolation procedure with the “RNAse-free DNAse Set” (Qiagen, Maryland, USA). One microgram of RNA of each sample was reversed transcribed using the “RT2 First Strand Kit” (SA Biosciences, Maryland, USA) [34]. For gene profiling, samples were applied to 384-well “RT2-Profiler PCR Array” plates for human inflammatory response and autoimmunity (SA Biosciences, Maryland, USA). PCR was performed in an Applied Biosystems ABI 7900 HT fast real-time PCR system with a 384-well block. A standard curve and an end-time dissociation curve were done for each plate, baseline and threshold cycles being detected automatically.
For comparison of the data between the plates, a baseline of 0.3 and threshold cycles from 2 to 10 were defined. Data were analysed by using the ΔΔ-CT method [29]. This mathematical method relates the PCR signal of the target gene (BMP-2) of group A to the signal of the target gene of group B. This allows a relative comparison of both groups.
The ELISA and rtPCR measurements are well-established methods and were performed according to the manufacturers’ instructions, so that neither a test–retest reliability nor a test of inter-observer variation was determined.
Statistical analysis
Descriptive statistics (mean, minimum, maximum, and standard deviations) were calculated from the measured data.
Statistical analysis of the PCR data between the samples was performed with the ΔΔ-CT method [29]. The Mann–Whitney U test was used for nonparametrically unmatched correlation analysis between the groups, and the Wilcoxon Test for nonparametrically matched samples. P = 0.05 was defined as the level of significance.
Results
The mean age of the patients was comparable between group A (70.2 ± 9.1 years) and group B (66.8 ± 12.3 years, n.s.). Five men and 5 women patients were included in each group. The ratio between left and right knees was 8/2 in group A and 7/3 in group B. The average time since implantation of the TKA in group A was 23 ± 16 months.
BMP-2 ELISA
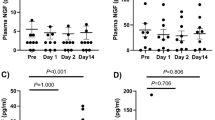
The BMP-2 concentration in the synovial fluid of group A knees was 24.3 ± 6.9 pg/mL. In contrast, group B knees presented a significantly lower BMP-2 concentration of just 5.9 ± 4.9 pg/mL (P < 0.001) (Fig. 1).
Gene expression analysis (rt-PCR)
The Ct value of BMP-2 of the native synoviocytes before addition of synovial fluid was 30.0 ± 4.2. In contrast, the Ct value was significantly reduced in group A to 27.7 ± 3.9 (P < 0.05). The synovial fluid of group B knees did not change the Ct value (31.4 ± 1.0). These values correspond to a 11.5 ± 0.1-fold expression of BMP-2 in group A knees compared with group B knees (P < 0.05) (Fig. 2).
Discussion
The most important finding of the present study was that BMP-2 concentration in the synovial fluid is significantly increased in patients suffering from arthrofibrosis after TKA, compared to patients with knee pain related to extraarticular factors. It could also be shown that the addition of synovial fluid to a synoviocyte cell line led to increased BMP-2 mRNA expression. This finding demonstrates that the increased BMP-2 concentration in arthrofibrotic knees after TKA resulted from cytokines in the synovial fluid following changes of the synovial tissue.
The aetiology of arthrofibrosis is still mostly indistinct. Factors like comorbidities, preoperative knee function, molecular factors (e.g. mast cell proliferation), surgical approach, and ineffective postoperative pain management are described [11, 20, 28, 39]. A pathologic immune response with the following chronic inflammation is also discussed [3]. Freeman et al. [12] showed an increased infiltration of inflammatory cells in arthrofibrosis. The normal resolution of the inflammatory reaction in tissue repair fails resulting in a persistent inflammation of the synovial tissue. Furthermore, a dysregulation on cytokine level seems to be present. Beside inflammatory cytokines (TNF-α, IL-1 and IL-6), there is an upregulation of TGF-β- and platelet-derived growth factor (PDGF), triggering an irreversible tissue fibrosis via the transformation of fibroblasts [48, 51].
BMP-2 is part of the same protein superfamily as TGF-β and may therefore be upregulated in arthrofibrosis, too. BMP-2 is an important factor in this multifactorial aetiology, but to our knowledge, it was not described as independent factor in the pathogenesis of arthrofibrosis until now.
Schmal et al. [40] investigated the BMP-2 levels in painful knees with intraarticular cause of pain (cartilage defect) and found even higher levels in comparison with our data that were not correlated to the pain level. This fortifies our hypothesis that increased BMP-2 levels are present in intraarticular causes of pain. Moreover, BMP-2 stimulates the expression of neurofilaments in peripheral nerves [7, 45, 46], which is similar to a treatment with nerve growth factor (NGF) [19]. BMP-2 is also an important cofactor of tumour necrosis factor (TNF-α) in peripheral nerve regeneration and nociception. Together with TNF-α, it stimulates the production of NGF in fibroblasts [17]. Some studies have shown that NGF is expressed in various inflammatory cells and is a potent mediator of pain and inflammation [5, 31, 52]. The authors concluded that the NGF system plays a key role in chronic and inflammatory pain response [5]. Upregulation of BMP-2 may therefore contribute to the pathogenesis of chronic pain via NGF.
This study is limited by the fact that the knee joints in the group of extraarticular cause of pain were non-replaced and only referred from hip pathology. Another limitation is that no allergy test was performed in the patients of group A. The role of allergy as an evident cause of pain after TKA is still indistinct. Degradation products of metal or acrylic cements are able to interact with the immune system and may induce a delay-type hypersensitivity reaction [15]. But there is still no evidence whether this causes persistent pain and implant failure in these patients [15, 41]. Schuh et al. [41] found a large amount of patients with allergy to implant metal and arthroplasty which were completely asymptomatic.
Conclusion
The synovial BMP-2 concentration could be a new and helpful tool in the differential diagnosis of painful total knee arthroplasty pointing the focus of further investigations on primary arthrofibrosis.
References
Beltran LS, Bencardino J, Ghazikhanian V, Beltran J (2010) Entrapment neuropathies III: lower limb. Semin Musculoskelet Radiol 14(5):501–511
Bonutti PM, Marulanda GA, McGrath MS, Mont MA, Zywiel MG (2010) Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 18(2):194–199
Bosch U (2002) Arthrofibrosis. Orthopade 31(8):785–790
Boulos K, Jolles-Haeberli BM (2008) Total knee arthroplasty today: what should we tell our patients? Rev Med Suisse 4(184):2737–2742
Capsoni S, Covaceuszach S, Marinelli S, Ceci M, Bernardo A, Minghetti L, Ugolini G, Pavone F, Cattaneo A (2011) Taking pain out of NGF: a “painless” NGF mutant, linked to hereditary sensory autonomic neuropathy type V, with full neurotrophic activity. PLoS One 6(2):e17321
Celis R, Pipinos II, Scott-Pandorf MM, Myers SA, Stergiou N, Johanning JM (2009) Peripheral arterial disease affects kinematics during walking. J Vasc Surg 49(1):127–132
Chalazonitis A, D’Autreaux F, Guha U, Pham TD, Faure C, Chen JJ, Roman D, Kan L, Rothman TP, Kessler JA, Gershon MD (2004) Bone morphogenetic protein-2 and -4 limit the number of enteric neurons but promote development of a TrkC-expressing neurotrophin-3-dependent subset. J Neurosci 24(17):4266–4282
Christensen BN, Kochukov M, McNearney TA, Taglialatela G, Westlund KN (2005) Proton-sensing G protein-coupled receptor mobilizes calcium in human synovial cells. Am J Physiol Cell Physiol 289(3):C601–C608
Ducic I, Levin M, Larson EE, Al-Attar A (2010) Management of chronic leg and knee pain following surgery or trauma related to saphenous nerve and knee neuromata. Ann Plast Surg 64(1):35–40
Fitzsimmons SE, Vazquez EA, Bronson MJ (2010) How to treat the stiff total knee arthroplasty?: a systematic review. Clin Orthop Relat Res 468:1096–1106
Freeman TA, Parvizi J, Dela Valle CJ, Steinbeck MJ (2010) Mast cells and hypoxia drive tissue metaplasia and heterotopic ossification in idiopathic arthrofibrosis after total knee arthroplasty. Fibrogenesis Tissue Repair 3:17
Freeman TA, Parvizi J, Della Valle CJ, Steinbeck MJ (2009) Reactive oxygen and nitrogen species induce protein and DNA modifications driving arthrofibrosis following total knee arthroplasty. Fibrogenesis Tissue Repair 2(1):5
Gao Y, Chen S, Yu C, Nie Z (2010) Endovascular treatment of multilevel arteriosclerosis obliterans of lower extremities. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 24(9):1033–1036
Garrett MP, Kakarla UK, Porter RW, Sonntag VK (2010) Formation of painful seroma and edema after the use of recombinant human bone morphogenetic protein-2 in posterolateral lumbar spine fusions. Neurosurgery 66(6):1044–1049
Granchi D, Cenni E, Tigani D, Trisolino G, Baldini N, Giunti A (2008) Sensitivity to implant materials in patients with total knee arthroplasties. Biomaterials 29(10):1494–1500
Haringman JJ, Kraan MC, Smeets TJ, Zwinderman KH, Tak PP (2003) Chemokine blockade and chronic inflammatory disease: proof of concept in patients with rheumatoid arthritis. Ann Rheum Dis 62(8):715–721
Hattorl A, Tsujimoto M, Hayashi K, Kohno M (1996) Bone morphogenetic protein-2 is markedly synergistic with tumor necrosis factor in stimulating the production of nerve growth factor in fibroblasts. Biochem Mol Biol Int 38(6):1095–1101
Ipach I, Mittag F, Lahrmann J, Kunze B, Kluba T (2011) Arthrofibrosis after TKA-Influence factors on the absolute flexion and gain in flexion after manipulation under anaesthesia. BMC Musculoskelet Disord 12:184
Iwasaki S, Hattori A, Sato M, Tsujimoto M, Kohno M (1996) Characterization of the bone morphogenetic protein-2 as a neurotrophic factor. Induction of neuronal differentiation of PC12 cells in the absence of mitogen-activated protein kinase activation. J Biol Chem 271(29):17360–17365
Jackson G, Waldman BJ, Schaftel EA (2008) Complications following quadriceps-sparing total knee arthroplasty. Orthopedics 31(6):547
Kachar SM, Williams KM, Finn HA (2008) Neuroma of the infrapatellar branch of the saphenous nerve a cause of reversible knee stiffness after total knee arthroplasty. J Arthroplasty 23(6):927–930
Kasper G, Dankert N, Tuischer J, Hoeft M, Gaber T, Glaeser JD, Zander D, Tschirschmann M, Thompson M, Matziolis G, Duda GN (2007) Mesenchymal stem cells regulate angiogenesis according to their mechanical environment. Stem Cells 25(4):903–910
Kennedy A, Ng CT, Chang TC, Biniecka M, O’Sullivan JN, Heffernan E, Fearon U, Veale DJ (2011) Tumor necrosis factor blocking therapy alters joint inflammation and hypoxia. Arthritis Rheum 63(4):923–932
Khan AM, McLoughlin E, Giannakas K, Hutchinson C, Andrew JG (2004) Hip osteoarthritis: where is the pain? Ann R Coll Surg Engl 86(2):119–121
Kindler LL, Bennett RM, Jones KD (2011) Central sensitivity syndromes: mounting pathophysiologic evidence to link fibromyalgia with other common chronic pain disorders. Pain Manag Nurs 12(1):15–24
Knutson K, Robertsson O (2010) The Swedish knee arthroplasty register. Acta Orthop 81(1):5–7
Kosashvili Y, Fridman T, Backstein D, Safir O, Bar Ziv Y (2008) The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int 29(9):910–913
Lavernia C, Cardona D, Rossi MD, Lee D (2008) Multimodal pain management and arthrofibrosis. J Arthroplasty 23(6 Suppl 1):74–79
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25(4):402–408
Muchow RD, Hsu WK, Anderson PA (2010) Histopathologic inflammatory response induced by recombinant bone morphogenetic protein-2 causing radiculopathy after transforaminal lumbar interbody fusion. Spine J 10(9):e1–e6
Ochodnicky P, Cruz CD, Yoshimura N, Michel MC (2011) Nerve growth factor in bladder dysfunction: contributing factor, biomarker, and therapeutic target. Neurourol Urodyn 30(7):1227–1241
Palmer KT, Calnan M, Wainwright D, Poole J, O’Neill C, Winterbottom A, Watkins C, Coggon D (2005) Disabling musculoskeletal pain and its relation to somatization: a community-based postal survey. Occup Med (Lond) 55(8):612–617
Peck D (2010) Slipped capital femoral epiphysis: diagnosis and management. Am Fam Physician 82(3):258–262
Rafei M, Campeau PM, Wu JH, Birman E, Forner K, Boivin MN, Galipeau J (2009) Selective inhibition of CCR2 expressing lymphomyeloid cells in experimental autoimmune encephalomyelitis by a GM-CSF-MCP1 fusokine. J Immunol 182(5):2620–2627
Riley EH, Lane JM, Urist MR, Lyons KM, Lieberman JR (1996) Bone morphogenetic protein-2: biology and applications. Clin Orthop Relat Res 324:39–46
Robertsson O, Bizjajeva S, Fenstad AM, Furnes O, Lidgren L, Mehnert F, Odgaard A, Pedersen AB, Havelin LI (2010) Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop 81(1):82–89
Robin BN, Chaput CD, Zeitouni S, Rahm MD, Zerris VA, Sampson HW (2010) Cytokine-mediated inflammatory reaction following posterior cervical decompression and fusion associated with recombinant human bone morphogenetic protein-2: a case study. Spine (Phila Pa 1976) 35(23):E1350–E1354
Ross MD, Elliott R (2010) Cervical cord compressive myelopathy in a man with a primary complaint of knee pain. J Spinal Cord Med 33(4):431–434
Schiavone Panni A, Cerciello S, Vasso M, Tartarone M (2009) Stiffness in total knee arthroplasty. J Orthop Traumatol 10(3):111–118
Schmal H, Niemeyer P, Sudkamp NP, Gerlach U, Dovi-Akue D, Mehlhorn AT (2011) Pain perception in knees with circumscribed cartilage lesions is associated with intra-articular IGF-1 expression. Am J Sports Med 39(9):1989–1996
Schuh A, Lill C, Honle W, Effenberger H (2008) Prevalence of allergic reactions to implant materials in total hip and knee arthroplasty. Zentralbl Chir 133(3):292–296
Smeets TJ, Barg EC, Kraan MC, Smith MD, Breedveld FC, Tak PP (2003) Analysis of the cell infiltrate and expression of proinflammatory cytokines and matrix metalloproteinases in arthroscopic synovial biopsies: comparison with synovial samples from patients with end stage, destructive rheumatoid arthritis. Ann Rheum Dis 62(7):635–638
Sun Z, Liu J, Wang P (2010) Research development of diagnosis and treatment of pain after total knee arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 24(6):708–713
Toms AD, Mandalia V, Haigh R, Hopwood B (2009) The management of patients with painful total knee replacement. J Bone Joint Surg Br 91(2):143–150
Tsujii M, Akeda K, Iino T, Uchida A (2009) Are BMPs involved in normal nerve and following transection?: a pilot study. Clin Orthop Relat Res 467:3183–3189
Wang YL, Wang DZ, Nie X, Lei DL, Liu YP, Zhang YJ, Suwa F, Tamada Y, Fang YR, Jin Y (2007) The role of bone morphogenetic protein-2 in vivo in regeneration of peripheral nerves. Br J Oral Maxillofac Surg 45(3):197–202
Wassilew GI, Lehnigk U, Duda GN, Taylor WR, Matziolis G, Dynybil C (2010) The expression of proinflammatory cytokines and matrix metalloproteinases in the synovial membranes of patients with osteoarthritis compared with traumatic knee disorders. Arthroscopy 26(8):1096–1104
Watson RS, Gouze E, Levings PP, Bush ML, Kay JD, Jorgensen MS, Dacanay EA, Reith JW, Wright TW, Ghivizzani SC (2010) Gene delivery of TGF-beta1 induces arthrofibrosis and chondrometaplasia of synovium in vivo. Lab Invest 90(11):1615–1627
Yercan HS, Sugun TS, Bussiere C, Ait Si Selmi T, Davies A, Neyret P (2006) Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee 13(2):111–117
Zara JN, Siu RK, Zhang X, Shen J, Ngo R, Lee M, Li W, Chiang M, Chung J, Kwak J, Wu BM, Ting K, Soo C (2011) High doses of bone morphogenetic protein 2 induce structurally abnormal bone and inflammation in vivo. Tissue Eng Part A 17(9–10):1389–1399
Zeichen J, Gerich T, Lobenhoffer P, Bosch U (1998) Intrinsic properties of arthrofibrosis tissue: histologic and cell biology analysis. Langenbecks Arch Chir Suppl Kongressbd 115(Suppl I):189–191
Zhu Y, Colak T, Shenoy M, Liu L, Pai R, Li C, Mehta K, Pasricha PJ (2011) Nerve growth factor modulates TRPV1 expression and function and mediates pain in chronic pancreatitis. Gastroenterology 141(1):370–377
Conflict of interest
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pfitzner, T., Geissler, S., Duda, G. et al. Increased BMP expression in arthrofibrosis after TKA. Knee Surg Sports Traumatol Arthrosc 20, 1803–1808 (2012). https://doi.org/10.1007/s00167-011-1774-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1774-8