Abstract
Purpose
This study aims to clarify the influence of surgical exposure on intra-operative soft tissue balance measurements using a new tensor in minimal incision total knee arthroplasty (TKA).
Methods
Sixty patients with osteoarthritis of the knee received minimal incision TKAs. Twenty patients received a posterior-stabilized TKA using a quadriceps sparing approach, and the other forty patients, using a limited medial parapatellar (mini) approach. After femoral trial placement, soft tissue balance was measured using an offset type tensor at full extension and 90° of knee flexion, with the patella both laterally retracted and reduced. The joint component gap and varus imbalance were used to assess the difference in patellar position and surgical exposure.
Results
At extension, the joint component gap and varus imbalance showed no statistical difference regardless of patellar position in either TKA. However, the joint component gaps decreased at 90° of flexion when the patella was laterally retracted in both TKAs. Additionally, a significantly smaller joint gap was observed in the quadriceps sparing TKA than the mini-TKA with a retracted patella at 90° of flexion. Varus ligament imbalances decreased with the patella laterally retracted at 90° of flexion in the quadriceps sparing TKA, not in the mini-TKA.
Conclusion
Surgeons should be aware of the influence in surgical exposure of the joint gap and ligament balance during patella shift in minimal incision TKA.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accurate osteotomies and implantations in total knee arthroplasties (TKAs) have become relatively simple procedures with the improvement of surgical instruments such as the introduction of the computer-assisted navigation system [2, 4, 7, 12, 14–18]; however, achieving adequate soft tissue balancing during the operation including adjusting joint gaps and ligament imbalances remains difficult, and much is left to the surgeon’s subjective feel and experience. In order to permit soft tissue balancing under more physiological conditions, an offset type tensor has been developed at our institution to assess soft tissue balance throughout the range of motion with reduced patellofemoral (PF) and aligned tibiofemoral joints [11, 13, 19]. Recently, surgical techniques associated with minimal incision surgery (MIS) for TKAs have been developed, and there have been several reports showing good clinical results [1, 5, 20]. However, with limited exposure and visualization, the skin, capsular tissues and bone surfaces receive higher stresses due to the retraction required. MIS TKAs that do not require patellar eversion, in broad terms, include the use of quadriceps sparing (QS), mini-midvastus, mini-subvastus and limited parapatellar approaches because of the different approaches to the vastus medialis oblique (VMO) that are employed. Thus, it is clear that the stress caused by patellar retraction during soft tissue evaluations changes depending on the approach used and possibly affects measurement. Based on these findings, we hypothesized that intra-operative soft tissue balance may be different even among different approaches in MIS TKA.
The first purpose of the present study was to compare the difference in soft tissue balance in MIS TKA between the two patellar positions: retraction and then reduction. Secondly, we investigated the influence of different approaches on intra-operative soft tissue balance in MIS TKAs with different patellar positions. The hypothesis was that soft tissue balance is more influenced by patellar positions in MIS especially at flexion.
Materials and methods
From a group of 60 consecutive osteoarthritic knees, 20 patients were intra-operatively selected to receive a posterior-stabilized (PS) TKA (NexGen PS Flex, Zimmer, Inc., Warsaw, IN) using QS approach (QS TKA) and the other 40 patients a PS TKA (NexGen LPS Flex, Zimmer, Inc., Warsaw, IN) using a limited medial parapatellar approach (mini-TKA) between February 2005 and December 2008, depending on VMO anatomical variation. The QS TKA group had a median age of 74 years (range 63–83), and 13 women and 7 men were included, while the mini-TKA group had a median age of 74 years (range 60–85) and 31 women and 9 men were included. After excluding patients with valgus deformity and severe bony defects, each remaining patient had a varus deformity, with an average pre-operative coronal plane alignment of 10.6 ± 1.0° in varus in QS TKA and 9.3 ± 1.2° in varus in mini-TKA. All surgeries were performed by the same senior author (HM).
Offset type tensor
As previously described, this device is ultimately designed to permit surgeons to measure the ligament balance (varus angle) and joint centre gap (joint/component gap), while applying a constant joint distraction force [9, 11, 19]. Joint distraction forces ranging from 30 lb (13.6 kg) to 80 lb (36.3 kg) can be exerted between the see-saw and platform plates through a specially made torque driver, which can change the applied torque value. Once appropriately distracted, attention is focused on two scales that correspond to the tensor: the angle (°, positive value in varus imbalance) between the see-saw and platform plates, and the distance (mm) between the centre mid-points of the upper surface of the see-saw plate and the proximal tibial cut. The angular divisions and distance are put on a graded scale by 1° and 1 mm and measured with 0.5 as the minimum unit. In primary in vitro experiments, the error for joint distraction was obtained within ±3%.
Intra-operative measurement
All TKAs were performed using the measured resection technique. A limited medial parapatellar arthrotomy exposed the quadriceps tendon within 2 cm in mini-TKA, and the QS arthrotomy did not damage the VMO in QS TKA, depending on the anatomical VMO variation. In all patients, the ACL and PCL were both resected. Distal femoral osteotomy was performed perpendicular to the mechanical axis of the femur using pre-operative long leg radiographs. Femoral external rotation was preset at 3° or 5° relative to the posterior condylar axis depending on pre-operative computed tomography. After this, a proximal tibial osteotomy was done, ensuring that each cut was made perpendicular to the mechanical axis in the coronal plane and with 7° of posterior inclination along the sagittal plane; there were no bony defects noted along the eroded medial tibial plateau in any of these cases. Following each osteotomy, osteophytes were removed, and any ligament imbalances were corrected in the coronal plane by appropriately releasing soft tissues along the medial structures of the knee. In all knees with varus deformity, step by step appropriate release of medial side soft tissue (posteromedial capsule, MCL, semimembranosus and pes anserinus) was performed with a spacer block, in which residual lateral laxity was allowed to avoid joint line elevation.
Following each bony resection and soft tissue release, the tensor was fixed to the proximal tibia, and the femoral trial prosthesis was fitted. The joint distraction force was set at 40 lb in all patients. This distraction force was selected because it reproduces the joint gap in full extension with femoral trial, which corresponds to the insert thickness of our preliminary clinical studies. This joint distraction force was loaded several times until the joint component gap remained constant to reduce the error that can result from creep elongation of the surrounding soft tissues. At this point, the joint component gap (mm) and the varus ligament imbalance (°) were measured with the knee at 0° (full extension) and 90° (flexion) each with the patella laterally retracted (Fig. 1a) and then reduced (Fig. 1b). For each measurement with a reduced PF joint, the medial parapatellar arthrotomy was temporally repaired by applying stitches both proximally and distally to the connection arm of the tensor. During each measurement, the thigh and knee were aligned to eliminate the external load on the knee at each flexion angle.
Statistical analysis
The study aimed to include at least 39 participants in mini-TKA group and 19 participants in QS group, which was expected to yield power >0.8, based on α < 0.05 and assuming a large effect size (d = 0.80) using G power 3 http://www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3/.
After expressing each measurement as a mean ± standard error of the mean (SE), a statistical software package (Statview 5.0, Abacus Concepts Inc., Berkeley, CA) was utilized to analyse the data. The unpaired t test was selected to identify differences in joint component gap and varus imbalance between lateral patellar retraction and PF joint reduction and one-way analysis of variance (ANOVA) with Fisher’s least significant difference (LSD) post hoc test for comparison between the two techniques. In all analyses, P < 0.05 was accepted as statistically significant.
Results
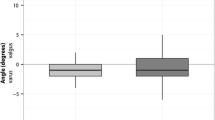
The joint component gap at extension showed no significant changes with patellar position in either TKA. However, the joint component gap at flexion significantly decreased at patellar retraction in both TKA. In addition, the joint component gap showed a significantly lower value at flexion with the retracted patella in QS TKA compared to mini-TKA (P < 0.05; Table 1).
Varus imbalance at extension showed no significant changes regardless of patellar position in both TKA. Whereas varus imbalance at flexion showed no significant changes regardless of patellar position in mini-TKA, there was a significant decrease at flexion when the patella was laterally retracted in QS TKA (P < 0.05). In addition, the varus imbalance showed a significantly lower value at flexion with the patella retracted in QS TKA compared to mini-TKA (Table 2).
Discussion
The most important finding of the present study was that the patellar positions influenced the soft tissue balance, and the amount of surgical exposure could be a significant factor for soft tissue balance at flexion in MIS TKA.
In the present study, the joint component gaps decreased at 90° flexion when the patella was laterally retracted in both QS and mini-TKA. Additionally, a significantly smaller joint gap was observed in QS TKA than in mini-TKA with a retracted patella at 90° of flexion. In MIS TKA, patellar retraction requires a higher lateral force on the patella especially at knee flexion due to its smaller surgical exposure. This is the reason that the lateral force tensed patellar tendon and quadriceps and the tension in the extensor mechanisms decreased the joint gap at flexion in both TKA. Additionally, a significant decrease in the joint gap in QS TKA compared to mini-TKA might have been caused by the higher tension in the extensor mechanisms in QS TKA than in mini-TKA caused by the difference in surgical exposures.
With varus/valgus balance, varus ligament imbalances were also smaller with the patella retracted than with the patella reduced at flexion in QS TKA, but not in mini-TKA. This also might result from the higher tension in the laterally retracted extensor mechanisms in QS TKA, which decreased the lateral compartment gap and resulted in the smaller varus imbalance.
Quite recently, our group’s study using the same tensor demonstrated that MIS QS TKA provided some difficulties in acquiring appropriate soft tissue balancing compared to conventional TKA [10]. In this report, due to limited working space, more varus imbalance was visible in MIS QS group compared to conventional group.
As previously reported, the decreases in the joint gap and varus ligament imbalance were caused by the PF joint reduction at 90° of flexion in conventional TKA [8]. It is suggested that the extensor mechanisms might be loosened because of its shorter running route during patellar eversion in conventional TKA. After the PF joint was reduced physiologically, the tension in the extensor mechanism as well as in the anterolateral structures including the retinaculum and iliotibial band was increased at the anterolateral aspect of the knee during knee flexion, resulting in the decrease in joint gap and varus ligament imbalance. In the same way, Yoshino et al. [22] reported that there was significant increase in load in the patella reset position compared to in the everted position in conventional PS TKA using their original tensor and speculated that the flexion gap distance would decrease by resetting the patella. Luring et al. [6] reported that eversion of the patella increased the valgus alignment measured by the navigation system in a cadaveric study. Gejo et al. [3] also reported that the patella tendon strain at 90° flexion correlated with the joint gap difference with patella position, and they suggested that the knee extensor mechanism may have influence on the joint gap. In the present study, however, the joint gap at 90° flexion in MIS TKA showed results contrary to those previously reported in conventional TKA. In MIS TKA, a smaller surgical exposure and lower damage to VMO compared to the conventional approach may need a higher external load on the extensor mechanism compared to those in conventional TKA when the patella is retracted or everted during soft tissue balance measurement. The varus imbalance at flexion was not changed by the patellar position in mini-TKA. Because the surgical exposure and laterally retracting force in mini-TKA were intermediate between conventional and QS TKA, lateral force and a shortened running route might neutralize each other during patella shift.
This study has some limitations. At first, although there were significant differences in several comparisons, the numbers of assigned patients in the two groups were not equal due to the variation of VMO attachment to the patella intra-operatively observed: There are only a small number of patients with a proximal VMO attachment of the patella, which indicates QS TKA, in the Japanese population [21]. Secondly, the amount of lateral retraction force and patella tendon strain was not evaluated and compared when the patella was laterally retracted. The other limitation in this study is that the tensor in its current design does not allow for knee rotation, so we are unable to estimate the influence of our intra-operative rotational alignment on the measurements.
Summarizing the results, the intra-operative patterns of soft tissue balance differ between the laterally retracted and reduced patella, as well as between QS and mini-TKA. The results indicate that surgeons performing conventional soft tissue balance evaluation with the patella laterally retracted in MIS TKAs are at a greater risk of underestimating the joint gap and varus ligament imbalance depending on the surgical exposure compared to the post-operative condition after TKA with the patella reduced.
Conclusion
The influence of surgical exposure on the joint gap and ligament balance during patella shift is important in minimal incision TKA. Therefore, soft tissue balance should be evaluated more accurately and consistently by maintaining a reduced PF joint for each intra-operative measurement.
References
Aglietti P, Baldini A, Giron F, Sensi L (2006) Minimally invasive total knee arthroplasty: is it for everybody? HSS J 2(1):22–26
Bathis H, Perlick L, Tingart M, Luring C, Perlick C, Grifka J (2004) Radiological results of image-based and non-image-based computer-assisted total knee arthroplasty. Int Orthop 28(2):87–90
Gejo R, Morita Y, Matsushita I, Sugimori K, Kimura T (2008) Joint gap changes with patellar tendon strain and patellar position during TKA. Clin Orthop Relat Res 466:946–951
Jenny JY, Boeri C (2001) Computer-assisted implantation of a total knee arthroplasty: a case-controlled study in comparison with classical instrumentation. Rev Chir Orthop Reparatrice Appar Mot 87(7):645–652
Laskin RS, Beksac B, Phongjunakorn A, Pittors K, Davis J, Shim JC, Pavlov H, Petersen M (2004) Minimally invasive total knee replacement through a mini-midvastus incision: an outcome study. Clin Orthop Relat Res 428:74–81
Luring C, Hufner T, Kendoff D, Perlick L, Bathis H, Grifka J, Krettek C (2006) Eversion or subluxation of patella in soft tissue balancing of total knee arthroplasty? Results of a cadaver experiment. Knee 13(1):15–18
Lutzner J, Krummenauer F, Wolf C, Gunther KP, Kirschner S (2008) Computer-assisted and conventional total knee replacement: a comparative, prospective, randomised study with radiological and CT evaluation. J Bone Joint Surg Br 90(8):1039–1044
Matsumoto T, Kuroda R, Kubo S, Muratsu H, Mizuno K, Kurosaka M (2009) The intra-operative joint gap in cruciate-retaining compared with posterior-stabilised total knee replacement. J Bone Joint Surg Br 91(4):475–480
Matsumoto T, Muratsu H, Kubo S, Matsushita T, Kurosaka M, Kuroda R (2011) Soft tissue tension in cruciate-retaining and posterior-stabilized total knee arthroplasty. J Arthroplasty 26(5):788–795
Matsumoto T, Muratsu H, Kubo S, Mizuno K, Kinoshita K, Ishida K, Matsushita T, Sasaki K, Tei K, Takayama K, Sasaki H, Oka S, Kurosaka M, Kuroda R (2011) Soft tissue balance measurement in minimal incision surgery compared to conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19(6):880–886
Matsumoto T, Muratsu H, Tsumura N, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2006) Joint gap kinematics in posterior-stabilized total knee arthroplasty measured by a new tensor with the navigation system. J Biomech Eng 128(6):867–871
Mizu-uchi H, Matsuda S, Miura H, Okazaki K, Akasaki Y, Iwamoto Y (2008) The evaluation of post-operative alignment in total knee replacement using a CT-based navigation system. J Bone Joint Surg Br 90(8):1025–1031
Muratsu H, Matsumoto T, Kubo S, Maruo A, Miya H, Kurosaka M, Kuroda R (2010) Femoral component placement changes soft tissue balance in posterior-stabilized total knee arthroplasty. Clin Biomech (Bristol, Avon) 25(9):926–930
Pang HN, Yeo SJ, Chong HC, Chin PL, Ong J, Lo NN (2011) Computer-assisted gap balancing technique improves outcome in total knee arthroplasty, compared with conventional measured resection technique. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-011-1483-3
Saragaglia D, Picard F, Chaussard C, Montbarbon E, Leitner F, Cinquin P (2001) Computer-assisted knee arthroplasty: comparison with a conventional procedure. Results of 50 cases in a prospective randomized study. Rev Chir Orthop Reparatrice Appar Mot 87(1):18–28
Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A (2003) Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br 85(6):830–835
Stulberg SD, Loan P, Sarin V (2002) Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am 84-A(Suppl 2):90–98
Swank M, Romanowski JR, Korbee LL, Bignozzi S (2007) Ligament balancing in computer-assisted total knee arthroplasty: improved clinical results with a spring-loaded tensioning device. Proc Inst Mech Eng H 221(7):755–761
Tanaka K, Muratsu H, Mizuno K, Kuroda R, Yoshiya S, Kurosaka M (2007) Soft tissue balance measurement in anterior cruciate ligament-resected knee joint: cadaveric study as a model for cruciate-retaining total knee arthroplasty. J Orthop Sci 12(2):149–153
Tria AJ Jr (2003) Advancements in minimally invasive total knee arthroplasty. Orthopedics 26(8 Suppl):s859–s863
Watanabe N, Narita W, Namura T, Ito H, Nishimura T, Kubo T (2008) Anatomical assessment of the vastus medialis oblique muscle in patients with osteoarthritis of the knee. J Arthroplasty 23(2):287–292
Yoshino N, Watanabe N, Watanabe Y, Fukuda Y, Takai S (2009) Measurement of joint gap load in patella everted and reset position during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 17(5):484–490
Acknowledgments
The authors acknowledge Janina Tubby for her assistance in preparation of this manuscript. The study presented here did not receive any funding and grant.
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oka, S., Muratsu, H., Matsumoto, T. et al. The influence of patellar position on soft tissue balance in minimal incision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20, 1064–1068 (2012). https://doi.org/10.1007/s00167-011-1642-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1642-6