Abstract
Despite the frequent use of computer-assisted total knee arthroplasty (TKA) and better radiological results for coronal alignment reported in many studies, there is still no evidence of improved clinical outcomes when compared to conventional TKA. We compared alignment after navigated TKA and conventional TKA in 80 randomized patients. Seventy three patients were available for physical and radiological examination at 20 month after surgery. Both groups showed similar Knee Society Score results, with medians of 89 points (navigated 49–95 points, conventional 48–95 points, n.s.) in the Knee Score and 70 points (navigated 45–100 points, conventional 40–100 points, n.s.) in the Function Score. The median improvement in the Knee Society Knee Score was 45 points (−3 to 88 points) in the navigated group and 35 points (−13 to 62 points) in the conventional group (P = 0.03), and the Knee Society Function Score improvement was 15 points (−10 to 50 points) in the navigated group versus 10 points (−10 to 50 points) in the conventional group (n.s.). The current health state at follow-up using the EuroQuol questionnaire was similar in both groups, with medians of 67 points in the navigated group and 65 points in the conventional group. This investigation did show slightly greater functional improvement at short-term follow-up in the navigated TKA group. Longer follow-up will be required to assess the possible benefit of computer-assisted navigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Computer-assisted navigation is frequently used in total knee arthroplasty (TKA). Several studies have investigated the precision of implant positioning, and many showed a better restoration of the mechanical leg axis, at least fewer outliers outside critical ranges compared to conventional TKA [1]. It has also been shown that soft tissue balancing is more accurate with the use of a navigation system [7, 14]. Therefore, better clinical results and possibly decreased revision rates have been expected in navigated TKA.
The use of computer-assisted navigation causes costs, including the cost of the navigation system and a prolonged operative time [3, 19]. These costs are justified if there is a benefit for the patient. It has been suggested that the use of a navigation system might be cost-effective if there are decreased revision rates [25]. However, there is till now no evidence of improved clinical results after navigated TKA [4]. There are many studies about navigated TKA, but only a few of them have assessed functional results after more than a 6-month follow-up [11, 12, 17, 26]. These studies did not find statistically significant differences between computer-assisted and conventional TKA.
In a previously published study comparing the component alignment between computer-assisted and conventional TKA using radiographic and CT evaluation [16], 80 patients were randomly assigned to either navigated or conventional cemented, unconstrained, cruciate-retaining TKA with a rotating platform (ScorpioTM PCS, Stryker Orthopaedics, Mahwah, NJ) without patellar resurfacing. There were fewer outliers outside a range of 3° varus or valgus in the navigated group, but this difference was not statistically significant. There were no differences in coronal, sagittal or rotational alignment of the femoral and tibial components between the two groups. These patients have been followed up in order to evaluate the postoperative functional results between navigated and conventional TKA.
The aim of this study was to determine whether there is any difference between the functional results of navigated and conventional TKA. The hypothesis was that the navigated TKA would show better clinical results.
Materials and methods
Inclusion criteria for the primary study (5) included primary or secondary osteoarthritis of the knee, no previous hemiarthroplasty or total arthroplasty, a mechanical axis between 20° varus and 5° valgus and no severe instability that could not be treated with an unconstrained, cruciate-retaining TKA. All patients were operated by two surgeons trained in navigated TKA (SK, JL).
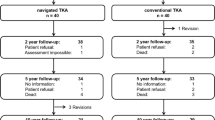
A total of 104 patients met the inclusion criteria and were screened for enrollment in the study. Fifteen patients did not provide informed consent, two patients could not be randomized due to a clinical need for navigation and seven patients were excluded due to the intraoperative decision to use a posterior stabilized implant. After giving their informed consent, 80 patients were randomized to navigated or conventional TKA study arm. The 1:1 randomization scheme was based on a permutation algorithm without stratification.
All patients included in the primary study [16] were invited for follow-up after 18–32 months postoperatively. The study protocol for follow-up was approved by the local independent ethics committee in January 2008. Patients were interviewed by a local study nurse preoperatively and postoperatively at a median of 20 months after TKA. In addition to the written interview, the Knee Society Score [9] and the EuroQol questionnaire (release EQ-5D) were performed [21].
The Knee Society Score is divided into the knee score and the function score. In both scores, a total of 100 points indicates full function. The knee score is based on pain, range of motion, stability and alignment of the leg. The function score is based on activities of daily living. The EuroQol describes the health state of the patient using subgroups of mobility, self-care, usual activities, pain/discomfort, anxiety/depression and a visual analog scale. The subgroups are divided into three levels (no problems, some problems and serious problems/unable to do). The visual analog scale records the patient’s current health state. A value of 100 indicates the best imaginable and a value of 0 indicates the worst imaginable health state. Physical examination was done by either of the two operating surgeons (JL, SK).
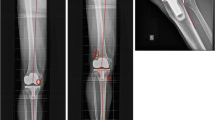
Radiographic assessment included a full-length standing and a lateral radiograph. The digital images were evaluated using the software ID.PACS Release 3.6 (Image Devices, Idstein, Germany). The mechanical axis was defined as the angle between a line from the center of the hip to the center of the tibial tray (fixation peg for rotating platform) and a line from the center of the tibial tray to the midpoint of the ankle joint. Radiolucent lines were assessed according to the criteria of the Knee Society Total Knee Arthroplasty roentgenographic evaluation and scoring system [6].
Statistical analysis
Endpoints of this investigation were differences between the two groups in the functional outcome (Knee Society Score) or in general health state (EuroQol questionnaire). Data description was based on medians and inter-quartile ranges for continuous values and on absolute and relative frequencies for categorical endpoints, respectively. Comparisons between groups were based on two sample Wilcoxon tests for continuous endpoints and on Fisher’s exact tests for categorical endpoints, respectively. Results of these exploratory significance tests were summarized in P-values, where P < 0.05 indicates statistically significant differences between groups. All analyses were performed according to the intention-to-treat principle using SPSS® software (release 16.0 for Windows®).
Sample size was determined based on the ability to detect a minimum difference of 5° in component alignment with a minimum power of 80% and the assumption of a 10% drop-out rate, as previously reported in detail [16].
Results
Of the 80 patients assessed in the primary study, two patients from the conventional group died before initiation of the follow-up study. Of the remaining 78 patients, five did not return for a follow-up visit (two from the navigated group and three from the conventional group), one patient had undergone revision for a preoperatively unknown metallic hypersensitivity with persistent swelling. In this case, the TKA was replaced by an allergy-coated implant. One patient had a Girdlestone resection following total hip infection on the same leg. In this case, the implanted TKA is still in situ, but its function could not reliably be evaluated due to the Girdlestone resection. Three patients refused to attend the follow-up examination, two of whom did not report any problems and one who still had some pain but declined further examination. Seventy three patients were available for physical and radiological follow-up after a median of 20 months postoperatively, 38 in the navigated TKA group and 35 in the conventional TKA group.
No unexpected device-related events were reported. In total, there were seven deep venous thromboses, one pulmonary embolism, four hematomas (none of which led to revision) and two temporary femoral nerve palsies with complete regression. No cases of deep infections or delayed wound healing were reported. In one patient, a mobilization under anesthesia was necessary 3 months postoperatively, and in one patient, a revision was performed (as already mentioned).
The Knee Society Knee Score (Table 1) showed lower values preoperatively in the navigated group but similar results to the conventional group at follow-up (P = 0.03). The Knee Society Function Score also showed lower values preoperatively in the navigated group and similar results to the conventional group at follow-up (n.s.).
The EuroQol questionnaire demonstrated an improvement of the current health state from in median 50 points preoperatively in both groups (range: 20–90 in the navigated group, 10–80 in the conventional group) to 70 points (range: 35–100) at follow-up in the navigated group and 65 points (range: 30–100) in the conventional group on a visual analog scale between 0 and 100. However, there was notable improvement in the subgroups of mobility, usual activities and pain/discomfort and less improvement in the subgroups of self-care and anxiety/depression. There were no statistical significant differences between the study groups.
Co-factors such as BMI, Age at operation and gender had no influence on functional outcome (Knee Society Score). A preoperative deformity of more than 10° varus resulted in a greater improvement in the Knee Society Knee Score, which is due to the direct input of the axis in this score. Postoperative leg alignment measured on a full-length standing radiograph had no influence on functional outcome.
Because we used a rotating platform and the femur and the tibia could align according to the soft tissue strains, we were able to measure the rotational deviation between the femoral and tibial component on the postoperative CT scans. Nine patients with a postoperative rotational mismatch of more than 10° between the femoral and tibial components showed no improvement and had significantly worse results in the Knee Society Function Score (Table 2). The postoperative femoral or tibial rotational alignment of the components alone had no influence on the functional outcome. None of these co-factors had an influence on the general health state (EuroQol questionnaire).
There were no radiolucent lines of more than 1 mm or changes in implant position at this short-term follow-up after in median 20 month.
Discussion
The most important finding of the present study was that there was no difference in short-term functional outcome and quality of live after navigated and conventional TKA.
Computer-assisted navigation leads in many studies to more accurate TKA implantation in the coronal plane, or at least to fewer outliers outside a critical range of 3° varus or valgus malalignment [1]. Because studies have demonstrated higher revision rates and less favorable clinical results for malaligned TKA [2, 10, 15, 24], it is assumed that computer-assisted navigation may lead to better clinical results.
There are many studies about postoperative alignment in conventional and navigated TKA, but, despite the frequent use of computer-assisted navigation, few studies have reported clinical results of more than 6-month follow-up [11, 12, 17, 26]. None of these studies demonstrated better functional outcome for navigated TKA compared to the conventional technique after short-term to medium-term follow-up.
Spencer et al. [26] reported about 60 patients (30 navigated and 30 conventional TKA) from a randomized controlled trial of 71 patients. At 2 years, there were no statistically significant differences between both groups using the Knee Society Score (156.4 vs. 158.9 points), the WOMAC (23.4 vs. 13.6 points), the Oxford Knee Score (26.7 vs. 20.1) and in none of subgroups of the SF-36 Health Survey. This is interesting because the initial study demonstrated significantly better coronal, sagittal and rotational alignment for the navigated TKA.
Molfetta et al. [17] reported about 60 patients from a retrospective case–control study after 5.4 years of follow-up. They did not show a difference in clinical outcomes using the Knee Society Knee Score (84 vs. 90 points) and Function Score (85 vs. 87 points), despite a significantly better restoration of the mechanical leg axis in navigated TKA.
Kim et al. [12] reported on 160 patients from an initial group of 170 who received bilateral sequential TKA, each patient with one navigated and one conventional implanted TKA. The Knee Society Knee Score (92 vs. 93 points) and Function Score (83 vs. 81 points) and Hospital for Special Surgery Score (89 vs. 91 points) did not show a difference between the two groups. However, it would seemingly be difficult to discriminate between two knees in the same patient for several parts of the scoring (e.g. walking ability, climbing stairs).
Kamat et al. [11] analyzed retrospectively 565 TKA, 263 that were done using computer navigation and 302 done using the conventional technique. Data were taken from the arthroplasty outcome program, which included a postal questionnaire every year using the Oxford Knee Score. Only 13 navigated and 15 conventional TKAs were followed up for 5 years. There was no statistical difference between the two groups in the Oxford Knee Score at any time. They had 3-year postoperative clinical and radiological follow-up for 67 navigated and 84 conventional TKA. There were fewer outliers from a neutral mechanical axis beyond ±3° in the navigated group (2.9 vs. 15.5%), but there was no difference in the Knee Society Score (164.9 vs. 162 points).
These results are consistent with our findings at 20 months after surgery. There were no differences between the two groups in the Knee Society Score and the general health state evaluated with the EuroQol questionnaire, although the navigated group showed greater improvement in both scores because the navigated knees had slightly poorer preoperative scores for both parts of the Knee Society Score. However, only the improvement in the Knee Society Knee Score was statistically significant.
TKA is one of the most successful procedures in terms of functional improvement, quality of life and cost effectiveness [18, 22]. It is therefore difficult for any new technique to further improve these results. Even if there is no statistically significant difference between navigated and conventional TKA in the short-term follow-up, it may take a longer time to show a possible difference. Longer follow-up is therefore needed to evaluate the possible advantages of this technique, which may result in lower revision rates. Furthermore, the Knee Society Score is widely accepted for measuring the results after TKA, but it may not be sensitive enough to detect small functional differences. Therefore, more sensitive evaluation tools may be necessary. Further limitations of the study include the lower Knee Society Score values preoperatively in the navigated group despite randomization and the loss of seven patients to follow-up.
On the other hand, the currently most accepted outcome parameter for the accuracy of TKA implantation is leg alignment, which is measured in most studies using a full-leg standing radiograph. It has been demonstrated that the reliability of this type of radiograph can vary due to inaccuracies caused by possible flexion and rotation of the leg [13, 20]. Also, the leg alignment measured on radiographs does not always correlate with the data given by the navigation system [27]. It has been suggested that the leg alignment data provided by the navigation system may be more precise than measurements obtained from full-leg standing radiographs [27]. Therefore, comparing the functional results of patients to the measurement of the full-leg standing radiographs may be a disadvantage of current studies.
There are more factors than leg alignment affecting clinical outcome after TKA including rotational alignment, soft tissue balancing, the patello–femoral joint and patient-related factors. With the exception of rotational alignment, none of these factors have been sufficiently investigated. It is not known whether computer-assisted navigation may influence soft tissue balancing and patellar tracking because these are difficult to measure. However, in our study, there was no improvement in the Knee Society Function Score if there was a rotational mismatch between the femoral and tibial component of more than 10° in the postoperative CT scan. This mismatch was mainly caused by malrotation of the tibial component in relation to the medial third of the tibial tuberosity. It has been assumed that a rotating platform design is forgiving to malrotation of the tibia. This seems to be not applicable to our patients. It could be demonstrated that knees with a rotational deviation between the femoral and tibial components showed different kinematics during flexion than rotationally well-aligned knees [8]. Other investigations demonstrated different kinematics in TKA with external femoral component rotation compared to neutral or internal femoral rotation [5, 23]. This may influence functional outcome and could explain our findings.
Conclusion
Total knee arthroplasty is a very successful procedure making it difficult to improve its results. Computer-assisted navigation did not result in a statistically significant better functional outcome after short-term follow-up. However, it may take a longer period of follow-up to evaluate whether better alignment after navigated compared to conventional TKA may reduce wear and consequently result in lower revision rates.
References
Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D (2007) Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am 89A:261–269
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34
Cerha O, Kirschner S, Gunther KP, Lützner J (2009) Cost analysis for navigation in knee endoprosthetics. Orthopäde 38:1235–1240
Dattani R, Patnaik S, Kantak A, Tselentakis G (2009) Navigation knee replacement. Int Orthop 33:7–10
DesJardins JD, Banks SA, Benson LC, Pace T, LaBerge M (2007) A direct comparison of patient and force-controlled simulator total knee replacement kinematics. J Biomech 40:3458–3466
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Hakki S, Coleman S, Saleh K, Bilotta VJ, Hakki A (2009) Navigational predictors in determining the necessity for collateral ligament release in total knee replacement. J Bone Joint Surg Br 91B:1178–1182
Harman MK, Banks SA, Kirschner S, Lützner J (2009) Axial alignment of mobile-bearing TKR: does it affect knee rotation and bearing motion? 10th EFORT Congress, http://www.efort.org/cdrom2009/FreePaperContent.asp?Pid=F208
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73B:709–714
Kamat YD, Aurakzai KM, Adhikari AR, Matthews D, Kalairajah Y, Field RE (2009) Does computer navigation in total knee arthroplasty improve patient outcome at midterm follow-up? Int Orthop 33:1567–1570
Kim YH, Kim JS, Choi Y, Kwon OR (2009) Computer-assisted surgical navigation does not improve the alignment and orientation of the components in total knee arthroplasty. J Bone Joint Surg Am 91A:14–19
Krackow KA, Pepe CL, Galloway EJ (1990) A mathematical analysis of the effect of flexion and rotation on apparent varus/valgus alignment at the knee. Orthopedics 13:861–868
Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB Accuracy of soft tissue balancing in TKA: comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc (Epub ahead of print). doi:10.1007/s00167-009-0983-x
Lotke PA, Ecker ML (1977) Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am 59:77–79
Lützner J, Krummenauer F, Wolf C, Günther K-P, Kirschner S (2008) Computer-assisted and conventional total knee arthroplasty—a prospective, randomized study with radiographic and CT evaluations. J Bone Joint Surg Br 90B:1039–1044
Molfetta L, Caldo D (2008) Computer navigation versus conventional implantation for varus knee total arthroplasty: a case-control study at 5 years follow-up. Knee 15:75–79
IH N (2004) NIH Consensus Statement on total knee replacement. J Bone and Joint Surg Am 86A:1328–1335
Novak EJ, Silverstein MD, Bozic KJ (2007) The cost-effectiveness of computer-assisted navigation in total knee arthroplasty. J Bone Joint Surg Am 89A:2389–2397
Oberst M, Bertsch C, Wurstlin S, Holz U (2003) CT analysis of leg alignment after conventional vs. navigated knee prosthesis implantation. Initial results of a controlled, prospective and randomized study. Unfallchirurg 106:941–948
Oppe M, Rabin R, de Charro F (2008) EQ-5D User Guide. www euroqol org
Rasanen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynanen OP, Roine RP (2007) Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop 78:108–115
Rhoads DD, Noble PC, Reuben JD, Tullos HS (1993) The effect of femoral component position on the kinematics of total knee arthroplasty. Clin Orthop Relat Res 286:122–129
Ritter MA, Faris PM, Keating EM, Meding JB (1994) Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res 299:153–156
Slover JD, Tosteson AN, Bozic KJ, Rubash HE, Malchau H (2008) Impact of hospital volume on the economic value of computer navigation for total knee replacement. J Bone Joint Surg Am 90A:1492–1500
Spencer JM, Chauhan SK, Sloan K, Taylor A, Beaver RJ (2007) Computer navigation versus conventional total knee replacement: no difference in functional results at two years. J Bone Joint Surg Br 89:477–480
Yaffe MA, Koo SS, Stulberg SD (2008) Radiographic and navigation measurements of TKA limb alignment do not correlate. Clin Orthop Relat Res 466:2736–2744
Acknowledgments
The authors are grateful to Heike Voigt for her valuable assistance in clinical data management and evaluation.
Conflict of interest statement
The authors have received funding from Stryker Orthopaedics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lützner, J., Günther, KP. & Kirschner, S. Functional outcome after computer-assisted versus conventional total knee arthroplasty: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc 18, 1339–1344 (2010). https://doi.org/10.1007/s00167-010-1153-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1153-x