Abstract
Purpose
The purpose of this study was to investigate the clinical results of anatomical reconstruction of anterior inferior tibiofibular ligament (AITFL) for the chronic tibiofibular syndesmotic disruption after typical pronation external rotation (PER) stage 4 injury.
Methods
Six consecutive patients with chronic syndesmotic disruption after PER stage 4 injury were surgically treated. In all six patients, preoperative CT revealed remarkable opening of only the anterior part of the distal tibiofibular joint, and all six underwent anatomical reconstruction of the AITFL using autogenous gracilis tendon after confirmation of preserved tension of the posterior inferior tibiofibular ligament through intra-operative arthroscopic examination. Clinical evaluation was made using the American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Scale (AOFAS)and visual analogue scale (VAS) just before reconstructive surgery and at the most recent follow-up (median: 38 months, range, 31–50).
Results
Median AOFAS score improved from preoperative 53 points (range, 47–74) to postoperative 95 points (range, 90–100) (P < 0.05), and median VAS score improved from preoperative 95 points (range, 55–100) to postoperative 4 points (range, 0–14) (P < 0.05).
Conclusions
The procedure, which can achieve anatomical reconstruction of the AITFL easily, seems to be one possible treatment for chronic disruption of the distal tibiofibular syndesmosis after PER stage 4 injury including avulsion fracture of the posterior malleolus, which is most common in this type of injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been reported that pronation external rotation (PER) stage 4 injury according to the Lauge-Hansen classification brings about the worst prognosis in rotational injury of the ankle because of high complication rate of the distal tibiofibular syndesmosis disruption [2]. Most cases with PER stage 4 injury include avulsion fracture of posterior malleolus and are rarely accompanied by rupture of the posterior inferior tibiofibular ligament (PITFL) [3], and if the typical type of this injury is treated initially only in consideration of adequate bony consolidation of fractures, a possible pattern of residual disruption is supposed as a remarkable opening of only the anterior part of the syndesmosis. The main cause of this pattern is thought to be rotation of distal fibula with or without malrotation, due to a disruption of the anterior tibiofibular ligament (AITFL). In such condition, fibular attachment of intact PITFL acts as a pivot for this rotation after consolidation of the posterior malleolar fracture. In this pattern, reconstruction of the anterior stabilizer is necessary to protect against recurrence of anterior opening after achievement of the anatomical position.
The purpose of this study was to investigate the clinical results of anatomical reconstruction of AITFL using autogenous gracilis tendon for chronic disruption of the distal tibiofibular syndesmosis after PER stage 4 injury with residual remarkable opening of the anterior part.
Methods
Between 2004 and 2007, six consecutive patients who sustained chronic disruption of the distal tibiofibular syndesmosis rotational ankle fracture were surgically treated in our institution. There were five men and one woman with the median age of 23 years (range, 19–56) at the time of surgery, and all patients were introduced to our institution for the treatment of unsolved persistent pain after initial treatment. All patients had previous rotational ankle fracture, which were all confirmed as PER stage 4 injury according to the Lauge-Hansen classification by radiographs taken at their practitioners immediately after initial injury. There are descriptive data of 6 patients in Table 1.
In all patients, physical examination at initial visit to our institution revealed swelling and pain to palpation on the anterolateral aspect of their ankles, and the range of motion of the joint was restricted especially in dorsiflexion. All patients were diagnosed with disruption of the distal tibiofibular syndesmosis by radiographs taken at our institution (Fig. 1). Furthermore, computed tomography (CT) was performed to access inaccuracy of the distal tibiofibular joint by comparing with unaffected side, and all patients revealed remarkable opening of only the anterior part in the distal tibiofibular joint due to rotation of distal fibula (Fig. 2).
For all 6 patients, our reconstructive surgery was performed at a median of 12 months (range, 10– 27 months) after initial injury (Table 1).
Procedure
At first, we performed arthroscopic examination for all patients to evaluate intra-articular disorder. Disrupted AITFL with interposition of fibrous scar tissue in the anterior aspect of the distal tibiofibular joint and preserved tension of the PITFL after consolidation of avulsion fracture of posterior malleolus was confirmed arthroscopically in all patients (Fig. 3).
Next, the distal fibula and distal tibiofibular joint was exposed through direct lateral approach, and aggressive debridement of fibrous scar tissue in the distal tibiofibular joint was performed. Anatomical reduction of distal fibula into the incisura of distal tibia could be achieved in 3 patients by debridement alone, but the remaining 3 patients needed linear osteotomy of the fibula at the level of 8 cm proximal from distal fibular tip to achieve anatomical reduction. After anatomical reduction of the distal tibiofibular joint was achieved, syndesmosis fixation was performed using 3.5-mm cannulated cancellous screw for all 6 patients. Thereafter, fibular plating was performed for 3 patients with fibular osteotomy using a locking plate system (3.5 mm LCP plate; Synthes, Bettlach, Switzerland).
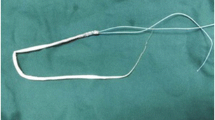
Finally, reconstruction of AITFL was performed with autogenous gracilis tendon using interference screws. The gracilis tendon of the ipsilateral knee was harvested, and an autogenous tendon with 140 mm length was folded over itself twice to manufacture into a tendon graft. Two bone tunnels were created at the proximal and distal attachment of AITFL with a diameter of 5.5 mm and a depth of 25 mm, and each 20-mm end of the graft was introduced into each bone tunnel, and pieces of the cancellous bone harvested when the bone tunnels were created were used to fill in each bone tunnel for protection of the graft from direct injury caused by thread of the interference screw [6]. Each bony attachment of the graft was fixed with an interference screw with a diameter of 5 mm (Tendon-Junction screw, Meira Co. Ltd.) (Figs. 4, 5).
Plain radiograph immediately after surgery in same case as Fig. 1
Postoperative regimen
A splint was applied until wound healing, and active range of motion exercises was allowed immediately after removal of splint. At 4 weeks after surgery, partial weight bearing was allowed, and the patients advanced to full weight bearing at their own rates.
Evaluation
The clinical evaluation was made using the American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Scale (AOFAS) and visual analogue scale (VAS).
Statistical analysis
Paired data analysis correlated with the clinical evaluation was done to compare the preoperative and postoperative score improvement. Comparisons of the results before reconstructive surgery and at the most recent follow-up in the AOFAS and VAS scores were made by Wilcoxon signed rank test. Differences were considered statistically significant when P was less than or equal to 0.05(0.05 ≥ P).
Results
The median follow-up period after surgery was 38 months (range: 31–50). The median AOFAS score at the most recent follow-up was 95 points (range, 90– 100), which was significantly higher (P < 0.05) than before surgery (53 points; range, 47–74). Also, the median VAS score at most recent follow-up was 4 points (range, 0–14), which was significantly lower (P < 0.05) than before surgery (95 points; range, 55–100). There was no complication of surgery.
Discussion
The most important finding of the present study was that the chronic disruption of the distal tibiofibular syndesmosis after the PER stage 4 injury with residual remarkable opening of the anterior part could be successfully treated by anatomical reconstruction of AITFL using autogenous gracilis tendon. The common characteristic of all our chronic cases after PER stage 4 injury was that opening was confirmed only at the anterior part of the distal tibiofibular joint and that there was no opening at the posterior part by preoperative CT. Analysis of this common pattern confirmed by CT permitted us to recognize that typical residual disruption of the distal tibiofibular syndesmosis after PER stage 4 injury was only a remarkable opening of the anterior part, if this injury is treated initially only in consideration of bony consolidation of fractures. The main cause of this pattern is considered to be rotation of distal fibula with or without malrotation, due to disruption of AITFL. In such condition, fibular attachment of intact PITFL acts as a pivot for this rotation after consolidation of the posterior malleolar fracture. In fact, preserved tension of the PITFL after consolidation of the posterior malleolar fracture was confirmed arthroscopically in all of our patients, and we logically considered the necessity of an anatomical reconstruction for only an AITFL for such cases.
Morris et al. [4] described a reconstruction technique using an autogenous hamstring graft and averred a necessity to reconstruct the interosseous ligament (IOL) because some investigators have considered it to be the primary bond between the tibia and fibula [1, 5]. Although reconstruction of this ligament may be effective for the chronic disruption with anterior and posterior opening which results from severe malunion after rotational ankle fracture, there is no sufficient evidence to confirm that this ligament must be reconstructed for such cases as those in the present study with only an anterior opening. Furthermore, anatomical reconstruction of this ligament is difficult to perform because both anatomical insertions cannot be confirmed directly through surgical approach.
There were some limitations in our study. It was a retrospective case series without controls. We could not make exact comparison of the surgical results with other surgical methods. Another limitation was the limited sample number. Evaluation of a large sample of chronic syndesmosis disruption after PER stage 4 injury is necessary to establish typical patterns of syndesmosis disruption, and randomized controlled study with large sample number is also needed in the future. However, presented procedure seems to be one possible treatment for chronic disruption of the distal tibiofibular syndesmosis after PER stage 4 injury including avulsion fracture of the posterior malleolus, which is most common in this type of injury, with future studies.
Conclusions
This procedure, which can achieve anatomical reconstruction of the AITFL easily, seems to be one possible treatment for chronic disruption of the distal tibiofibular syndesmosis after PER stage 4 injury including avulsion fracture of the posterior malleolus, which is most common in this type of injury. However, the results of this study should be confirmed by randomized controlled study with large sample number in the future.
References
Hoefnagels EM, Waites MD, Wing ID, Belkoff SM, Swierstra BA (2007) Biomechanical comparison of the interosseous tibiofibular ligament and the anterior tibiofibular ligament. Foot Ankle Int 28:602–604
Joy G, Patzakis MJ, Harvey JPJR (1974) Precise evaluation of the reduction of severe ankle fractures. J Bone Joint Surg Am 56:979–993
Kelikian H, Kelikian AS (1985) Disorders of the ankle. WB Saunders, Philadelphia
Morris MW, Rice P, Schneider TE (2009) Distal tibiofibular syndesmosis reconstruction using a free hamstring autograft. Foot Ankle Int 30:506–511
Rammelt S, Zwipp H, Grass R (2008) Injuries to the distal tibiofibular syndesmosis:an evidence-based approach to acute and chronic lesions. Foot Ankle Clin N Am 13:611–633
Takao M, Oae K, Uchio Y, Ochi M, Yamamoto H (2005) Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: a new technique using an interference fit anchoring system. Am J Sports Med 33:814–823
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yasui, Y., Takao, M., Miyamoto, W. et al. Anatomical reconstruction of the anterior inferior tibiofibular ligament for chronic disruption of the distal tibiofibular syndesmosis. Knee Surg Sports Traumatol Arthrosc 19, 691–695 (2011). https://doi.org/10.1007/s00167-010-1311-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1311-1