Abstract
Purpose
Knee pain and disability can persist following knee replacement surgery which may place patients at increased risk of falls. This study investigated the falls risk and the occurrence of falls of people with knee osteoarthritis (OA) before and at 12 months following knee replacement surgery.
Method
Thirty-five patients with knee OA were tested prior to undergoing knee replacement surgery and at 12 months following surgery using the short form Physiological Profile Assessment, which incorporates tests of vision, lower limb proprioception, knee extension strength, reaction time and postural sway. Physical activity, number of falls, fear of falling, pain, disability and health-related quality of life were also assessed.
Results
No significant differences were found between the number of falls pre- and post-surgery (n.s.), with 48.5 and 40% reporting at least one fall in the 12 months before and following the surgery, respectively. Improvements in knee strength, reaction time and fear of falling were evident following surgery, with no improvement in lower limb proprioception. Self-reported pain, function and stiffness were significantly improved, but health-related quality of life deteriorated following the surgery.
Conclusion
The number of falls experienced following knee replacement surgery remained relatively high, which may be attributed to the persistence of impaired lower limb proprioception. Although knee replacement surgery improves function and alleviates pain, people who undergo this procedure may need to engage in rehabilitation following the surgery to reduce the risk of falling.
Level of evidence
Therapeutic study investigating the result of treatment on patient outcomes, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (OA) is a painful, chronic degenerative joint disorder affecting a large portion of the older population worldwide [26, 40]. Moreover, recent studies have shown that chronic pain and musculoskeletal conditions, including knee OA, are independent risk factors for falls [18–20, 34] with approximately 50% of people with knee OA reporting one or more falls each year [21, 38]. There is growing evidence to suggest that pain and the neuromuscular deficits (in strength, balance and proprioception) associated with OA contribute to the increase risk of falling in this population [10, 19, 20, 31].
Total knee replacement is a common surgical treatment for severe knee OA, with over 40,000 procedures performed each year in Australia [1]. Although knee replacement generally improves physical function and quality of life [7, 13], pain and disability can persist following surgery [2, 4]. Moreover, weakness of the knee extensors and impaired proprioception following knee replacement surgery [12] have been also reported, which can negatively affect functional performance [27, 28, 36, 37] and may consequently place people at greater risk of falls following surgery.
Recently, we assessed the risk of falls of patients who underwent knee replacement surgery before and at 4 months following the surgery using the Physiological Profile Assessment tool (PPA), which includes clinical tests of balance, strength, proprioception, vision and reaction time [21]. At 4 months following the surgery, participants exhibited deficits in knee extension strength and lower limb proprioception, which may place them at increased risk of falls early following the surgery. However, little is known about the occurrence of falls and risk factors for falls in people following knee replacement over a longer period. A recent prospective observational study reported a significant reduction in the number of falls in the first, second and fourth post-operative quarters of the first year following the surgery compared to the pre-operation quarter [35]. Assessment of physiological risk factors such as strength and balance 12 months following the surgery, however, was not investigated.
The purpose of this study, therefore, was to investigate the falls risk and the occurrence of falls of people with knee OA before and at 12 months following knee replacement surgery. Specifically, we compared balance, strength, proprioception and vision, fear of falls, quality of life and physical activity before and at 12 months following the surgery. We hypothesised that the falls risk and the occurrence of falls would be reduced after knee replacement surgery.
Materials and methods
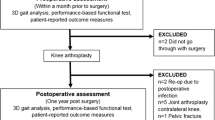
This project was part of a larger study that investigated gait (swing phase mechanics particularly minimum foot clearance), balance and falls risk in people before and after knee replacement. A power calculation to determine the sample size, therefore, was based on minimum foot clearance parameters. At the time of the study design, only limited published results were available on minimum toe clearance or the falls risk of patients with knee OA, and therefore the data from a previous study [6] which investigated the toe clearance of elderly fallers and non-fallers were used to determine the number of participants required. A sample size calculation indicated that for 80% power and a P value of 0.05 at least 25 participants were required. To mitigate the possible effect of subject drop out, a total of 35 participants for each group were considered to be sufficient.
Thirty-five patients (16 females and 19 males) who were scheduled for knee replacement surgery participated in the study [21] and were tested prior to the surgery and at 12 months following their surgery. Mean ± SD age, height, mass and body mass index of the participants were: 67.4 ± 7.3 years, 167.4 ± 8.6 cm, 84.9 ± 12.3 kg and 30.4 ± 4.9 kg/m2. To be included in the study, participants from the surgical group needed to be able to walk at least 45 metres independently and were excluded if they had uncontrolled systemic disease or a pre-existing neurological or other orthopaedic condition affecting their ability to walk. Participants were recruited from the La Trobe University Medical Centre, the Warringal Private Medical Centre and from an outpatient physiotherapy clinic. Patients who were scheduled for knee replacement surgery were informed about the study by the receptionists or the physiotherapists at the clinic. Patients who were willing to participate were contacted by the researchers. Patients were then screened over the phone to identify if they were eligible to take part in the project. Those who met the inclusion criteria were scheduled time for testing at the gait laboratory of the Musculoskeletal Research Centre, La Trobe University. Ethics approval was obtained from the Faculty of Health Sciences Human Ethics Committee, La Trobe University. All participants were informed about the nature of the study and signed a consent form prior to participation.
Measurements
Quality of life
Quality of life was measured using the self-administered Assessment of Quality of Life (AQoL) utility instrument, which assesses quality of life over five domains including illness, independent living, social relationships, physical senses and psychological well-being [14]. The utility scores for each dimension and an overall utility score range from 0 to 1, with 0 representing the worst health and 1 representing perfect health.
Knee pain and function
Physical function, pain and stiffness were assessed using the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) [3]. This index assesses the severity of the knee pain during 5 daily activities (range 0–500), stiffness (range 0–200) and the severity of impairment of lower-extremity function during 17 activities (0–1,700). The items were scored with the use of a 10 mm visual analogue scale, where 0 represents no pain or difficulty with physical function and higher scores represent worse functional health. All three subcategories are summed to give a global WOMAC score (range 0–2,400).
Physical activity questionnaire
The Incidental and Planned Activity Questionnaire (IPAQ) for older people was used to assess the physical activity level of the participants [8]. The IPAQ includes 10 questions that estimate the physical activity during the last week and covers the frequency and duration of planned activity (planned exercise and walks) and incidental activities (casual day-to-day activities). The score was derived from multiplying the frequency score and duration score to create a total duration for incidental and planned activity as well as an overall total score. Total time spent was summed across all components and expressed as hours per week as detailed in Delbaere et al. [8].
Fear of falling
The Short Falls Efficacy Scale International (FES-I) questionnaire was used to document fear of falling [16]. The FES-I consists of 7 items on Likert scale that score the participant’s level of concern regarding the possibility of falling when performing certain daily activities as follows: (1) when getting dressed or undressed, (2) taking a bath, (3) getting in or out of a chair, (4) going up or down stairs, (5) reaching for something above your head or on the ground, (6) walking up or down slop and (7) getting out to a social event. The total score ranges from 7 (not concerned) to 28 (severe concern) [16].
Falls history
The number of falls the participants experienced in the 12 months prior to surgery was recorded. Moreover, participants were requested to record any falls experienced during the 12 months following the surgery using a specialised monthly diary. Participants were asked to record any falls incidence on the monthly diary, and at the end of each month, participants return the diary to the researchers. If the participant sustained a fall, they were asked a series of questions regarding the severity and circumstances surrounding the fall.
Falls risk assessment
The short form of the PPA was used to assess falls risk and includes 5 tests (Fig. 1): vision (edge contrast sensitivity), peripheral sensation (a lower limb matching task for determining proprioception), lower limb strength (knee extension), reaction time and balance (postural sway when standing on a medium density foam rubber mat) [24]. The PPA is a validated and reliable tool [24] and has been demonstrated to have a predictive accuracy of 75% for prospectively documented falls in older people [22, 25]. The PPA uses a discriminant function to compute a standardised falls risk score. The level of falls risk according to the overall falls risk score was classified as follows: <0—low risk, 0–1—mild risk, 1–2—moderate risk and >2—high risk [24].
The individual tests of the PPA were performed as follows: (1) visual contrast sensitivity was assessed using the Melbourne Edge Test. The chart had 20 circular 25-mm-diameter patches containing edges with reducing contrast with variable orientation as the identifying feature. The lowest contrast patch correctly identified was recorded as the participant’s contrast sensitivity in decibel units, where 1 dB = 10 log10 contrast. A higher score indicated better contrast sensitivity; (2) proprioception was measured during sitting by matching the position of the legs on either side of a clear plastic sheet with the eyes closed. Any error in matching the limbs was recorded in degrees. After 2 practice trials, the average of 5 trials was recorded; (3) the strength of the knee extensor muscle group on the painful leg was measured by pushing isometrically at 90° against padded straps attached to strain gauges. Three trials were recorded and the highest score was used for the analysis. Knee strength scores were normalised to the participant’s height and weight to account for differences in body size using the formula:
(4) reaction time was assessed using a light as the stimulus. Depression of a switch by the hand as the response was measured in ms for 10 attempts and the average of the 10 trials was recorded; and (5) postural sway was measured using a swaymeter that recorded the sway of the body in the medio-lateral (M/L) and anterior posterior (A/P) directions while standing on a medium density foam rubber mat (70 × 60 × 15 cm thickness) with the eyes open. The total excursion of the sway in each direction was measured in millimetres.
Statistical analysis
Prior to data analysis, all variables were assessed for normality using the skewness statistic. Data transformation was performed for parameters which were found not to normally distribute. Paired t tests were used to assess the differences between pre- and 12 months post-surgery for the following variables: the overall PPA score and the PPA component tests (proprioception, strength, reaction time and balance), quality of life, physical activity and fear of falls, WOMAC scores for pain, function and stiffness. The non-parametric Wilcoxon test was used to compare differences between pre- and 12 months post-surgery for the proprioception test, and fear of falls as the values were ordinal. χ2 test was used to compare the differences in the number of falls between pre- and post-surgery. All statistical analyses were performed using SPSS Version 18.0 (SPSS Inc, Chicago, IL, USA) and a P value <0.05 was considered statistically significant.
Results
No significant differences were found between the number of falls between pre- and post-surgery (n.s.) with 48.5% reporting at least one fall in the 12 months prior to the surgery and 40% reporting at least one fall in the 12 months following the surgery (Table 1). A total of 16 falls (2 participants experienced 2 falls) were reported during the 12 months following the surgery, with 7 due to trips, 6 due to loss of balance, 2 due to a missed step and 1 due to dizziness. Nine patients had unilateral symptoms, 9 had previous total knee replacement in their contralateral knee and 17 patients had bilateral symptoms. All 35 patients attended the 12-month post-surgery assessment.
Health-related quality of life and physical activity
Health-related quality of life following the surgery was significantly reduced (P = 0.002) compared to pre-surgery status. The participants’ level of physical activity reduced slightly, both in relation to total physical activity (P = 0.02) and planned activity (P = 0.03). Self-reported pain, stiffness and function were significantly improved following the surgery with an overall improvement of the WOMAC total score (P < 0.001) as indicated in Table 1. Reduction in fear of falling was also evident at 12 months post-surgery compared to pre-surgery (P < 0.001).
Falls risk measures
The overall PPA score was not significantly different between pre- and post-surgery (n.s.), nor were lower limb proprioception (n.s.) or postural sway in the A/P or M/L direction (Table 1). However, a significant improvement was observed in knee extension strength and reaction time (P < 0.001) following surgery.
Discussion
The most important finding of the present study was that the incidence of falls following knee replacement was not significantly different compared to the number of falls in the preceding year, and remained relatively high compared to the 30–33% reported number of falls in the general community [5, 9, 30, 32]. This study was the first to investigate the risk of falls in people with knee OA before and 12 months following knee replacement surgery using a validated battery of physiological tests. The overall PPA score did not differ significantly between pre- and post-surgery; however, significant improvements were found for the knee extension strength and reaction time while balance and lower limb proprioception remained similar to the pre-surgery values.
A recent observational study reported a reduction in the number of falls following knee replacement surgery by comparing the number of falls between the pre-operative quarter (24.2% fallers) and each quarters of the first year following the surgery (11.7–11.8% fallers) [35]. The overall falls rate for the total 12 months following the surgery was 24.2%; however, the number of falls for the whole year prior to the surgery was not reported. The difference between falls rate for the 12 months following surgery between the present study (40%) and the 24.2% reported by Swinkels et al. is unclear; however, it may be related to the different definition of falls used in each study. Swinkels et al. [35] excluded falls that were a result of a major intrinsic event while the present study used the recommendation of the Prevention of Falls Network Europe group [17] where a fall is defined as “an unexpected event in which participants come to rest on the ground, floor, or lower level” [17]. This may also explain the relatively low rate of falls reported by Swinkels et al. compared to the falls rate reported for community-dwelling older people [5, 9, 30, 32]. The majority of the falls reported in the present study were due to trips and loss of balance; however, it is unclear if these falls were directly related to the operated limb. Falls in older people usually result from an interaction of multiple factors with both extrinsic (environmental) and intrinsic (individual-related) factors contributing. However, due to the presence of pain and neuromuscular deficits associated with knee replacement, it is possible that these factors may play a greater role in increasing the risk of falls post-surgery.
The overall PPA score did not differ significantly between pre- and post-surgery but several individual tests demonstrated significant improvements, including knee extension strength and reaction time. Balance and lower limb proprioception, however, remained similar to the pre-surgery values. In our previous work, we found reduced proprioception and knee extension strength for the same surgical group prior to and 4 months following the surgery compared to an age-matched control group [21]. The current results, therefore, indicate no improvement in proprioception at 12 months following the surgery but significant improvement in knee extension strength. The activity level of the participants at 12 months following the surgery was significantly lower than the level of activity reported prior to the surgery, but still indicated a relatively high level of physical activity engagement compared to early after the surgery [21] and to other older people when using the same scale [8, 21]. The improvement in knee extension strength may therefore be partly explained by the increase in the level of physical activity following the surgery. Given that muscle weakness has been shown to be a risk factor for falls [22, 23, 29, 39], the improvement in strength may possibly contribute to the slight reduction in the number of falls experienced following the surgery. Moreover, strengthening the knee extensor muscles is also important for improvement in functional performance and daily functioning for people following knee replacement surgery [27, 28].
Adequate sensorimotor function, such as proprioceptive acuity, is important to ensure accurate limb placement during functional tasks as well as controlling the degree of knee movement. Although the literature is inconsistent in relation to changes in proprioception following knee replacement surgery [11, 12, 15, 21], we have previously reported impaired proprioception for the current participants at their pre-surgery assessment as well as early after the surgery compared to an age-matched control group [21]. The current results indicate that proprioception did not improve 12 months following the surgery. Impaired lower limb proprioception is a well-recognised independent risk factor for falls [22, 25, 33]. Although it is unclear if the poor proprioception observed following the surgery was related to the occurrence of falls, it is possible that inadequate sensorimotor function at the knee affected movement control, which contributed to loss of balance. It is therefore recommended that rehabilitation following knee replacement surgery should include exercises to improve knee neuromuscular control as well as knee extension strength.
Musculoskeletal pain has been shown to be associated with an increased risk of falls [10, 19, 20]. Persistent pain and disability are often reported following knee replacement surgery [2, 4]. In the present study, a significant reduction in pain and stiffness and an improvement in function were observed at 12 months post-surgery. The level of pain, however, varied considerably following the surgery as indicated by the large standard deviation. This potentially could have affected health-related quality of life scores, which significantly deteriorated post-surgery. Fear of falling was significantly improved following the surgery which may be related to the general improvement in function and pain reduction, as patients may feel more confident to use and trust the operated leg.
It is important to acknowledge the limitations of the study. People who undergo knee replacement surgery may have a range of other health problems which may not be related to their operated knee. The occurrence of falls following knee replacement surgery therefore may have been related to other factors which were not assessed in the current study. Further study is needed to investigate the occurrence of falls in people following knee replacement and possible interventions to alleviate the risk of falls. The clinical implication of the study is that patients who undergo knee replacement surgery should maintain active involvement in physical activity not just for their general well-being and better daily functioning but also to reduce the risk of falls.
Conclusion
People with knee OA demonstrate improvements in pain, function, fear of falling and knee extension strength at 12 months following knee replacement surgery. Despite this, the number of falls experienced 12 months following the surgery remains relatively high, which may be partly attributed to the persistence of impaired lower limb proprioception. Although knee replacement surgery generally improves function and alleviates pain, people who undergo knee replacement surgery should maintain adequate strength and neuromuscular control through active engagement in physical activity or exercise rehabilitation to reduce their risk of falling.
References
Australian Orthopaedic Association National Joint Replacement Registry (2010) Annual report. Adelaide. http://www.dmac.adelaide.edu.au/aoanjrr/documents/aoanjrrreport_2010.pdf
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ (2007) The role of pain and function in determining patient satisfaction after total knee replacement. Data from the national joint registry for England and Wales. J Bone Jt Surg Br 89:893–900
Bellamy N (1989) Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum 18:14–17
Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, Houle T (2003) Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res 416:27–36
Campbell AJ, Borrie MJ, Spears GF (1989) Risk factors for falls in a community based prospective study of people 70 years and older. J Gerontol 44:M112–M117
Chiba H, Ebihara S, Tomita N, Sasaki H, Butler JP (2005) Differential gait kinematics between fallers and non-fallers in community dwelling elderly people. Geriatr Gerontol Int 5:127–134
Cushnaghan J, Bennett J, Reading I, Croft P, Byng P, Cox K, Dieppe P, Coggon D, Cooper C (2009) Long-term outcome following total knee arthroplasty: a controlled longitudinal study. Ann Rheum Dis 68:642–647
Delbaere K, Hauer K, Lord SR (2009) Evaluation of the incidental and planned activity questionnaire (IPAQ) for older people. Br J Sports Med 44:1029–1034
Dolinis J, Harrison JE, Andrews GR (1997) Factors associated with falling in older Adelaide residents. Aust N Z J Public Health 21:462–468
Foley SJ, Lord SR, Srikanth V, Cooley H, Jones G (2006) Falls risk is associated with pain and dysfunction but not radiographic osteoarthritis in older adults: Tasmanian older adult cohort study. Osteoarthr Cartil 14:533–539
Frost H, Lamb SE, Robertson S (2002) A randomized controlled trial of exercise to improve mobility and function after elective knee arthroplasty. Feasibility, results and methodological difficulties. Clin Rehabil 16:200–209
Fuchs S, Thorwesten L, Niewerth S (1999) Proprioceptive function in knees with and without total knee arthroplasty. Am J Phys Med Rehabil 78:39–45
Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D (1998) Health-related quality of life after knee replacement. J Bone Jt Surg Am 80:163–173
Hawthorne G, Richardson J, Osborne R (1999) The assessment of quality of life (AQoL) instrument: a psychometric measure of health-related quality of life. Qual Life Res 8:209–224
Isaac SM, Barker KL, Danial IN, Beard DJ, Dodd CA, Murray DW (2007) Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee 14:212–217
Kempen GI, Yardley L, van Haastregt JC, Zijlstra GA, Beyer N, Hauer K, Todd C (2008) The short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 37:45–50
Lamb SE, Jorstad-Stein EC, Hauer K, Becker C (2005) Development of a common outcome data set for fall injury prevention trials: the prevention of falls network Europe consensus. J Am Geriatr Soc 53:1618–1622
Lawlor DA, Patel R, Ebrahim S (2003) Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ 327:712–717
Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik JM (2002) Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc 50:671–678
Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, Kiel DP, Lipsitz LA, Bean JF (2009) Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA 302:2214–2221
Levinger P, Menz HB, Wee E, Feller JA, Bartlett JR, Bergman NR (2011) Physiological risk factors for falls in people with knee osteoarthritis before and early after knee replacement surgery. Knee Surg Sports Traumatol Arthrosc 19:1082–1089
Lord SR, Clark RD, Webster IW (1991) Physiological factors associated with falls in an elderly population. J Am Geriatr Soc 39:1194–1200
Lord SR, McLean D, Stathers G (1992) Physiological factors associated with injurious falls in older people living in the community. Gerontology 38:338–346
Lord SR, Menz HB, Tiedemann A (2003) A physiological profile approach to falls risk assessment and prevention. Phys Ther 83:237–252
Lord SR, Ward JA, Williams P, Anstey KJ (1994) Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc 42:1110–1117
March LM, Bagga H (2004) Epidemiology of osteoarthritis in Australia. Med J Aust 180:S6–S10
Meier W, Mizner RL, Marcus RL, Dibble LE, Peters C, Lastayo PC (2008) Total knee arthroplasty: muscle impairments, functional limitations, and recommended rehabilitation approaches. J Orthop Sports Phys Ther 38:246–256
Mizner RL, Petterson SC, Snyder-Mackler L (2005) Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther 35:424–436
Moreland JD, Richardson JA, Goldsmith CH, Clase CM (2004) Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 52:1121–1129
Morris M, Osborne D, Hill K, Kendig H, Lundgren-Lindquist B, Browning C, Reid J (2004) Predisposing factors for occasional and multiple falls in older Australians who live at home. Aust J Physiother 50:153–159
Nahit ES, Silman AJ, Macfarlane GJ (1998) The occurrence of falls among patients with a new episode of hip pain. Ann Rheum Dis 57:166–168
O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137:342–354
Rossat A, Fantino B, Nitenberg C, Annweiler C, Poujol L, Herrmann FR, Beauchet O (2010) Risk factors for falling in community-dwelling older adults: which of them are associated with the recurrence of falls? J Nutr Health Aging 14:787–791
Sturnieks DL, Tiedemann A, Chapman K, Munro B, Murray SM, Lord SR (2004) Physiological risk factors for falls in older people with lower limb arthritis. J Rheumatol 31:2272–2279
Swinkels A, Newman JH, Allain TJ (2009) A prospective observational study of falling before and after knee replacement surgery. Age Ageing 38:175–181
Valtonen A, Poyhonen T, Heinonen A, Sipila S (2009) Muscle deficits persist after unilateral knee replacement and have implications for rehabilitation. Phys Ther 89:1072–1079
Walsh M, Woodhouse LJ, Thomas SG, Finch E (1998) Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther 78:248–258
Williams SB, Brand CA, Hill KD, Hunt SB, Moran H (2010) Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study. Arch Phys Med Rehabil 91:106–114
Wolfson L, Judge J, Whipple R, King M (1995) Strength is a major factor in balance, gait, and the occurrence of falls. J Gerontol A Biol Sci Med Sci 50. Spec no: 64-67
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81:646–656
Acknowledgments
This study was funded by the Clive and Vera Ramaciotti Foundation and the Arthritis Australia. HBM is currently a National Health and Medical Research Council fellow (Clinical Career Development Award, ID: 433049). The authors would like to thank Margaret Perrott for her assistance in the data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levinger, P., Menz, H.B., Morrow, A.D. et al. Lower limb proprioception deficits persist following knee replacement surgery despite improvements in knee extension strength. Knee Surg Sports Traumatol Arthrosc 20, 1097–1103 (2012). https://doi.org/10.1007/s00167-011-1710-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1710-y