Abstract
Purpose
The purpose of this study was to evaluate the functional and radiographic outcomes of a novel surgical technique devised to treat chronic lateral ankle instability. The technique involves direct repair of the anterior talofibular ligament and anatomic reconstructions of the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL) using a free semitendinosus tendon allograft and interference screws.
Methods
This retrospective study involved a review of the records of 27 patients (28 ankles) with chronic lateral ankle instability treated from 2007 to 2009. VAS pain scores, AOFAS scores, Karlsson–Peterson ankle scores (24 ankles), and patient satisfaction were evaluated at median of 19 (12–26) months postoperatively. Radiographically, talar tilt angles and anterior talar translation were assessed in pre- and postoperative ankle stress views.
Results
Median patient age at surgery was 36.5 (16–57) years. Median VAS pain score decreased from 6 (3–9) to 2 (0–4) (P < 0.05), and median AOFAS score improved from 63 (41–84) to 91 (81–100) preoperatively to final follow-up (P < 0.05). Median Karlsson–Peterson score also significantly improved from 55 (32–77) to 80 (59–100) (P < 0.05), whereas talar tilt decreased from 17.8° (10.0°–25.5°) to 6.7° (0.3°–13.0°) and the mean anterior drawer test decreased from 10.0 mm (0.6–19.4) to 4.5 mm (0.2–8.7) (P < 0.05). Eighty-eight percent (21/24) were satisfied with surgery. No complication, such as subtalar stiffness or recurrent instability, was encountered.
Conclusions
The described technique, which involves anatomic reconstruction of the ATFL and CFL using the semitendinosus tendon and interference screws with direct repair of the capsule, is a viable option for treating lateral ankle instability with stable tendon fixation and provides satisfactory clinical outcomes.
Level of evidence
Case-series, Level IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ankle sprain is one of the most common musculoskeletal injuries, and the majority of ankle sprain cases involve the lateral ankle ligaments [8]. Although most ankle sprains respond well to conservative measures, chronic instability following an acute lateral ankle sprain has been reported to occur in 20–40% of patients [28]. Furthermore, although rehabilitation often improves ankle instabilities, some individuals are eventually indicated for lateral ankle ligament reconstruction due to persistent ankle instability.
More than 50 surgical procedures have been described to address lateral ankle stability [21]. These vary from direct repair of the anterior talofibular ligament (ATFL) [4, 19] and of the calcaneofibular ligament (CFL) [14–16] to reconstructions based on the usages of autograft or allograft tissues [11, 12, 17, 29, 31]. However, the best surgical option remains debatable [6]. The modified Broström procedure has been most widely used for direct ligament repair [1, 4, 15, 20], but this procedure [4] is not always possible because of poor ATFL or CFL quality or a deficiency of these ligaments, which prevents effective shortening imbrication. Furthermore, the importance of CFL reconstruction has been emphasized recently [26]. However, it is difficult to achieve CFL reconstruction efficiently during the Broström procedure, and problems, such as hindfoot motion restriction, associated with nonanatomic tenodesis [7, 9, 12, 31], when a peroneus brevis is utilized, have also been reported [22, 23]. On the other hand, others have reported that anatomic reconstruction of injured ligaments restores normal resistance to anterior translation and inversion without restricting subtalar or ankle motion [5, 9, 21], and as a result, anatomic reconstructions for lateral ankle instability utilizing an autograft or allograft tendon [6, 10, 26, 30] have gained in popularity. However, most techniques in the literature fall short of satisfying the requirements for the anatomic repositioning of ligaments, and stable ligament fixation.
Here, we describe a novel surgical technique for chronic lateral ankle instability that involves anatomic reconstruction of the anterior talofibular and CFLs using a semitendinosus tendon allograft and interference screws with shortening repair of the ATFL and capsule. The hypothesis of the paper is that the described technique satisfies requirements, such as anatomic ligament repositioning and stable ligament fixation during lateral ankle ligament reconstruction.
Materials and methods
This study was performed on 27 patients (28 ankles) with chronic lateral ankle instability that were treated using our surgical technique from 2007 to 2009 by one senior author (HGJ). Preoperative and postoperative records, radiographs, and operative notes were reviewed, and functional statuses and radiographic parameters were prospectively assessed. Institutional Review Board approval was obtained for this study, and informed consent was obtained from all 27 patients involved.
The inclusion criteria for the surgical procedure were chronic lateral ankle instability of at least 3-month duration with repeated episodes of recurrent inversion sprain and evidence of lateral ankle instability by clinical and radiographic examinations (talar tilt >10°) that failed to respond to peroneal muscle-strengthening exercise. Varus stress view and the anterior drawer test were performed utilizing the Telos SE 2000 stress device (ARD Medizin Produkte GmbH, Germany). Radiographs were taken in neutral position at 150 N of stress force. Cases with intra-operative findings of a much attenuated or deficient ATFL, which therefore, were expected to achieve a poor outcome by direct ligament repair only and were selected for ligament reconstruction using an allograft tendon. Preoperative ankle MR (magnetic resonance) images that visualized the thicknesses and contours of the ATFL and CFL (indicators of ligament condition) were found to be helpful for planning surgical options preoperatively. Young and physically demanding patients were favored for surgery.
Surgical technique and postoperative management
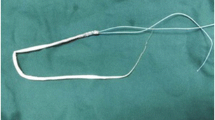
Under general or spinal anesthesia, a patient was laid in a semilateral position and a thigh tourniquet was applied. A 12-cm-long “U”-shaped incision was centered over the tip of the fibula and extended anteriorly over the lateral talus and posteriorly over the lateral calcaneus and posterior border of the fibula (Fig. 1). The ATFL and capsule at the fibular attachment site were then dissected and identified. After evaluating and confirming attenuation, deficiency, and scarring of ATFL and CFL tissue, and in the expectation of a poor outcome for Broström repair, lateral ligament reconstruction using a free allograft tendon was decided upon intraoperatively. The ATFL was then longitudinally incised along its fibular insertion leaving about a 5-mm ligament stump at the fibula side. A second incision at right angles to the initial incision was added from the center of the initial incision to form a “T” shape ending at the ATFL attachment at the base of talar neck adjacent to the talar body. A semitendinosus allograft (Community Tissue Services, Dayton, USA) of thickness 3.5–4.5 mm was used (tendons had been previously sterilized by irradiation and preserved at −40°C). Both ends of the semitendinosus allograft were sutured over a length of 1.5 cm by a whip stitch using #2 Ti-cron (Tyco Healthcare-Syneture, Connecticut, USA).
A tunnel of diameter 5.0–7.0 mm and depth 18 mm was prepared at the upper margin of the footprint of the ATFL attachment at the anterior border of the talar body in a posterosuperior direction under C-arm fluoroscopic guidance. One end of the semitendinosus tendon was inserted in the hole and firmly fixed with a 4.75-mm-sized interference screw (Arthrex Inc., Naples, FL, USA).
At the footprints of the ATFL and CFL attachment sites on the distal fibula, two almost parallel bone tunnels of diameters equal to the allograft tendon thickness, with a 2–4 mm space between tunnel rims, were made for tendon passage. The ATFL was newly reconstructed by passing the semitendinosus tendon through the proximal bone tunnel of distal fibula made at the ATFL insertion point in an anterior to posterior direction using a Nitinol suture passing wire (Arthrex Inc., Naples, FL, USA) and by stabilizing the tendon with either a suture anchor, simple suture, or interference screw at 0° of ankle extension and 10° eversion under maximum tension. The tendon was then passed through the distal fibular tunnel in posterior to anterior direction to form the fibular insertion of the CFL. Subcutaneous tissue was dissected at the inferior pole of the “U”-shaped skin incision, while taking care to identify and protect the sural nerve. The peroneal tubercle area of the calcaneus, used for CFL insertion, was dissected, and a bone tunnel was prepared at the CFL footprint site in lateral to medial direction. The free end of the tendon graft was then passed from the distal fibula tip underneath the peroneal tendons to be positioned at the CFL insertion area at the peroneal tubercle. The distal tendon end was shortened with the intention of inserting about 3 cm of the tendon end, and a 2-cm whip stitch was applied at the newly formed tendon end. The tendon graft was then passed through the calcaneus hole, and the tendon was firmly fixed with an interference screw in 0° of ankle extension and 10° of eversion while maintaining strong tension on the tendon medially. It was then confirmed that the reconstructed ATFL and CFL were strongly tensioned and that screws were firmly fixed (Fig. 2). Imbrication of the previously incised ATFL remnant and capsule was then performed using the “pants-over-vest” technique to augment the free tendon reconstruction. The absence of the lateral ankle laxity and the maintenance of a normal range of ankle motion were confirmed by manual examination. The position of the tunnels and interference screws was then confirmed using an image intensifier.
Evaluation methods
Twenty-three patients (24 ankles) were successfully contacted and returned for a final follow-up examination at a median 19 months (12–26 months) postoperatively. At final clinic visits, patients were assessed using a standardized questionnaire and by physical examination. Patients were also asked to rate their pain levels on a 10-point VAS scale. In addition, American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot functional scores and Karlsson–Peterson ankle instability scores were evaluated pre- and postoperatively. Ranges of motion of ankles (dorsiflexion and plantar flexion) and of subtalar joints (inversion and eversion) were physically examined before surgery and at latest follow-up. Subtalar range of motion was measured in the prone position with knee flexed at 90° using a standard goniometer. In addition, patients were also asked to rate their overall satisfaction with their surgical results as very satisfied, satisfied, fair, or dissatisfied.
For radiographic analysis at final follow-up, talar tilt angles on varus stress views and anterior talar displacement (defined as the distance between antero-inferior margin of distal tibia and the anterosuperior tip of the talar head as determined by the anterior drawer test) were measured and compared with preoperative data. Each radiographic value was measured twice by two observers (both orthopedic surgeons) individually, and average values were then calculated. Measurement accuracies for talar tilt and anterior talar translation were 0.1° and 0.1 mm as determined using a picture archiving and communication system (PACS; GE Healthcare, Mt. Prospect, IL, USA) workstation.
Statistical analysis
SPSS software (version 12.0, SPSS Inc., Chicago) was utilized throughout. The paired t test was used to compare and analyze preoperative and postoperative VAS pain scores, AOFAS ankle-hindfoot function scores, Karlsson–Peterson ankle scores, and radiographic measurements (talar tilt angle and anterior talar translation). Statistical significance was accepted for P values of <0.05.
Results
The median age of the 27 patients (28 ankles) was 36.5 years (16–57 years). All 28 ankles had a previous ankle sprain history and had a preoperative symptomatic recurrent ankle sprain period of 61.5 months (3–120 months). The semitendinous allograft tendons used for reconstruction of the ATFL and CFL had a median thickness of 4.0 mm (3.5–4.5 mm). For talar attachment sites of ATFLs, holes of average width 6.0 mm (5.0–7.0 mm) and of median length 18 mm were produced. Allograft tendons were fixed using interference screws of median length 5.5 mm (4.75–6.25 mm). Two fibular tunnels were prepared of average diameter 4.5 mm (4.0–5.0 mm). In calcanei, holes were of median diameter 5.3 mm (4.5–6.0 mm), and interference screws of median diameter 5.5 mm (4.75–6.25 mm) were used for fixation.
Twenty-four (23 patients; 20 men; both ankles in one female patient) of the 28 ankles were followed for more than 1 year after surgery with a median follow-up of 19 months (12–26 months). Median preoperative VAS pain score was 6 points (3–9 points), and this reduced significantly to 2 points (0–4 points) at final follow-up (P < 0.05). Median preoperative AOFAS ankle-hindfoot function score was 63 points (41–84 points), and this increased to 91 points (81–100 points) at final follow-up (P < 0.05). Similarly, median preoperative Karlsson–Peterson ankle instability score was 55 points (32–77 points), and this increased significantly to 80 points (59–100 points) at final follow-up. Regarding the Karlsson–Peterson instability scale, median instability increased significantly from 13 points (5–20 points) to 20 points (15–25 points), which is close to the maximum total score of 25. It took a median 4.0 months (1–7 months) for the 23 patients to return to work.
Median preoperative and postoperative tibio-talar and subtalar ranges of motion were not significantly different (NS), but no ankle demonstrated a significant limitation of tibio-talar or subtalar range of motion postoperatively.
Of the 20 ankles that underwent concomitant arthroscopic examinations, four ankles had an osteochondral lesion of the talus (OLT) and four had a degenerative chondral defect (DCD). Debridement and microfracture were performed on four OLT cases, whereas debridement and multiple drilling were performed on the four DCD cases. Marked synovitis was found in 12 ankles and was treated by arthroscopic synovectomy.
In terms of patient satisfaction, results for 21 of the 24 ankles (88%) were satisfactory or better (very satisfied 50% and satisfied 38%). In two of the three ankles rated as “fair,” patients complained of residual ankle pain related to a combined DCD lesion, but nevertheless, ankles became stable postoperatively.
In terms of postoperative complications, one patient complained of postoperative sural nerve neuralgia at the posterolateral ankle, which resolved after conservative treatment. No other complication, such as a wound problem, recurrent ankle instability, subtalar joint stiffness, a peroneal tendon problem, or distal fibula fracture through bone tunnels, was encountered.
Radiographic evaluations
According to radiological results, median preoperative talar tilt angle under varus stress decreased significantly from 17.8° (10.0°–25.5°) to 6.7° (0.3°–13.0°) at final follow-up (P < 0.05). Anterior talar translations measured using the anterior drawer test also decreased from a median of 10.0 mm (0.6–19.4) to a median of 4.5 mm (0.2–8.7 mm), which represented a significance improvement (P < 0.05).
Discussion
This study shows that the described technique, which involves anatomic reconstruction of the ATFL and CFL using the semitendinosus tendon and interference screws with direct repair of the capsule, is a viable option for treating lateral ankle instability with stable tendon fixation and provides satisfactory clinical outcomes. The most important findings of the present study are that the described technique achieves anatomic repositioning and stable fixation. Twenty to forty percent of severe ankle sprains cause ankle instability [28], and lateral ligament reconstructive surgery is indicated when rehabilitation therapy or a brace fails to elicit an improvement. Many reports have presented surgical techniques for treating lateral ankle instabilities [1, 4, 11–13, 15, 20, 31], but the majority concern is the reconstruction of structures responsible for talar instabilities [28].
Reconstructive surgeries for lateral ankle instabilities may be classified as anatomic or nonanatomic. Anatomic surgeries can be further subdivided into lateral ligament shortening procedures and anatomic reconstruction using a free tendon. Nonanatomic reconstruction techniques are usually tenodesis procedures that utilize a half or all of the peroneus brevis tendon [7, 12, 31], which is actually the main dynamic stabilizer of the lateral side of the ankle. Tenodesis procedures are also rather invasive in terms of approach and have been reported to tend to restrict ankle and subtalar motions excessively [22, 23, 27] as compared with anatomic reconstruction procedures. Furthermore, in one study, more degenerative changes in ankles were reported in a tenodesis group during long-term follow-up [24].
The Broström procedure and its modifications [1, 4, 15, 20], which involve augmentation with inferior extensor retinaculum (IER), have been most commonly performed and have been reported to have a favorable outcome [3, 21, 24]. Modified Broström procedures are known to be technically less demanding than free tendon reconstruction or tenodesis procedures, but good outcomes cannot be expected of a modified Broström procedure when the ATFL or IER is severely attenuated or defective, or when a Broström procedure has already failed [10, 13]. Moreover, although reconstructions of the CFL and ATFL have been recently emphasized in the context of ideal lateral ligament reconstruction [26], often during the Broström procedure or its modifications, reconstruction of the CFL is omitted or replaced with IER augmentation. Therefore, in order to achieve anatomic, stable, and concomitant reconstructions of the ATFL and CFL, reconstruction of the lateral ligaments utilizing a free tendon graft has become popular. Although many reconstruction techniques have been introduced that utilize an autograft tendon [10, 26, 30], synthetic carbon fiber [2], or an allograft tendon [6], the majority have been reported to be incapable of reviving the ATFL and CFL anatomically, of being technically difficult to reproduce, or to result in questionable stability of ATFL or CFL tendon to bone fixation. In a previous study, during lateral ligament reconstruction utilizing a bone-patella tendon graft [30], suture anchors were used for tendon-bone fixation, though they have been proven to be biomechanically weaker than interference screw fixation [18]. Furthermore, other previous reports of lateral ligament reconstruction utilizing semitendinosus tendon [6, 26] failed to reproduce the anatomic orientations of ATFL and CFL reported in a cadaveric study by Burks and Morgan [5]. In this previous cadaveric study, it was reported that the average width and length of the ATFL were 7.2 and 24.8 mm, respectively, whereas the corresponding CFL values were 5.3 and 35.8 mm, respectively [5]. Furthermore, with the foot in a plantigrade position, the CFL was found to form an angle of 133° with the fibula, and the ATFL and CFL were found to originate on average at 10 and 8.5 mm from the fibula tip, respectively. During our surgical procedures, we aim to reconstruct the ATFL and CFL anatomically according to the individual’s specific anatomy by meticulous dissection and to localize the footprints of the ATFL and CFL attachments at the fibula, talar neck, and calcaneus with screw holes and tunnels prepared for reconstruction. Although ATFL and CFL reconstructions with gracilis tendon by Coughlin [10] appeared close to anatomic in terms of orientation, making loop tunnels in the talus, fibula, and calcaneus appeared technically demanding for a routine procedure. On the other hand, our technique requires 1-hole tunnels for tendon fixation with interference screws, and we found this to be more stable and technically less demanding than “loop type” tendon fixation.
During the early study period, titanium screws were used, but these were later changed to bioabsorbable screws due to importation concerns. However, no loosening of either screw type was observed after stable fixation. The only screw-related problems encountered were two cases of intra-operative bioabsorbable screw breakage during fixation in relatively small holes, and these were replaced with smaller screws.
The described technique utilizes an allograft tendon in order to avoid donor site morbidity and shorten operation time. However, the use of an allograft does raise issues of possible disease transmission and cost [6, 25]. We found that a semitendinous tendon of thickness 3.5–4.5 mm most appropriates as a tendon graft. The limitation of this study is that results were based on a relatively small number of cases and that the follow-up period was relatively short, and thus, additional large-scale study is required with a long-term follow-up. The significance of this study is that the described technique provides anatomical reconstruction of the lateral ankle ligaments (ATFL and CFL) using free tendon and interference screws with firm tendon fixation. Furthermore, we believe that the described technique can be recommended as a viable alternative for the treatment of chronic lateral ankle instability, especially for ankles with poor lateral ligament tissues.
Conclusions
The described technique, which involves anatomic reconstruction of the ATFL and CFL using a semitendinosus allograft tendon and interference screws with adjunctive shortening repair of the original ATFL and capsule, was found to be highly effective and to provide stable fixation for addressing lateral ankle instabilities, especially in ankles with poor lateral ligament tissues.
References
Ahlgren O, Larsson S (1989) Reconstruction for lateral ligament injuries of the ankle. J Bone Joint Surg Br 71(2):300–303
Becker HP, Rosenbaum D, Zeithammel G, Gnann R, Bauer G, Gerngross H, Claes L (1996) Tenodesis versus carbon fiber repair of ankle ligaments: a clinical comparison. Clin Orthop Relat Res 325:194–202
Bell SJ, Mologne TS, Sitler DF, Cox JS (2006) Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med 34(6):975–978
Broström L (1966) Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand 132(5):551–565
Burks RT, Morgan J (1994) Anatomy of the lateral ankle ligaments. Am J Sports Med 22(1):72–77
Caprio A, Oliva F, Treia F, Maffulli N (2006) Reconstruction of the lateral ankle ligaments with allograft in patients with chronic ankle instability. Foot Ankle Clin 11(3):597–605
Chrisman OD, Snook GA (1969) Reconstruction of lateral ligament tears of the ankle. An experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am 51(5):904–912
Colville MR (1998) Surgical treatment of the unstable ankle. J Am Acad Orthop Surg 6(6):368–377
Colville MR, Marder RA, Zarins B (1992) Reconstruction of the lateral ankle ligaments. A biomechanical analysis. Am J Sports Med 20(5):594–600
Coughlin MJ, Schenck RC Jr, Grebing BR, Treme G (2004) Comprehensive reconstruction of the lateral ankle for chronic instability using a free gracilis graft. Foot Ankle Int 25(4):231–241
Elmslie RC (1934) Recurrent subluxation of the ankle-joint. Ann Surg 100(2):364–367
Evans DL (1953) Recurrent instability of the ankle; a method of surgical treatment. Proc R Soc Med 46(5):343–344
Girard P, Anderson RB, Davis WH, Isear JA, Kiebzak GM (1999) Clinical evaluation of the modified Broström-Evans procedure to restore ankle stability. Foot Ankle Int 20(4):246–252
Gould N (1987) Repair of lateral ligament of ankle. Foot Ankle 8(1):55–58
Gould N, Seligson D, Gassman J (1980) Early and late repair of lateral ligament of the ankle. Foot Ankle 1(2):84–89
Hamilton WG, Thompson FM, Snow SW (1993) The modified Broström procedure for lateral ankle instability. Foot Ankle 14(1):1–7
Horibe S, Shino K, Taga I, Inoue M, Ono K (1991) Reconstruction of lateral ligaments of the ankle with allogeneic tendon grafts. J Bone Joint Surg Br 73(5):802–805
Jeys L, Korrosis S, Stewart T, Harris NJ (2004) Bone anchors or interference screws? A biomechanical evaluation for autograft ankle stabilization. Am J Sports Med 32(7):1651–1659
Karlsson J, Bergsten T, Lansinger O, Peterson L (1988) Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am 70(4):581–588
Karlsson J, Bergsten T, Lansinger O, Peterson L (1989) Surgical treatment of chronic lateral instability of the ankle joint. A new procedure. Am J Sports Med 17(2):268–273 (discussion 273–274)
Karlsson J, Eriksson BI, Bergsten T, Rudholm O, Sward L (1997) Comparison of two anatomic reconstructions for chronic lateral instability of the ankle joint. Am J Sports Med 25(1):48–53
Kjaersgaard-Andersen P, Madsen F, Frich LH, Wethelund JO, Sojbjerg JO (1990) Lateral hindfoot instability treated with the Evans tenodesis: a biomechanical analysis. J Foot Surg 29(1):25–32
Kjaersgaard-Andersen P, Sojbjerg JO, Wethelund JO, Helmig P, Madsen F (1989) Watson-Jones tenodesis for ankle instability. A mechanical analysis in amputation specimens. Acta Orthop Scand 60(4):477–480
Krips R, van Dijk CN, Halasi PT, Lehtonen H, Corradini C, Moyen B, Karlsson J (2001) Long-term outcome of anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: a multicenter study. Foot Ankle Int 22(5):415–421
Marrale J, Morrissey MC, Haddad FS (2007) A literature review of autograft and allograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 15(6):690–704
Paterson R, Cohen B, Taylor D, Bourne A, Black J (2000) Reconstruction of the lateral ligaments of the ankle using semi-tendinosis graft. Foot Ankle Int 21(5):413–419
Rosenbaum D, Bertsch C, Claes LE (1997) NOVEL Award 1996: 2nd prize tenodeses do not fully restore ankle joint loading characteristics: a biomechanical in vitro investigation in the hind foot. Clin Biomech (Bristol, Avon) 12(3):202–209
Sammarco VJ (2001) Complications of lateral ankle ligament reconstruction. Clin Orthop Relat Res 391:123–132
Snook GA, Chrisman OD, Wilson TC (1985) Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am 67(1):1–7
Sugimoto K, Takakura Y, Kumai T, Iwai M, Tanaka Y (2002) Reconstruction of the lateral ankle ligaments with bone-patellar tendon graft in patients with chronic ankle instability: a preliminary report. Am J Sports Med 30(3):340–346
Watson-Jones R (1955) Fractures and joint injuries, vol II, 4th edn. E & S Livingstone Ltd, Edinburgh
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jung, HG., Kim, TH., Park, JY. et al. Anatomic reconstruction of the anterior talofibular and calcaneofibular ligaments using a semitendinosus tendon allograft and interference screws. Knee Surg Sports Traumatol Arthrosc 20, 1432–1437 (2012). https://doi.org/10.1007/s00167-011-1666-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1666-y