Abstract
Controversy still exists regarding which cementation technique of the tibial component is preferable. Full cementation showed excellent long-term outcomes, and surface cementation with fixed-bearing designs provided excellent mid-term results. Concerns have been expressed about possible rotary forces to the tibial rotating platform, when the tibial stem remains cementless, with the risk of early loosening. The purpose of this study was to evaluate the rate of early loosening and radiolucency lines in 70 consecutive unidirectional rotating platform, posterior stabilized, total knee arthroplasties, using surface cementation. Multivariate analysis was performed to identify any correlations between early loosening or radiolucency lines and clinically relevant covariates: age, sex, BMI, follow-up time, cement penetration, radiolucencies, tibial slope, femoral flexion, frontal alignment, pre-operative and post-operative Knee Scores. The tibial plateau was divided into four zones in antero-posterior view and into two zones in lateral view, and the cement penetration was evaluated in each zone. The mean follow-up was 43 months (SD 14), and the average patients’ age was 73 (SD 7). The Knee Score averaged 91 (SD 8) and the Function score 86 (SD 17) at last follow-up visit. The cement penetration was >2 mm in all zones. No early loosening was detected, but in five asymptomatic patients (7%) radiolucency was noted around the tibial stem. The presence of radiolucent lines was not correlated with any of the covariates. The rate of early loosening and radiolucency lines with mobile tibial tray and surface cementation is comparable to other studies using different cementation techniques or surface cementation combined with fixed platform total knee arthroplasties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A stable primary fixation is one of the most important factors influencing the longevity of a total knee arthroplasty (TKA) [14]. Nevertheless, the most reliable cement fixation technique for the tibial component is still controversial. Proponents of full cementation of the tibial component (cementation of both undersurface and stem) state that this technique provides better short- and long-term fixation [9, 12]. On the other hand, advocates of surface or hybrid cementation (cementation of the undersurface only) and press-fitting of the tibial stem state that a sufficient implant stability is achieved, with decreased metaphyseal bone loss in case of revision and without the potential stress shielding effect [18, 21, 22].
The surface cementation technique demonstrated excellent mid-term results, when using fixed-bearing devices [9], and biomechanical properties comparable to full cementation technique, most of all when the undersurface cement mantle is around 3 mm [3, 9, 10, 18, 25].
Mobile-bearing tibial components were designed to reduce polyethylene wear and stresses across fixation interfaces [4]. Nevertheless, very little is known about the use of combined surface cementation and rotating-platform devices. Mobile-bearing designs showed in vitro a higher micromotion rate when fixed with hybrid technique compared to full cementation [14] and concerns have been expressed about possible early loosening in vivo, but no clinical outcomes are reported in the literature. Aseptic failure of tibial component fixation occurring within 2 years from the first implant is considered as early loosening [9, 16].
The starting hypothesis of this clinical study was that, with mobile-bearing TKAs and surface cementation, the rate of early loosening and radiolucency lines around the tibial tray would have been comparable to other designs and fixation techniques. Every correlation between early loosening or radiolucency lines and clinically relevant covariates was investigated to determine the risk factors for these conditions.
Materials and methods
Between 2003 and 2005, 70 consecutive primary total knee replacements with unidirectional rotating platform (URP) posterior stabilized (PS) TKAs (NexGen® Complete Knee Solution Legacy® Posterior Stabilized Mobile-Bearing Knee, Zimmer, Inc, Warsaw, IN) were performed in 62 patients. Forty-two patients were women, and twenty were men. The average patients’ age at surgery was 73 (range 55–85, SD 7). The average body mass index (BMI) was 25.8 (SD 5.3). The mean follow-up was 43 months (range 37–61, SD 14). The diagnosis was primary osteoarthritis in 59 knees (84%); primary osteoarthritis (previously subjected to osteotomy) in 3 knees (4%); post-traumatic arthritis in 4 knees (6%); rheumatoid arthritis in 4 knees (6%). Coronal deformity was varus in 53 (76%) knees, valgus in 8 (11%), while 9 (13%) knees presented preoperative neutral alignment. A surface tibial cementation technique with stem press-fitting was used in all the cases.
Cementation technique
The NexGen-LPS URP (Zimmer, Warsaw, IN) was used in all patients, without patellar resurfacing.
The tourniquet was inflated after bone cut executions, soft tissue balancing and trial components positioning. A pulsatile lavage was performed to avoid excessive bleeding during the cementation phase. Once the appropriate consistency and viscosity (usually 5–6 min after mixing) was achieved, the cement (Cemex System, Tecres Spa, Italy) was placed directly on the undersurface of the tibial (not on the stem) and femoral components, with small amount on the posterior condyles.
An oval-shaped amount of cement was positioned on the tibial surface, and digital compression was used to force the cement into the cancellous bone. The tibial component was impacted in place, and the cement exceeding was carefully removed.
A horseshoe-shaped piece of cement was placed over the anterior and distal surface of the prepared femur, and digital compression was used as previously described. The femoral component was then impacted. Then, the trial insert was positioned, and the knee was kept in extension until the complete polymerization of the cement, while copious saline lavages were performed. After having checked the absence of loose cement bodies, the polyethylene tray was implanted and the tourniquet deflated.
All patients followed the same post-operative rehabilitation protocol, starting continuous passive motion (CPM) the day after surgery and beginning full weight bearing as tolerated 2 days after surgery. CPM was continued for 3 weeks post-operatively.
All patients were followed prospectively and evaluated clinically and radiographically at 3 and 6 months, at one year and every year thereafter.
Two independent observers performed clinical [10] and radiological [6] assessments, using the Knee Society Score (KSS). Data were collected and tabulated using Microsoft Excel 2003 (Redmond, WA). Preoperative, early post-operative, and final follow-up standing antero-posterior, lateral, and Merchant digital X-ray views were analyzed. Radiographs were taken tangential to the tibial tray bone-cement interface. This provided adequate visualization of the cement layer. The radiographs were evaluated for radiolucency at the bone–cement interfaces around the two components and around the tibial stem according to the method of the Knee Society [6]. Every change in the position of the components, femoral-tibial alignment in the coronal plane, and osteolysis was recorded. The osteolysis was defined as an expanding area of focal radiolucency of at least 1 cm, as described by Rodriguez et al. [20].
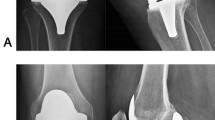
The radiographs were acquired digitally with a DICOM (Digital Imaging and Communications in Medicine) standard, and the measurements were made using a Fuji® DICOM viewer. To standardize the image acquisition and to test the accuracy of the measurements, a magnification marker was used (5 Euro cents coin, diameter 2 cm). On the first post-operative antero-posterior and lateral views, the angles between the anterior tibial crest and the tibial component were measured. These angles were used to position the X-ray beam and acquire radiographs tangential to the tibial tray during the follow-up visits. Furthermore, the thickness of the metal tray was measured on the DICOM viewer, and this value compared to the real dimension of the implant in order to confirm the radiograph was tangential to the tibial plateau. The cement mantle bone penetration was measured dividing the tibial surface into 4 zones [9] on the anterior-posterior view (from medial to lateral the regions are 1, 2, 3 and 4) and in 2 zones in lateral view (1 and 2 from anterior to posterior) to evaluate the depth of the cement penetration (Figs. 1 and 2). The cement penetration in each zone was measured with the DICOM viewer. Each radiograph was examined by two independent observers. For each exposure, the mean value of the measurements made by the two observers was considered.
Ethical board statement
In light of the Italian law, we are not required to ask for approval for this type of studies. However, each author certifies that his institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research. Nevertheless, we obtained an informed consent from the patients included in the study, explaining the advantages and drawbacks of each technique (surface versus full cementation).
Statistical analysis
The study was designed to identify a minimal difference of one point in terms of mean/SD ratio between radiolucency lines and any other covariate. Assuming an alpha level of 0.05 and a power of 0.90, sixty patients are needed to detect such effect. Computations of sample size were performed using ADDPLAN v4.0 (ADDPLAN GmbH, Cologne, Germany).
Inter-observer reliability between the two independent observers was calculated using the Spearman Brown prediction formula for all measured parameters (variability range 0.95–0.99).
Variables were described using median (Interquartile range) or mean (SD) according to their symmetry and categorical variables presented with percentages and absolute number of observed subjects. Differences between groups were performed using a Wilcoxon test for the continuous variables and a Chi-Square with Yates correction for categorical ones. Multivariable analysis was performed using a logistic regression model for the radiolucency lines as outcome. Covariates’ selection was performed with forward procedure using AIC (Akaike Information Criterion) as selection criterion. The covariates considered clinically relevant included age, sex, BMI, follow-up time, cement penetration in each zone, tibial slope, femoral flexion, frontal alignment and clinical, functional and total pre-operative and post-operative Knee Scores. All analyses were performed using the R System.
Results
Seventy knees in 62 patients underwent primary cemented TKA PS URP using surface cementation technique. No patients were lost to follow up.
The preoperative femoral-tibial angle in the coronal plane averaged 5 degrees of varus (range from 12 degrees of valgus to 15 degrees of varus) and at the final follow-up evaluation averaged 4 degrees of valgus (range from 5 degrees of varus to 8 degrees of valgus).
The average active range of movement was from 4 degrees (range 0–20 degrees) to 110 degrees (range 80–135 degrees) preoperatively and from 1 degree (range 0–13 degrees) to 123 degrees (range 85–135 degrees) at the final follow-up.
The preoperative average clinical and functional Knee Society ratings were 52 points (SD 15) and 42 points (SD 23), respectively, and at the final follow-up evaluation 91 points (SD 8) and 86 points (SD 17), respectively.
No radiographs demonstrated osteolytic lesions around the implants, as defined by Rodriguez et al. [9]. Nonprogressive radiolucent lines were noted in 5 cases (7%) around the tibial stem (Fig. 3) with no sign of component loosening or osteolysis identifiable on the radiograph at final follow-up. All patients were asymptomatic. The radiolucencies were noted at a mean of 39 months (SD 12) from surgery and a mean of 11.5 months (SD 2) from their recognition to the last follow-up. The presence of radiolucent lines was not significantly correlated with age, sex, BMI, follow-up time, cement penetration in each zone (in both antero-posterior and lateral views), tibial slope, femoral flexion, frontal alignment and both preoperative and last follow-up Knee Scores.
The mean radiographic cement penetration in anterior-posterior view was 2.3 mm (SD 0.7) in zone 1, 3.2 mm (SD 0.6) in zone 2, 2.9 mm (SD 0.7) in zone 3 and 2.6 mm (SD 0.8) in zone 4. The mean radiographic cement penetration in lateral view was 2.8 mm (SD 0.7) in zone 1 and 3.1 mm (SD 0.6) in zone 2.
Discussion
The most important finding of this study is that the rate of early loosening, using surface cementation and mobile tibial tray in TKAs, is comparable to other cementation techniques and prosthetic designs described in the literature.
Total knee arthroplasty is a reliable procedure with excellent overall results and a 15-year Kaplan–Meier survivorship from 84 to 99% [9]. Rotating platform implants reported results comparable to fixed-bearing TKAs at 15 and 20 years follow-up [4].
A stable primary fixation is considered a cornerstone in order to obtain durable results and to avoid early loosening of the implant. The cement fixation is still the “gold standard” [9]. Many factors have been described to improve the cementation technique, and these include a cement penetration of 3 mm [25], the use of pulsatile lavages [5, 11, 15], the cement application in a low viscosity state [11, 15], and the use of an intra-osseous suction [1, 17]. Nevertheless, the most reliable type of cementation (full versus hybrid) is still controversial. Although full cementation technique is widely accepted and reported excellent and durable results [8, 9], hybrid fixation is certainly a fascinating alternative option that may reduce the stress shielding effect on the proximal tibia and the metaphyseal bone loss in case of revision [18, 21].
Few studies report biomechanical and clinical results of surface cementation technique. Peters et al. in their biomechanical cadaver study found no differences in terms of micromotion and cement penetration between surface and full cementation, using both cruciate and I-beam tibial trays [18].
Bert and McShane, in a biomechanical study on artificial proximal tibia model, showed comparable stability between full and hybrid cementation, when a 3-mm cement penetration was achieved [3].
Seki et al. in a cadaver study compared both implant stability and proximal tibial cortex strain, both with full and with hybrid cementation technique. No significant differences in micromotion were found between the two methods. However, cemented stems had significantly increased strain relief in the proximal tibia compared to uncemented stems. [21].
Skwara et al. in a recent biomechanical cadaveric study found no significant differences in terms of primary stability between full and surface cementation. However, a higher number of failures were recognized in the fully cemented group [22].
Lombardi et al. compared full- versus surface-cement technique in 68 consecutive knees. Two of 23 knees with surface-cemented tibial components required revision secondary to aseptic failure at 36 and 55 months, whereas none of the 45 knees with fully cemented tibial components had to be revised. They suspected the surface-cemented knees failed because of poor cement penetration (average 2 mm), compared to fully cemented knees (average 4-mm) [13].
Hofmann et al. reported the results of surface cementation with a fixed-bearing implant at a minimum 5-year follow-up. They treated 128 consecutive knees, and no osteolytic lesions were found. However, 3 tibias had radiolucent lines with asymptomatic, nonprogressive, and not associated with implant failure patterns. The average depth of penetration of cement was 2.7 mm [9].
All the papers cited comparing full versus surface cementation techniques used fixed-bearing tibial components. The only paper comparing both cementation techniques using a tibial rotating platform is a biomechanical study [14]. The authors described the increased micromotion of the tibial component in mobile-bearing TKA using hybrid technique (with a 3-mm cement mantle), compared to full cementation. A limitation of this study is the use of sawbones.
The present study is the first to report short-term clinical and radiological results of an URP prosthesis using a surface cementation technique and a press-fit stem fixation. The overall results reported are comparable to Hofmann’s et al. outcomes with a fixed-bearing design, either in clinical/radiological evaluations or in average cement penetration [9]. We have to underline that both in Hofmann’s study and in the present study, the implants have a peripheral lip that may enhance cement penetration by reducing cement escape during implantation [24].
In the present study, no loosening cases were observed, but in five cases (7%) radiolucency lines around the noncemented stem were recognized. Although the natural history of radiolucencies seems to be benign, there are still some concerns that they may represent signs of loosening. However, these five patients were asymptomatic with full weight bearing and excellent range of motion. The average follow-up was 50.5 months (SD 10, range 37 to 60 months). They were followed for a mean of 11.5 months (DS 2) after the radiolucencies were noted, without any clinical or radiological worsening. This is certainly an encouraging point, but considering the two aseptic failures described by Lombardi et al. at 36 and 55 months of follow-up, we cannot surely state that radiolucency lines noted are not correlated with loosening [13]. A long-term follow-up is required to certainly exclude this possibility. Nevertheless, Smith et al. reported, out of 195 hybrid fixed TKAs, 15 cases (8%) of radiolucency lines around the tibial component, diagnosed within the first 2 years and without any progression to loosening [23].
As mentioned, a limitation of the present study is the relatively short follow-up (minimum 37 months, average 43 months, SD 14). A long-term follow-up study is required to definitely confirm the reliability of the technique. Nevertheless, many studies showed that the highest rate of complications after TKA, most of all aseptic failures, occurs in the early post-operative period [2, 7, 19]. For these reasons, the authors feel that an initial report may be useful to exclude a high early failure rate with hybrid fixation and mobile-bearing designs.
Conclusions
In the light of these considerations, we can conclude that full cementation technique still remains the gold standard, according to the longer follow-up outcomes reported in the literature. Nevertheless, at short follow-up, the rate of early loosening and radiolucency lines with mobile tibial tray and surface cementation is comparable to other studies using different cementation techniques or surface cementation and fixed platform total knee arthroplasties.
References
Banwart JC, McQueen DA, Friis EA et al (2000) Negative pressure intrusion cementation technique for total knee arthroplasty. J Arthroplasty 3:360–367
Barrack RL, Nakamura SJ, Hopkins SG, Rosenzweig S, Winner of the 2003 James A. Rand Young Investigator’s Award (2004) Early failure of cementless mobile-bearing total knee arthroplasty. J Arthroplasty 19:101–106
Bert JM, McShane M (1998) Is it necessary to cement the tibial stem in cemented total knee arthroplasty? Clin Orthop Relat Res 356:73–78
Callaghan JJ, O’Rourke MR, Iossi MF, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC (2005) Cemented rotating-platform total knee replacement. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am 87:1995–1998
Dorr LD, Lindberg JP, Claude-Faugere M et al (1984) Factors influencing the intrusion of methylmethacrylate into human tibia. Clin Orthop Relat Res 183:147–152
Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failure in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Gandhi R, Tsvetkov D, Davey JR, Mahomed NN (2009) Survival and clinical function of cemented and uncemented prostheses in total knee replacement: a meta-analysis. J Bone Joint Surg Br 91:889–895
Hofmann AA, Goldberg TD, Tanner AM, Cook TM (2006) Surface cementation of stemmed tibial components in primary total knee arthroplasty: minimum 5-year follow-up. J Arthroplasty 21:353–357
Hyldahl H, Regner L, Carlsson L et al (2005) All-polyethylene vs. metal-backed tibial component in total knee arthroplasty a randomized RSA study comparing early fixation of horizontally and completely cemented tibial components: part 2. Completely cemented components: MB not superior to AP components. Acta Orthop 76:778–784
Insall JN, Dorr LD, Scott RD et al (1989) Rationale of knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Krause WR, Krug W, Miller J (1982) Strength of the cement-bone interface. Clin Orthop Relat Res 163:290–299
Lombardi AV Jr, Berasi CC, Berend KR (2007) Evolution of tibial fixation in total knee arthroplasty. J Arthroplasty 22(4 Suppl 1):25–29
Lombardi AV Jr, Mallory TH, Gunderson R, et al (1998) Surface-cementation of the tibial component in total knee arthroplasty. Proceedings 65th Annual Meeting of the American Academy of Orthopaedic Surgeons, New Orleans, LA, pp 1
Luring C, Perlick L, Trepte C, Linhardt O, Perlick C, Plitz W, Grifka J (2006) Micromotion in cemented rotating platform total knee arthroplasty: cemented tibial stem versus hybrid fixation. Arch Orthop Trauma Surg 126:45–48
Maistrelli GL, Antonelli L, Fornasier V et al (1995) Cement penetration with pulsed lavage versus syringe irrigation in total knee arthroplasty. Clin Orthop Relat Res 312:261–265
Marcacci M, Soavi R, Loreti I et al (2001) Micromotion between the half bearings in the interax prosthesis: a roentgen stereophotogrammetric analysis. J Arthroplasty 16:991–997
Matthews JJ, Ball L, Blake SM, Cox PJ (2009) Combined syringe cement pressurisation and intra-osseous suction: an effective technique in total knee arthroplasty. Acta Orthop Belg 75:637–641
Peters CL, Craig MA, Mohr RA, Bachus KN (2003) Tibial component fixation with cement. Full-versus surface-cementation techniques. Clin Orthop Relat Res 409:158–168
Piedade SR, Pinaroli A, Servien E, Neyret P (2009) Revision after early aseptic failures in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 17:248–253
Rodriquez JA, Bhende H, Ranawat CS (2001) Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res 388:10–17
Seki T, Bourgeault ST, Chareancholvanich K, Lew W et al (1997) Does a central stem affect bone strain and the stability of a cemented tibial tray in primary and revision TKA? Orthop Trans 21:635–640
Skwara A, Figiel J, Knott T, Paletta JRJ, Fuchs-Winkelmann S, Tibesku CO (2009) Primary stability of tibial components in TKA:in vitro comparison of two cementing techniques. Knee Surg Sports Traumatol Arthrosc 17:1199–1205
Smith S, Naima VS, Freeman MA (1999) The natural history of tibial radiolucent lines in a proximally cemented stemmed total knee arthroplasty. J Arthroplasty 14:3–8
Vertullo CJ, Davey JR (2001) The effect of a tibial baseplate undersurface peripheral lip on cement penetration in total knee arthroplasty. J Arthroplasty 4:487–492
Walker PS, Soudry M, Ewald FC et al (1984) Control of cement penetration in total knee arthroplasty. Clin Orthop Relat Res 185:155–164
Acknowledgments
The authors acknowledge Laneune Baccam for the professional proof reading and the valuable help during the drafting of the manuscript. The authors have no personal or institutional financial support to disclose, regarding this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rossi, R., Bruzzone, M., Bonasia, D.E. et al. No early tibial tray loosening after surface cementing technique in mobile-bearing TKA. Knee Surg Sports Traumatol Arthrosc 18, 1360–1365 (2010). https://doi.org/10.1007/s00167-010-1177-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1177-2