Abstract
Purpose of this study is to conduct a meta-analysis comparing the results of open and arthroscopic Bankart repair using suture anchors in recurrent traumatic anterior shoulder instability. Using Medline Pubmed, Cochrane and Embase databases we performed a search of all published articles. We included only studies that compared open and arthroscopic repair using suture anchors. Statistical analysis was performed using chi-square test. Six studies met the inclusion criteria. The total number of patients was 501, 234 suture anchors and 267 open. The rate of recurrent instability in the arthroscopic group was 6% versus 6.7% in the open group; rate of reoperation was 4.7% in the arthroscopic group vs. 6.6% in open (difference not statistically significant). The difference was statistically significant only in the studies after 2002 (2.9% of recurrence in the arthroscopic group vs. 9.2% in open; 2.2% of reoperation in the arthroscopic group vs. 9.2% in open). Results regarding function couldn’t be combined because of non-homogeneous scores reported in the original articles, but the arthroscopic treatment led to better functional results. Arthroscopic repair using suture anchors results in similar redislocation and reoperation rate compared to open Bankart repair; however, we need larger and more homogeneous prospective studies to confirm these findings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
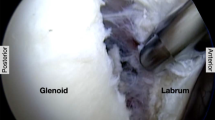
Since 1938, when Bankart described the detachment of the anterior inferior labrum from the glenoid rim as a cause of anterior instability and presented his case report of 27 patients treated surgically, open surgical repair has been considered the gold standard [1]. Over the past two decades, arthroscopic techniques have evolved and are currently widely used in Bankart repair for recurrent shoulder instability. Arthroscopic techniques have been developed in an attempt to reduce common criticisms associated with open repair including wide dissection, loss of external rotation and post-operative pain [2, 6, 12].
Presently, both open and arthroscopic repair of antero-inferior labral tears for shoulder instability are extensively utilized. A review of literature shows that the debate remains open between the two treatment modalities with studies presenting differing results and conclusions. However, it is currently accepted that, within the arthroscopic group, repair using suture anchors is more effective than other arthroscopic techniques including transglenoid sutures and suture tacks. Limits of current studies are related to the heterogeneity of the study groups and the great variability within arthroscopic techniques compared with open procedures, with the consequence of attempting to compare various open procedures and various arthroscopic techniques. Other limits are represented by the small size of the study groups and short-term follow-up for arthroscopic repair using suture anchors. Presently, only few papers comparing open and arthroscopic repair using suture anchors have been published.
The purpose of this study is to conduct a meta-analysis comparing the results of open Bankart repair versus arthroscopic Bankart repair using suture anchors in recurrent traumatic anterior shoulder instability.
Materials and methods
Using Medline Pubmed, Cochrane and Embase we performed a search of all published articles using as keywords “anterior shoulder instability, Bankart repair, suture anchors, arthroscopic Bankart repair, open Bankart repair”. The search was limited to English language articles, and the research was conducted by one author and reviewed by a second author. The abstracts were then reviewed in order to select only articles including a direct comparison between open and arthroscopic technique for Bankart repair. Full articles of the selected abstracts were obtained and evaluated by the authors.
Inclusion criteria were established before data collection. We included only studies that directly compared open and arthroscopic Bankart repair using suture anchors for the treatment of shoulder instability. We considered only post-traumatic anterior instability.
Articles that included multi-directional and posterior instability were excluded. Articles that presented results of treatments using arthroscopic techniques other than suture anchors (i.e., transglenoid sutures, staples, tacks) were also excluded. Studies that reported combined arthroscopic treatments (i.e., suture anchors and transglenoid sutures) and non-anatomic open reconstruction (i.e., Bristow-Latarjet, Eden-Hybinette, Putti-Platt) were excluded as well.
One author extracted the data. All study results were tabulated including year of study, level of evidence, number of patients and surgical technique. Demographic data including the number of patients, mean age, mean follow-up and dominant extremity (where available) were included. We also collected the rate of recurrences, reoperation, and information about pre-operative and post-operative ROM. Finally, functional outcome according to the scores reported in original articles (UCLA shoulder scale, Rowe score for instability, Constant score, ASES score) were tabulated. We accepted level I, II, III studies.
Statistical analysis
Statistical analysis was performed using the chi-square test, useful for the analysis of 2 × 2 tables, with 95% confidence interval (CI). The significance level was set at P < 0.05. The variables evaluated and compared were the rate of recurrences, reoperation, range of motion and functional outcome. Results were first tabulated within each group and then combined.
Results
Starting from the analysis of 2,337 abstracts obtained using our keywords, we identified 62 full articles that presented the results of the comparison between arthroscopic and open procedures using suture anchors. Seven studies directly compared open and arthroscopic repair, evaluating 528 patients, 249 shoulders treated arthroscopically with suture anchors and 279 treated with open Bankart repair. At the final review, the study by Guanche et al. [13] was excluded because they utilized combination of different arthroscopic techniques. Therefore, the articles included in the meta-analysis were six (Table 1), and the total number of patients was 501, 234 treated arthroscopically and 267 using an open procedure (Tables 2, 3). The mean age was 28.1 in the arthroscopic group, 26.4 in the open group; average follow-up was 30.2 months in the arthroscopic group, 29.9 months in the open group.
The recurrence rate in the arthroscopic group was 6% compared to 6.7% in the open group; rate of reoperation was 4.7% in the arthroscopic group versus 6.6% in open (Table 4). This difference was not statistically significant (P < 0.05). When including studies later than 2002, we found statistically significant differences between the two groups with 2.9% of recurrences in the arthroscopic group versus 9.2% in the open surgery group (Table 5). We report a 2.2% rate of reoperation in the arthroscopic group vs. 9.2% in the open surgery group.
As regard to functional outcome, the scores used in original articles were not homogeneous (i.e., UCLA scale, Rowe score, Constant score, ASES score), thus statistical analysis in order to evaluate a significance difference was not possible (Table 6).
Discussion
The present study has shown that the arthroscopic repair using suture anchors leads to redislocation and reoperation rates comparable to open Bankart repair. In addition, recent arthroscopic techniques appear to have a lower recurrence and reoperation than open suture anchor techniques.
Open Bankart repair, as described by Rowe [21], is still considered by many the gold standard for the surgical treatment of traumatic anterior shoulder instability. The classic open procedure includes the dissection of the subscapularis tendon and capsule to expose the anterior inferior margin of the labrum for a secure reattachment to the glenoid rim using various techniques, including suture anchors.
Arthroscopic techniques have been developed in an attempt to obtain similar results to open technique without the criticisms associated with open Bankart repairs. This includes reduced pain, shorter hospital stay, earlier rehabilitation and return to sport. Initial results of arthroscopic instability surgery were disappointing, with a rate of recurrent instability for transglenoid sutures ranging between 0 and 49% [2, 5, 11, 19]; bio-absorbable tacks seemed to lead to better results with rate of recurrent instability ranging between 9 and 21% [8, 11, 20, 22]. However, the redislocation rates were still higher than rates seen in open Bankart repair using suture anchors published by Dickinson [7] and Rowe [21], with recurrence rates of 3.5–4%. Common reasons for failure with arthroscopic treatment are related to a significant learning curve, wrong indications, failure to address capsular laxity and lack of recognition of significant bony lesions (“inverted pear glenoid” or engaging Hill-Sachs) [4, 15].
The introduction of suture anchors in arthroscopic surgery led to improved results that were comparable to open surgery [3, 9, 16]. Although recurrent anterior shoulder instability is one of the most common shoulder problems treated by orthopedic surgeons, there have been few rigorous trials and meta-analyses comparing these new arthroscopic methods to traditional open techniques. To date, only three meta-analyses have been conducted and none compared the same surgical method of fixation. The first, published by Hobby et al. [14], demonstrated similar rates of failure between open and arthroscopic group; it also showed that arthroscopic suture anchor repair presents lower rates of failure compared to other arthroscopic techniques. Mothadi et al. [18] demonstrated better outcomes with the open technique with respect to recurrence and return to activity. Lenters et al. [17] demonstrated that arthroscopic treatment wasn’t as effective as open repair in terms of redislocation rate but led to a better functional result according to Rowe score. On the other hand, Kim et al. [16] in a case–control study demonstrated a similar rate of recurrent instability between open and suture anchors (two recurrences in each group), but better functional results in the arthroscopic group. The authors included only traumatic recurrent anterior dislocation, excluding patients with full thickness rotator cuff tears, greater tuberosity fractures, capsular tear at the humeral insertion and previous shoulder surgery. They also noticed that patients with fewer anchors develop a greater incidence of residual instability, therefore recommending the use of a minimum of three anchors.
Similarly, Fabbriciani [9] and Bottoni [3], in prospective randomized studies (level 1 evidence), showed that the arthroscopic procedure was as effective as open surgery. Both authors included only recurrent post-traumatic anterior instability. Fabbriciani excluded patients with rotator cuff tears, SLAP lesions, ALPSA lesions, rotator interval tear or lesion of the middle glenohumeral ligament, glenoid bone defects, multidirectional instability; he reported no failures and similar outcomes between the two procedures according to Constant and Rowe scores. Bottoni excluded patients with any prior surgery on the shoulder or multidirectional instability; he reported two failures in the open group (6.9%) versus one failure in the arthroscopic (3.1%). The author also reported that the surgical time for open procedure was longer compared to arthroscopic surgery.
Two of three retrospective studies presented weakness related to heterogeneous study groups [10, 24]. The study by Field et al. [10] compared two groups of patients similar with regard to population (50 open vs. 50 arthroscopic), age and number of dislocations but different with regard to the surgeon who performed the procedure (open and the arthroscopic procedure were performed by two different authors). The authors reported 8% recurrences in arthroscopic group versus 0% in open group. Similarly, Weber et al. [24] presented 16.3% recurrence in arthroscopic group versus 3.7% in open group, but we find that the study presents limits related to the difference in the population (106 open vs. 43 arthroscopic) and to the date of the study (1991). Dissimilarly, a recent retrospective study by Wang et al. [23] reported no statistically significant difference in the functional outcome and more recurrences in open group (23.5%) versus arthroscopic (5.5%). For the most part, recurrences were usually secondary to sport injuries or traumatic events that force the arm in external rotation [3, 16, 23].
The strength of our meta-analysis is in strict criteria that led to the inclusion of studies that directly compare open and arthroscopic Bankart repair using suture anchors and excluded multidirectional instability and repair with arthroscopic techniques other than suture anchors. Only six studies met the inclusion criteria, for a total number of 501 subjects. Evaluating and combining the results of 224 arthroscopic procedures and 267 open procedures, we obtained that arthroscopic repair using suture anchors results in lower redislocation and reoperation rate compared to open Bankart repair, but the result wasn’t statistically significant. However, excluding studies antecedent to 2002, we found that the result was statistically significant. The limits described above for the study by Field et al. (1999) and the study by Weber et al. (1991) could explain this result.
Moreover, an accurate review of literature shows that articles published after 2002 report better results using suture anchors than previous studies. This could be related to the learning curve, particularly important in shoulder arthroscopy, to the improvements in instrumentation, but mainly to a better understanding of the disorder and better indications. In fact, in the last 10 years, shoulder arthroscopy has left the role of experimental technique, adopted in few selected centers, to become a widely adopted technique.
Our study could present the potential limitations of a meta-analysis, related to the strength and heterogeneity of clinical trials included. This may happen especially when non-homogeneous populations are considered, and variability in the outcome assessment is present. Level of activity, participation in contact sports, severity of instability (instability vs. dislocation) are also factors that influence the success of surgical stabilization, but these variables were not adequately reported in each study. We should also consider that surgeons apply each technique somewhat differently and sometimes aren’t equally competent with the open and the arthroscopic technique. In data extraction and analysis, many studies reported different outcome measures with some not providing information on outcome scores (Field et al., Weber et al.).
It wasn’t possible to combine the results of the open versus arthroscopic procedures regarding range of motion and function because of the variety of parameters and scores reported in the original articles (Rowe, UCLA, ASES, Constant) but overall, we found that the arthroscopic treatment led to better functional results.
Regarding the loss in external rotation, Kim et al. reported no significant difference at 90° of abduction, but the difference was found to be significant in the study published by Bottoni, who reported a minor loss in external rotation in the arthroscopic group (−2° with arthroscopy, −6.6° with open).
In the study groups, there was a prevalence of male gender, but there were no studies that separately analyzed the results. However, gender doesn’t seem to be a factor influencing the result.
No comments can be done about the correlation between dominant extremity and functional result.
Conclusion
From our meta-analysis, the arthroscopic repair using suture anchors results in similar redislocation and reoperation rate compared to open Bankart repair with recent studies (post 2002) showing improved redislocation and reoperation rates. However, multicenter clinical trials with long-term follow-up should be conduct to correctly compare the results of an established procedure with a newer promising technique.
References
Bankart ASB (1938) The pathology and treatment of recurrent dislocation of the shoulder joint. Br J Surg 26:23–29
Benedetto KP, Glotzer W (1992) Arthroscopic Bankart procedure by suture technique: indications, technique, and results. Arthroscopy 8:111–115
Bottoni CR, Smith EL, Berkowitz MJ, Towle RB, Moore JH (2006) Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med 34:1730–1737
Burkhart SS, De Beer JF (2000) Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 16:677–694
Caspari RB, Savoie FH (1991) Arthroscopic reconstruction of the shoulder: the bankart repair. In: McGinty JB et al (eds) Operative arthroscopy. Raven Press, New York, pp 507–515
Cole BJ, L’Insalata J, Irrgang J, Warner JJ (2000) Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am 82:1108–1114
Dickinson JW, Devas MB (1957) Bankart’s operation for recurrent dislocation of the shoulder. J Bone Joint Surg Br 39:114–119
Dora C, Gerber C (2000) Shoulder function after arthroscopic anterior stabilization of the glenohumeral joint using an absorbable tack. J Shoulder Elbow Surg 9:294–298
Fabbriciani C, Milano G, Demontis A, Fadda S, Ziranu F, Mulas PD (2004) Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy 20:456–462
Field L, Savoie F, Griffith P (1999) A comparison of open and arthroscopic Bankart repair [abstract]. J Shoulder Elbow Surg 8:195
Freedman KB, Smith AP, Romeo AA, Cole BJ, Bach BR Jr (2004) Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for recurrent anterior instability of the shoulder: a meta-analysis. Am J Sports Med 32:1520–1527
Green MR, Christensen KP (1993) Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy 9:371–374
Guanche CA, Quick DC, Sodergren KM, Buss DD (1996) Arthroscopic versus open reconstruction of the shoulder with isolated Bankart lesions. Am J Sports Med 24:144–148
Hobby J, Griffin D, Dunbar M, Boileau P (2007) Is arthroscopic surgery for stabilization of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J Bone Joint Surg Br 89:1188–1196
Kang RW, Frank RM, Nho SJ, Ghodadra NS, Verma NN, Romeo AA, Provencher MT (2009) Complications associated with anterior shoulder instability repair. Arthroscopy 25:909–920
Kim SH, Ha KI (2002) Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy 18:755–763
Lenters TR, Franta AK, Wolf FM, Leopold SS, Matsen FA 3rd (2007) Arthroscopic compared with open repairs for recurrent anterior shoulder instability. A systematic review and meta-analysis of the literature. J Bone Joint Surg Am 89:244–254
Mohtadi NG, Bitar IJ, Sasyniuk TM, Hollinshead RM, Harper WP (2005) Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy 21:652–658
Morgan CD, Bodenstab AB (1987) Arthroscopic Bankart suture repair: techniques and early results. Arthroscopy 3:111–122
Resch H, Povacz P, Wambacher M, Sperner G, Golser K (1997) Arthroscopic extra-articular Bankart repair for the treatment of recurrent anterior shoulder dislocation. Arthroscopy 13:188–200
Rowe CR, Patel D, Southmayd WW (1978) The Bankart procedure: a long term end-result study. J Bone Joint Surg Am 60:1–16
Speer KP, Warren RF, Pagnani M, Warner JJ (1996) An arthroscopic technique for anterior stabilization of the shoulder with a bioabsorbable tack. J Bone Joint Surg Am 78:1801–1807
Wang C, Ghalambor N, Zarins B, Warner JJ (2005) Arthroscopic versus open Bankart repair: analysis of patient subjective outcome and cost. Arthroscopy 21:1219–1222
Weber SC (1991) A prospective evaluation comparing arthroscopic and open treatment in the management of recurrent anterior glenohumeral dislocation. Orthop Trans 15:763
Conflict of interest statement
The authors declare that they have no conflict of interest related to the publication of this manuscript and that no financial grants have been received for the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petrera, M., Patella, V., Patella, S. et al. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc 18, 1742–1747 (2010). https://doi.org/10.1007/s00167-010-1093-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-010-1093-5