Abstract
Purpose
The combination of chondrogenic factors might be necessary to adequately stimulate articular cartilage repair. In previous studies, enhanced repair was observed following transplantation of chondrocytes overexpressing human insulin-like growth factor I (IGF-I) or fibroblast growth factor 2 (FGF-2). Here, the hypothesis that co-overexpression of IGF-I and FGF-2 by transplanted articular chondrocytes enhances the early repair of cartilage defects in vivo and protects the neighbouring cartilage from degeneration was tested.
Methods
Lapine articular chondrocytes were transfected with expression plasmid vectors containing the cDNA for the Escherichia coli lacZ gene or co-transfected with the IGF-I and FGF-2 gene, encapsulated in alginate and transplanted into osteochondral defects in the knee joints of rabbits in vivo.
Results
After 3 weeks, co-overexpression of IGF-I/FGF-2 improved the macroscopic aspect of defects without affecting the synovial membrane. Immunoreactivity to type-I collagen, an indicator of fibrocartilage, was significantly lower in defects receiving IGF-I/FGF-2 implants. Importantly, combined IGF-I/FGF-2 overexpression significantly improved the histological repair score. Most remarkably, such enhanced cartilage repair was correlated with a 2.1-fold higher proteoglycan content of the repair tissue. Finally, there were less degenerative changes in the cartilage adjacent to the defects treated with IGF-I/FGF-2 implants.
Conclusion
The data demonstrate that combined gene delivery of therapeutic growth factors to cartilage defects may have value to promote cartilage repair. The results also suggest a protective effect of IGF-I/FGF-2 co-overexpression on the neighbouring articular cartilage. These findings support the concept of implementing gene transfer strategies for articular cartilage repair in a clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular cartilage has a limited reparative capacity. Cartilage defects in adults do not regenerate [27] and may predispose the affected joint to develop secondary osteoarthritis [25]. Among the many different clinical strategies to induce the formation of a cartilaginous repair tissue, autologous articular chondrocyte implantation (ACI) [1] is a therapeutic option particularly suited to repair large cartilage defects [17]. However, even with such an elaborate technique, the new tissue that forms does not completely resemble the original structure of the articular cartilage [2] and its long-term properties remain uncertain [17, 37]. Accordingly, novel strategies are needed to further enhance the structural and functional properties of the repair tissue [27].
Polypeptide growth factors regulate chondrogenesis [11] and may be applied as therapeutic agents [36]. In particular, insulin-like growth factor I (IGF-I) and fibroblast growth factor-2 (FGF-2) are potent candidates to enhance articular cartilage repair in vivo [4, 8, 9, 13, 15, 22]. IGF-I is anabolic for articular chondrocytes and stimulates the production of type-II collagen and proteoglycans, two key extracellular matrix proteins, in vitro [24] and in vivo [26, 36]. FGF-2 is mitogenic for articular chondrocytes in vitro [21], supports chondrogenesis [11] and enhances the repair of articular cartilage defects in vivo [31]. Yet, the experimental and clinical application of growth factors for articular cartilage repair is complicated by their short intraarticular half-life [30, 33]. Gene transfer of growth factor genes in cells or tissues that are transplanted into articular cartilage defects allows for a spatially defined overexpression of these therapeutic molecules over prolonged and clinically relevant periods of time [5, 6, 14, 15, 22].
In previous studies, single overexpression of human IGF-I or FGF-2 improved the repair of osteochondral defects in rabbits [15, 22]. Interestingly, transplantation of NIH 3T3 fibroblasts co-overexpressing IGF-I and FGF-2 led to accelerated repair after 3 weeks in vivo in a magnitude that was larger than when IGF-I was provided alone [23]. Yet, the histological repair score for single IGF-I treatment was inferior when NIH 3T3 fibroblasts were used instead of articular chondrocytes [15, 22], suggesting that chondrocytes might be of higher value for transplantation strategies applying genetically modified cells co-overexpressing a combination of growth factors.
This study tested the hypothesis that co-overexpression of IGF-I and FGF-2 by transplanted articular chondrocytes enhances the early repair of cartilage defects in vivo and protects the neighbouring cartilage from early osteoarthritic degeneration.
Materials and methods
The experimental set-up was similar than in previous studies to allow for a comparison [15, 22, 23]. This included the IGF-I and FGF-2 gene vectors with identical regulatory expression sequences (e.g. the cytomegalovirus immediate–early promoter/enhancer) [21, 24], articular chondrocytes obtained from male Chinchilla bastard rabbits (similar mean weight) from the same breeder (Charles River, Sulzfeld, Germany) [22], the alginate hydrogel for cell encapsulation [19], the animal model of an osteochondral defect, an identical 3-week time point of observation [15, 22], and the histological score system [32] for evaluation.
Materials
All reagents were obtained from Invitrogen/Gibco (Karlsruhe, Germany) unless otherwise indicated. Alginate, bovine testicular hyaluronidase, calf thymus DNA, L-Cystein and Na2ETDA were from Sigma (Munich, Germany), chondroitin-6-sulphate from Fluka (Buchs, Switzerland) and 1,9-dimethylmethylene blue from Serva (Darmstadt, Germany). Collagenase type I (activity: 232 U/mg) was purchased at Biochrom (Berlin, Germany). Plasticware was obtained from Falcon (Becton–Dickinson, Pont de Claix, France).
Articular chondrocyte culture and lipid-based transfection
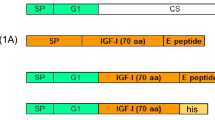
Articular cartilage was harvested from the knee and hip joints of three juvenile male Chinchilla bastard rabbits (mean weight: 1.8 ± 0.5 kg) as previously described [15, 22, 23]. Cell viability, as determined by trypan blue exclusion, always exceeded 90%. Cells were placed in monolayer culture in basal medium containing 10% foetal bovine serum (growth medium). Transfections were performed using expression plasmid vectors carrying either the E. coli lacZ gene sequence encoding for β-galactosidase (pCMVlacZ; termed lacZ-transfected) or a combination of human IGF-I (pCMVhIGF-I) and human FGF-2 cDNA (pCMVhFGF-2; termed IGF-I/FGF-2-transfected) placed under the control of the human cytomegalovirus immediate-early promoter/enhancer (CMV-IE) and the non-liposomal lipid formulation FuGENE 6 (v/w ratio 1:2; Roche Applied Sciences, Mannheim, Germany), as previously described [15, 19, 22, 29]. Transfection efficiency was determined by detection of β-galactosidase activity 36 h after transfections by X-Gal staining [20].
Encapsulation of transfected articular chondrocytes in alginate spheres
One day after transfection, the chondrocytes were encapsulated in alginate as previously described [15, 19, 22]. The resulting alginate implants containing lacZ- or IGF-I/FGF-2-transfected chondrocytes (termed lacZ or IGF-I/FGF-2 implants) were either transplanted in vivo or further examined in vitro [15, 19, 22].
Detection of cell viability and transgene expression
On days 0 and 21 post-encapsulation, the individual implants (n = 3 per time point and condition) were solubilised, the released cells were counted and viability was determined using a Neubauer chamber and trypan blue exclusion staining, based on 4 counts per sample, as previously described [15, 19, 22]. To measure the secretion of IGF-I and FGF-2 by the implants, conditioned medium was collected on days 0, 2, 4, 7, 14, and 21 post-encapsulation (n = 3 per time point and condition), and levels of IGF-I and FGF-2 were determined by ELISA (both R&D Systems, Wiesbaden, Germany) with detection limits of 26 pg/ml (IGF-I) and 3 pg/ml (FGF-2) essentially as previously described [15, 19, 22].
Transplantation of alginate implants into osteochondral cartilage defects in vivo
All animal procedures were approved by the Saarland Governmental Animal Care Committee, and the principles of laboratory animal care were followed. The transplantation of implants in vivo was performed at the day of encapsulation (1 day post-transfection) as previously described [15, 22, 23]. Briefly, seven female Chinchilla bastard rabbits (Charles River, Sulzfeld, Germany; mean weight: 2.9 ± 0.1 kg; seven joints per group) were anaesthetised, the knee joint was entered through a medial parapatellar approach and two cylindrical osteochondral defects were created in the patellar groove of each knee (n = 28 defects) with a burr (3.2 mm in diameter; Synthes, Umkirch, Germany). Implants from a single preparation were press-fit into the defects. The right and left knees alternatively received lacZ (n = 14 defects) or IGF-I/FGF-2 implants (n = 14 defects) in both defects of the same joint. To maximise exposure of the defects to loading, animals were allowed full activity immediately post-operatively.
Macroscopic assessment of the joints
Three weeks after implantation in vivo, the rabbits were euthanised with pentobarbital (150 mg/kg body weight; Merial, Hallbergmoos, Germany) and the knee joints were examined macroscopically. An inverse scoring system was developed, incorporating individual parameters for contracture, effusion and adhesion of the joint, synovialitis, osteophyte formation, colour and surface of the defect, integration with surrounding cartilage and filling of the defect (Table 1). The individual scores were combined, resulting in an average total score. Values range from 12 points (no signs of repair) to 0 points (normal articular cartilage). A total of 28 defects were scored.
Histological and immunohistochemical analyses
The distal femurs were retrieved, fixed in 4% phosphate-buffered formalin, trimmed, and decalcified. Paraffin-embedded frontal sections of the distal defects (5 μm) were stained with safranin O and haematoxylin and eosin (HE) according to routine histological protocols [16]. Type-II, type-I collagen and lacZ immunostaining was performed as previously described [15, 23] using a 1/50 dilution of a monoclonal mouse anti-type-II or type-I collagen IgG (Acris Antibodies, Hiddenhausen, Germany) and a biotinylated anti-mouse antibody (Vector Laboratories, Grünberg, Germany). To control for secondary immunoglobulins, sections were processed as earlier, except for the secondary antibody. Visualisation of the collagen network (collagen fibril birefringence, orientation and parallelism, i.e. anisotropy) within the repair tissue was performed on HE-stained histological sections using polarised light microscopy (BX-45, Olympus, Hamburg, Germany).
The synovial membrane was evaluated on HE-stained sections (Fig. 1) using a previously published scoring system [8]. The three categories in this system include villus thickening (fibrosis), villus architecture (blunting) and the presence of inflammatory cell infiltrates. Total point values range between 0 and 9 points. A total of 50 sections were scored by two investigators without knowledge of the treatment groups.
Microscopic evaluation of inflammatory and adverse reactions to the described treatment was performed on HE-stained histological sections of the synovial membrane as described by Fortier et al. [8]. Among the knee joints that received lacZ (a) or IGF-I/FGF-2 (b) implants, no significant differences in thickness or architecture of synovial villi and in the presence of inflammatory cell infiltrates were observed. Original magnification ×100, scale bars 0.2 mm (a, b)
Immunoreactivity to type-II collagen in the repair tissue was compared with that of the adjacent normal articular cartilage that served as a positive internal control. Immunoreactivity to type-I collagen in the repair tissue was compared with that of the subchondral bone adjacent to the normal articular cartilage that served as a positive internal control. A score was given to each knee joint—0: no immunoreactivity; 1: significantly weaker immunoreactivity; 2: moderately weaker immunoreactivity; 3: similar immunoreactivity; 4: stronger immunoreactivity compared with controls. Histological sections (n = 2–3 per defect and collagen type) were scored by two investigators blinded with regard to the treatment groups.
For the quantitative assessment of the repair tissue, serial histological sections of the distal femora were taken at 200-μm intervals. Sections within approximately 1.0 mm from the centre of the defect (n = 9–11 per defect) were analysed using the articular cartilage repair scoring system described by Sellers and co-workers [32] (Table 2) as previously described [4, 15, 22, 23]. A total of 140 sections were scored independently by two investigators without knowledge of the treatment groups. Inter-observer reliability was determined. Images of the cartilage defects were acquired using a solid-state CCD camera mounted on a BX-45 microscope (Olympus, Hamburg, Germany).
Degenerative changes in the articular cartilage adjacent to the defects were evaluated on safranin O-stained histological sections. A 3-mm area of normal articular cartilage adjacent to both integration sides (excluding the area of integration) was evaluated for changes in cellularity, clustering and safranin O staining intensity [28, 34]. The following point values were applied—0: severe hypocellularity and poor or no staining; 1: mild or moderate hypocellularity and slight staining; 2: normal cellularity, mild clusters and moderate staining; 3: normal cellularity, no clusters and normal staining.
The area occupied by the lacZ and IGF-I/FGF-2 alginate implants was measured on safranin O-stained serial histological sections of the distal femora that were taken at 400-mm intervals as previously described [23].
Proteoglycan content of the repair tissue in vivo
The entire repair tissue of the proximal defects was retrieved. To each sample, 100 μl papain solution (0.0125%) was added, following overnight incubation at 60°C. Proteoglycans were detected using the dimethylmethylene blue (DMMB) assay (detection limit: 0.2 μg) [7] as previously described [23].
Statistical analysis
Each test condition was performed in duplicate or triplicate for the in vitro characterisation experiments and with seven defects per group for the in vivo experiments. Differences in cell number, viability or proteoglycan content were compared between treatment and control groups using nested analysis of variance (ANOVA). To determine the sample size for the in vivo experiments, a standard deviation of 25% for the mean total score was estimated based on literature values for selected cartilage repair procedures. For a power of 80% (beta = 0.20) and a two-tailed alpha level of 0.05, a sample size of seven defects per group would have been sufficient to detect a mean difference of 5 points between the groups, assuming a pooled standard deviation of 2.5 points (effect size = 5/2.5 = 2.0, using the two-sample Student’s t-test; version 5.0, nQuery Advisor, Statistical Solutions, Saugus, MA, USA). To evaluate the histological grading of in vivo experiments, points for each category and total scores were compared between the two groups using a mixed general linear model with repeated measures (knees nested within the same animals). Differences in the proteoglycan contents of the retrieved tissues in vivo were identified by a paired t test on 6 degrees of freedom. To determine a possible correlation between the histological average total score and the proteoglycan contents of the repair tissue, the non-parametric Spearman’s rank correlation coefficient (Spearman’s ρ) was applied. Inflammatory responses, immunohistochemical analyses, macroscopic score and areas occupied by the implants were evaluated using ANOVA. Statistical analysis of the data was performed using the SPSS software package (version 12.0, SPSS Inc., Chicago, IL, USA). Data are expressed as mean ± 95% confidence interval (CI). A two-tailed P < 0.05 was considered statistically significant.
Results
Transfection efficiency and cell viability in vitro
Mean transfection efficiency was of 30.1 ± 4.1%, as noted by X-Gal staining, consistent with previous data [19, 22]. Cell viability was above 85% at the time of encapsulation in alginate in both groups. Over the time of in vitro cultivation, cell viability remained constant in the IGF-I/FGF-2 group (86.0 ± 1.4% by day 21) but decreased significantly following lacZ treatment (79.5 ± 0.7% by day 21; P < 0.05, n = 6).
Growth factor synthesis in vitro
At day 2 in vitro, IGF-I expression levels in the supernatants of IGF-I/FGF-2 implants were of 33.4 ± 1.8 ng/107 cells/24 h (n = 3) (Table 3). By day 7 after transfection, they declined to 15.9 ± 7.0 ng/107 cells/24 h but were still significant compared with control implants. Beyond this time point (days 14 and 21), IGF-I was not detectable in the supernatants of IGF-I/FGF-2 implants anymore. IGF-I was never detectable in supernatants of lacZ implants. The FGF-2 expression levels of IGF-I/FGF-2 implants were of 7.5 ± 1.1 ng/107 cells/24 h at day 2 in vitro (Table 3) and returned to baseline by day 7 (1.1 ± 1.0 ng/107 cells/24 h; P > 0.3 versus lacZ implants). FGF-2 concentrations in the supernatants of lacZ implants ranged between 0.0 ± 0.1 and 0.3 ± 0.5 ng/107 cells/24 h.
Macroscopic aspect after in vivo transplantation
After 3 weeks in vivo, there were no contractures, effusions, adhesions, synovialitis or osteophyte formations in any of the treated joints (Table 1). Colour and filling of the defects were significantly different (both P < 0.01), resulting in a 2.4-fold improvement in the average total score of defects receiving the IGF-I/FGF-2 implants compared with the lacZ-treated defects (1.6 ± 0.5 and 3.9 ± 0.7, respectively; P < 0.01).
Microscopic evaluation of the synovium in vivo
There was no significant difference in the thickness or architecture of synovial villi or in the presence of inflammatory cell infiltrates between knees receiving the IGF-I/FGF-2 (1.3 ± 1.0) or lacZ implants (1.7 ± 1.4) at 3 weeks (Table 4; Fig. 1).
Immunohistochemical detection of collagen synthesis and lacZ expression in vivo
The repair tissue was evaluated for the presence of type-I collagen as an indicator of fibrocartilage (Table 5; Fig. 5). Three weeks after transplantation, immunoreactivity to type-I collagen was significantly stronger in the repair tissue of defects that received lacZ implants (mean: 3.2) than in those where the IGF-I/FGF-2 implants were applied (mean: 2.0; P < 0.01). The new tissue was also analysed for the presence of type-II collagen, a major component of the extracellular matrix of hyaline articular cartilage (Table 5; Fig. 5). In the lacZ group, immunoreactivity to type-II collagen was inferior to that of the adjacent normal articular cartilage. Defects receiving IGF-I/FGF-2 implants exhibited slightly stronger immunoreactivity to type-II collagen (mean: 1.6) compared with those receiving lacZ implants (mean: 1.5; n.s.). After 3 weeks in vivo, lacZ expression was revealed by immunohistochemistry within lacZ implants but not within IGF-I/FGF-2 implants (Fig. 2).
Representative analysis of lacZ expression in alginate implants after 3 weeks in vivo. Transgene expression was detected by immunohistochemistry using a mouse anti-β-gal antibody (1:45) and a biotinylated secondary antibody in the cells of lacZ (a) and IGF-I/FGF-2 implants (b). Original magnification ×200, scale bars 0.1 mm
Polarised light microscopy of the repair tissue
Collagen fibrils within the repair tissue of defects receiving lacZ and IGF-I/FGF-2 implants were mainly oriented parallel to the joint surface, without reproducing a normal articular cartilage organisation. Similar to the data obtained by immunohistochemical analyses, birefringence (an indicator of collagen content) was weaker within the repair tissue than in the surrounding normal articular cartilage in both lacZ- and IGF-I/FGF-2-treated defects (Fig. 3). Birefringence in the subchondral bone was similar between the defect areas and the adjacent tissue, confirming a good reconstitution of the subchondral bone in both experimental groups.
Visualisation of the collagen network within the repair tissue using polarised light microscopy on HE-stained histological sections following transplantation of lacZ (a, c) and IGF-I/FGF-2 (b, d) implants. Birefringence caused by collagen fibrils within the subchondral bone (presumably mainly type-I collagen) is depicted in golden yellow, while birefringent collagen fibrils in the cartilaginous tissue (mainly located in the adjacent normal cartilage) are depicted in white. The subchondral bone was well reconstituted without regard to the treatment group, as displayed by high birefringence, while type-II collagen network was barely detectable after 3 weeks in vivo and orientated parallel to the surface. Images (c) and (d) are magnified views of (a) and (b), respectively. Original magnifications ×40 (a, b) and ×100 (c, d). Scale bars 1.0 mm (a, b) and 0.4 mm (c, d)
Evaluation of degenerative changes within the adjacent articular cartilage
There were significantly less degenerative changes in the cartilage adjacent to defects receiving IGF-I/FGF-2 implants (mean 1.4 ± 0.7) compared with defects receiving lacZ implants (1.9 ± 0.7; P < 0.01) (Table 6; Fig. 4).
Degenerative changes in the adjacent articular cartilage tissue were evaluated using a grading system [28] that includes single parameters of cellularity, staining intensity and cluster formation. The neighbouring cartilage demonstrated significantly decreased degeneration following IGF-I/FGF-2 treatment (a, c) when compared with lacZ implants (b, d). Original magnifications ×40 (a, b) and ×100 (c, d). Scale bars 0.8 mm (a, b) and 0.3 mm (c, d)
Histological evaluation and grading of articular cartilage repair in vivo
To evaluate the fate of the alginate spheres implants, the area occupied by them (excluding any ingrown tissue) was measured. No significant difference between the groups (lacZ implants: 1.41 ± 0.51 mm2; IGF-I/FGF-2 implants: 1.1 ± 0.51 mm2) was seen. Articular cartilage repair was next evaluated by two investigators using a previously published histological grading system for articular cartilage defects [32] (Table 2). Correlation coefficients (Spearman’s ρ) for inter-observer variability always exceeded 0.9. Combined gene transfer of IGF-I/FGF-2 (n = 7 joints) significantly improved the average individual scores of defect filling (2.6-fold), integration (1.2-fold), matrix staining (1.9-fold), cellular morphology (1.5-fold), architecture of defect (1.4-fold) and surface (1.3-fold), and subchondral bone formation (1.3-fold) compared with the lacZ implants (each P < 0.01) (Table 7). The average total score after 3 weeks in vivo was significantly (1.4-fold) improved for defects receiving the IGF-I/FGF-2 implants compared with those receiving lacZ implants (P < 0.01) (Table 7; Fig. 5).
Stimulation of articular cartilage repair in osteochondral defects 3 weeks after transplantation of genetically modified chondrocytes in vivo. Histological appearance of osteochondral defects following treatment with lacZ (a, c, e, g, i, l) or IGF-I/FGF-2 implants (b, d, f, h, k, m) stained with safranin O (a–d), haematoxylin and eosin (HE) (e–h), a monoclonal mouse anti-human type-I collagen IgG (i, k) or a monoclonal mouse anti-human type-II collagen IgG (l, m). Panels (c, d) and (g, h) are magnified views of (a, b) and (e, f), respectively. Safranin O staining is increased in defects receiving an IGF-I/FGF-2 implant (b, d) compared with defects receiving lacZ implants (a, c). Cells in the repair tissue of the IGF-I/FGF-2 defects were round, had round nuclei and were oriented in a columnar fashion (d, h). Immunoreactivity to type-I collagen was increased in the repair tissue of defects receiving lacZ implants (i), whereas immunoreactivity to type-II collagen was elevated in defects receiving IGF-I/FGF-2 implants (m). Sections were taken from defects having a histological rating equal to the mean score for its respective treatment group. Photomicrographs were obtained using standardised photographic parameters, including light intensity. Original magnifications ×20 (a, b, e, f), ×40 (i–m) or ×100 (c, d, g, h). Scale bars 2.0 mm (a, b, e, f), 0.6 mm (i–m) and 0.6 mm (c, d, g, h)
Proteoglycan contents of the repair tissue in vivo
Defects treated with IGF-I/FGF-2 implants contained 2.1-fold more proteoglycans compared with lacZ-treated defects (6.3 ± 2.4 vs. 3.0 ± 1.3 μg/mg dry weight, respectively; n = 7; P = 0.02) (Fig. 6). A statistical analysis revealed a correlation between the average total histological score and the proteoglycan contents of the repair tissue (Spearman’s ρ = −0.6, P = 0.02), suggesting that an improved overall histological aspect of the repair tissue is associated with a higher individual proteoglycan content.
Discussion
The most important findings of the present study were the enhanced cartilage repair by combined gene transfer of IGF-I/FGF-2 in vivo, the good correlation between histological and biochemical parameters of the repair tissue, and the absence of degenerative changes within the neighbouring articular cartilage.
Both IGF-I and FGF-2 are known to enhance cartilage repair following single overexpression [15, 22] or application as recombinant proteins [35]. The present study is a direct continuation of previous investigations applying IGF-I or FGF-2 as single genes [15, 22] or when transplanting alginate spheres based on NIH 3T3 fibroblasts co-overexpressing either IGF-I/FGF-2 or IGF-I alone [23]. Interestingly, when NIH 3T3 fibroblasts were selected as a more easily accessible cell source, transplantation of co-transfected IGF-I/FGF-2 implants improved articular cartilage repair after 3 weeks in vivo in a magnitude that was larger than with IGF-I alone or when compared with lacZ implants [23]. In the present study, transplantation of chondrocytes overexpressing IGF-I/FGF-2 significantly improved articular cartilage repair for all individual categories of the applied histological grading system (except for tidemark formation) including the subchondral bone as well as the resulting average total score, in good agreement with previous data [15, 22]. However, a synergistic effect of the combined IGF-I/FGF-2 gene transfer versus application of IGF-I [22] or FGF-2 [15] alone is not displayed by the average cartilage repair score in vivo. The previously published studies on single overexpression [15, 22] were used as historical controls rather than including 14 additional animals for single overexpression of IGF-I and FGF-2 (n = 7 each) in the present study, because the cartilage repair score of the negative controls (the contralateral knees) always had similar values [15, 22]. Factors of the experimental set-up that remained constant between these and the present study, including the ~30% transfection efficiencies [15, 19, 22, 23], the gene vectors, the animal source, their age and the osteochondral defect model, control group and identical histological evaluation after the same observation period of 3 weeks. Taking in account that transfection efficiency may vary between individual transfections, chondrocytes were co-transfected with IGF-I and FGF-2, rather than applying a pool of chondrocytes individually transfected with either IGF-I or FGF-2 as a mean to ascertain the presence of both genes within the transplanted cells. Since articular chondrocytes from juvenile animals were used, it remains to be seen whether transplanted adult lapine chondrocytes will yield similar results.
IGF-I and FGF-2 secretion of the implants was elevated for at least 7 days in vitro, shorter than the reported 21-day period with NIH 3T3 fibroblasts for a combined IGF-I/FGF-2 overexpression [23], the 28-day period noted with articular chondrocytes for single FGF-2 overexpression [15] and the 36-day period for single IGF-I overexpression [22]. However, the recombinant lacZ protein was detected within lacZ implants at 3 weeks in vivo. Chondrocytes in the IGF-I/FGF-2 implants employed here secreted a maximum of 273.7 pg IGF-I/implant/24 h and of 69.9 pg FGF-2/implant/24 h, compared with 631.8 pg IGF-I/implant/24 h and 210.7 pg FGF-2/implant/24 h in chondrocytes reported previously [15, 22]. NIH 3T3 fibroblasts initially secreted 2,186.7 pg IGF-I/implant/24 h and 276.0 pg FGF-2/implant/24 h [23]. This suggests that duration and levels of transgene expression affect cartilage repair. Interestingly, a low dose of 1 ng/ml FGF-2 stimulated IGF-I-mediated articular chondrocyte proliferation in vitro, whereas higher doses (50, 100 ng FGF-2/ml) inhibit the anabolic activity of IGF-I [18].
The proteoglycan content of the repair tissue was significantly elevated in the IGF-I/FGF-2 group and correlated significantly with the histological data, supporting the validity of the applied histological grading system. As IGF-I (rather than FGF-2) is known to enhance the production of extracellular matrix components such as type-II collagen, proteoglycan and aggrecan [36], this finding is in good agreement with previous data [9, 12, 22].
Early osteoarthritic changes within the cartilage adjacent to the defect were significantly reduced following combined gene transfer of IGF-I/FGF-2. Although the influence of growth factor overexpression approaches on the development and progression of osteoarthritis is not yet clarified [10], this finding is consistent with previous studies demonstrating the beneficial effect of IGF-I to maintain the cartilage structure [30] and of FGF-2 to delay cartilage degradation in osteoarthritis [3]. Whether this protective effect on of the neighbouring cartilage is the result of paracrine effects of IGF-I and/or FGF-2 or can be explained by the better mechanical support of the improved repair tissue remains to be elucidated.
Limitations of this study include the uncertainty regarding the fate of the transplanted cells as well as the origin of those re-populating the defects. Additional measures to further improve cartilage repair—e.g. other combinations of therapeutic factors or novel gene transfer systems allowing for a longer duration of transgene expression—will have to be determined. Future research may also need to focus on long-term evaluations of the repair tissue in this model and to be performed in a larger animal model of articular cartilage repair.
Taken together, these findings support the concept of implementing gene transfer strategies for articular cartilage repair in a clinical setting.
Conclusion
The most important findings of the present study are the enhanced cartilage repair by combined ex vivo gene delivery of IGF-I/FGF-2 via alginate-embedded and transplanted articular chondrocytes, the good correlation between histological and biochemical parameters of cartilage repair and the protection of the neighbouring cartilage from early osteoarthritic changes.
References
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Buckwalter JA, Mankin HJ (1998) Articular cartilage repair and transplantation. Arthritis Rheum 41:1331–1342
Chia SL, Sawaji Y, Burleigh A, McLean C, Inglis J, Saklatvala J, Vincent T (2009) Fibroblast growth factor 2 is an intrinsic chondroprotective agent that suppresses ADAMTS-5 and delays cartilage degradation in murine osteoarthritis. Arthritis Rheum 60:2019–2027
Cucchiarini M, Madry H, Ma C, Thurn T, Zurakowski D, Menger MD, Kohn D, Trippel SB, Terwilliger EF (2005) Improved tissue repair in articular cartilage defects in vivo by rAAV-mediated overexpression of human fibroblast growth factor 2. Mol Ther 12:229–238
Evans CH, Ghivizzani SC, Smith P, Shuler FD, Mi Z, Robbins PD (2000) Using gene therapy to protect and restore cartilage. Clin Orthop Relat Res 379(Suppl):S214–S219
Evans CH, Liu FJ, Glatt V, Hoyland JA, Kirker-Head C, Walsh A, Betz O, Wells JW, Betz V, Porter RM, Saad FA, Gerstenfeld LC, Einhorn TA, Harris MB, Vrahas MS (2009) Use of genetically modified muscle and fat grafts to repair defects in bone and cartilage. Eur Cell Mater 18:96–111
Farndale RW, Buttle DJ, Barrett AJ (1986) Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta 883:173–177
Fortier LA, Mohammed HO, Lust G, Nixon AJ (2002) Insulin-like growth factor-I enhances cell-based repair of articular cartilage. J Bone Joint Surg Br 84:276–288
Gelse K, von der Mark K, Aigner T, Park J, Schneider H (2003) Articular cartilage repair by gene therapy using growth factor-producing mesenchymal cells. Arthritis Rheum 48:430–441
Goldring MB, Goldring SR (2007) Osteoarthritis. J Cell Physiol 213:626–634
Goldring MB, Tsuchimochi K, Ijiri K (2006) The control of chondrogenesis. J Cell Biochem 97:33–44
Goodrich LR, Hidaka C, Robbins PD, Evans CH, Nixon AJ (2007) Genetic modification of chondrocytes with insulin-like growth factor-1 enhances cartilage healing in an equine model. J Bone Joint Surg Br 89:672–685
Hidaka C, Goodrich LR, Chen CT, Warren RF, Crystal RG, Nixon AJ (2003) Acceleration of cartilage repair by genetically modified chondrocytes over expressing bone morphogenetic protein-7. J Orthop Res 21:573–583
Ivkovic A, Pascher A, Hudetz D, Maticic D, Jelic M, Dickinson S, Loparic M, Haspl M, Windhager R, Pecina M (2010) Articular cartilage repair by genetically modified bone marrow aspirate in sheep. Gene Ther 17:779–789
Kaul G, Cucchiarini M, Arntzen D, Zurakowski D, Menger MD, Kohn D, Trippel SB, Madry H (2006) Local stimulation of articular cartilage repair by transplantation of encapsulated chondrocytes overexpressing human fibroblast growth factor 2 (FGF-2) in vivo. J Gene Med 8:100–111
Kiernan JA (1999) Histological and Histochemical Methods—Theory and Practice. Butterworth-Heinemann, Oxford
Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, Roberts S, Solheim E, Strand T, Johansen O (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 89:2105–2112
Loeser RF, Chubinskaya S, Pacione C, Im HJ (2005) Basic fibroblast growth factor inhibits the anabolic activity of insulin-like growth factor 1 and osteogenic protein 1 in adult human articular chondrocytes. Arthritis Rheum 52:3910–3917
Madry H, Cucchiarini M, Stein U, Remberger K, Menger MD, Kohn D, Trippel SB (2003) Sustained transgene expression in cartilage defects in vivo after transplantation of articular chondrocytes modified by lipid-mediated gene transfer in a gel suspension delivery system. J Gene Med 5:502–509
Madry H, Cucchiarini M, Terwilliger EF, Trippel SB (2003) Recombinant adeno-associated virus vectors efficiently and persistently transduce chondrocytes in normal and osteoarthritic human articular cartilage. Hum Gene Ther 14:393–402
Madry H, Emkey G, Zurakowski D, Trippel SB (2004) Overexpression of human fibroblast growth factor 2 stimulates cell proliferation in an ex vivo model of articular chondrocyte transplantation. J Gene Med 6:238–245
Madry H, Kaul G, Cucchiarini M, Stein U, Zurakowski D, Remberger K, Menger MD, Kohn D, Trippel SB (2005) Enhanced repair of articular cartilage defects in vivo by transplanted chondrocytes overexpressing insulin-like growth factor I (IGF-I). Gene Ther 12:1171–1179
Madry H, Orth P, Kaul G, Zurakowski D, Menger MD, Kohn D, Cucchiarini M (2010) Acceleration of articular cartilage repair by combined gene transfer of human insulin-like growth factor I and fibroblast growth factor-2 in vivo. Arch Orthop Trauma Surg 130:1311–1322
Madry H, Zurakowski D, Trippel SB (2001) Overexpression of human insulin-like growth factor-I promotes new tissue formation in an ex vivo model of articular chondrocyte transplantation. Gene Ther 8:1443–1449
Martin JA, Brown T, Heiner A, Buckwalter JA (2004) Post-traumatic osteoarthritis: the role of accelerated chondrocyte senescence. Biorheology 41:479–491
Nixon AJ, Fortier LA, Williams J, Mohammed H (1999) Enhanced repair of extensive articular defects by insulin-like growth factor-I-laden fibrin composites. J Orthop Res 17:475–487
O’Driscoll SW (1998) The healing and regeneration of articular cartilage. J Bone Joint Surg Am 80:1795–1812
O’Driscoll SW, Keeley FW, Salter RB (1986) The chondrogenic potential of free autogenous periosteal grafts for biological resurfacing of major full-thickness defects in joint surfaces under the influence of continuous passive motion. An experimental investigation in the rabbit. J Bone Joint Surg Am 68:1017–1035
Orth P, Weimer A, Kaul G, Kohn D, Cucchiarini M, Madry H (2008) Analysis of novel nonviral gene transfer systems for gene delivery to cells of the musculoskeletal system. Mol Biotechnol 38:137–144
Rogachefsky RA, Dean DD, Howell DS, Altman RD (1993) Treatment of canine osteoarthritis with insulin-like growth factor-1 (IGF-1) and sodium pentosan polysulfate. Osteoarthritis Cartilage 1:105–114
Schofield JN, Wolpert L (1990) Effect of TGF-beta 1, TGF-beta 2, and bFGF on chick cartilage and muscle cell differentiation. Exp Cell Res 191:144–148
Sellers RS, Peluso D, Morris EA (1997) The effect of recombinant human bone morphogenetic protein-2 (rhBMP-2) on the healing of full-thickness defects of articular cartilage. J Bone Joint Surg Am 79:1452–1463
Shida J, Jingushi S, Izumi T, Iwaki A, Sugioka Y (1996) Basic fibroblast growth factor stimulates articular cartilage enlargement in young rats in vivo. J Orthop Res 14:265–272
Solchaga LA, Yoo JU, Lundberg M, Dennis JE, Huibregtse BA, Goldberg VM, Caplan AI (2000) Hyaluronan-based polymers in the treatment of osteochondral defects. J Orthop Res 18:773–780
Tanaka H, Mizokami H, Shiigi E, Murata H, Ogasa H, Mine T, Kawai S (2004) Effects of basic fibroblast growth factor on the repair of large osteochondral defects of articular cartilage in rabbits: dose-response effects and long-term outcomes. Tissue Eng 10:633–641
Trippel SB (1997) Growth factors as therapeutic agents. Instr Course Lect 46:473–476
Vasiliadis HS, Danielson B, Ljungberg M, McKeon B, Lindahl A, Peterson L (2010) Autologous chondrocyte implantation in cartilage lesions of the knee: long-term evaluation with magnetic resonance imaging and delayed gadolinium-enhanced magnetic resonance imaging technique. Am J Sports Med 38:943–949
Acknowledgments
Supported by the Deutsche Forschungsgemeinschaft (DFG MA 2363/1-2 to H.M.). The authors thank E. Kabiljagic and E. Gluding for expert technical assistance.
Conflict of interest
The authors declare no competing financial interests. The authors, their immediate families and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orth, P., Kaul, G., Cucchiarini, M. et al. Transplanted articular chondrocytes co-overexpressing IGF-I and FGF-2 stimulate cartilage repair in vivo. Knee Surg Sports Traumatol Arthrosc 19, 2119–2130 (2011). https://doi.org/10.1007/s00167-011-1448-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1448-6