Abstract
Developing bio-absorbable interference screws for anterior cruciate ligament (ACL) reconstruction has proven to be a challenging task. The aim of this study was to investigate the osteogenetic response of poly-lactide carbonate (PLC) interference screws in ACL reconstruction in humans. Ten patients (median age, 28 years) underwent arthroscopic ACL reconstruction with semitendinosus/gracilis tendon graft and a PLC interference screw. The patients were scanned with a multi-slice CT scanner 2 weeks and 1 year postoperatively. Fourteen days postoperatively a mean tunnel widening of 78% [52%; 110%] was observed. At 1-year follow-up, the mean tunnel widening was 128% [84%; 180%]. No sign of bone replacement or bone ingrowth was observed. Factors such as accelerated rehabilitation, micro-motions, and early screw degradation might be responsible for this large tunnel widening. Our results demonstrate the difficulty in translation of preclinical data. This study illustrates the need for extensive preclinical investigation of new materials for clinical purposes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of metallic interference screws has been challenged by bioresorbable screws for anterior cruciate ligament (ACL) reconstruction graft fixation. Tunnel enlargement, imaging artifacts, grafts laceration, and ruptures have been reported as drawbacks of metallic interference screws [5, 29, 37, 38]. Especially tunnel enlargement or osteolysis, which is considered a multi-factorial event, does not only cause postoperative disabilities for the patient, but also complicate revision surgery considerably [29, 37].
Poly-l-Lactide acid (PLLA) is widely accepted as a biodegradable material for interference screws. It has shown to work well clinically and to perform comparably to metal interference [15, 24, 34]. However, among several different polymers available, PLLA has shown to have a clinically slow degradation [4, 20, 21, 34–36]. Also allergic reaction, delayed intra-articular inflammatory reaction, severe cartilage damage after screw breaking (and recurrent locking of the knee joint) have been reported using these PLLA screws [16, 18, 23].
Bio-absorbable co-polymer screws consisting of poly-d(2%),l(98%) lactide, and poly-d(85%),l(15%)-lactide-co-glycolide interference screws have been shown to benefit from faster degradation time with evident replacement of the screw with new bone in the canal. This has been shown by Barber et al. in a prospective study on 63 patients with radiographic follow-up at 2–3 years postoperative using the poly-d(2%),l(98%) lactide composition, and by Lajtai et al. on 28 patients with MRI 5.2 years after surgery for the (D85:L15) polymer [3, 17].
Bio-absorbable poly-lactide carbonate (PLC) interference screw (Calaxo Screw, Smith & Nephew Endoscopy, Andover, MA) consists of 65% of the co-polymer poly-d(85%),l(15%)-lactide-co-glycolide (PLGA) and 35% calcium carbonate. As introduced above, there is clinical evidence of using the 85:15 solution polymer in poly-(d,l)-lactide-co-glycolide. The inorganic component of calcium carbonate has shown to enhance strength retention of bioresorbable materials, buffer the local degradation products to help prevention of acidic environment, and provide calcium for new bone formation. Walsh et al. [33] presented promising results using PLC in an ovine model where PLC screws was replaced by bone within 1 year after soft tissue ACL reconstruction.
Calcium carbonate (CaCO3) has shown to be advantageous as implant material in terms of quick and effective degradation and new bone formation [31, 32]. Studies have shown that extracellular calcium can promote differentiation and proliferation of osteoblastic cells through calcium sensing receptors (CaR). Localized elevated extracellular calcium has been shown to stimulate osteogenic growth factors and parathyroid hormone-related peptide (PTHrP) secretion [2, 13, 14, 26].
Despite the promising preclinical data, the screw was withdrawn from the market by the company due to a report of a sterile tibial cyst and intra-articular granuloma formation after ACL reconstruction using the PLC interference screws [7].
This study was initialized and inclusion of patients was completed before the PLC screw was withdrawn from the market. We wanted to test whether the preclinical findings of screw replacement by bone could be found in the human situation. A computer tomography method was used to detect tunnel crosssection area and new bone formation. The aim of this study was to investigate the osteogenetic response of PLC interference screws in ACL reconstruction.
We hypothesized that the poly-(d,l)-lactide and calcium carbonate screw would degrade relatively fast with subsequent replacement with new bone in the canal.
Patients and methods
Ten patients were included according to the criteria’s in Table 1 in 2006 and were operated with ACL reconstruction from January to April 2007. The median age of the patients at the time of operation was 28 years (22–45 years). The study protocol was approved by the local ethical committee. They received ACL reconstruction with a bio-absorbable PLC interference screw as tibial fixation (Calaxo screw, Smith & Nephew Endoscopy, Andover, MA, USA). The femoral fixation was Rigidfix (Depuy Mitek, Raynham, MA). The patients underwent arthroscopic ACL reconstruction with semitendinosus/gracilis tendon graft. The patients were scanned with computed tomography (CT) 2 weeks and 1 year postoperatively.
All patients had ACL reconstruction using arthroscopically assisted technique. Gracilis and semitendinosus tendon was harvested through a small incision over the pes anserinus. All four strands were sutured separately with 2 Fiberwire sutures (Arthrex, Naples, FL).
Transtibial technique was used for femoral drilling. An oblique tibial drill hole starting at the anterior edge of the medial collateral ligament and ending in the ACL tibial footprint ensured a shallow and posterior femoral starting point for the femoral drill hole. A minimum 25 mm of the graft was placed in the femoral tunnel. In all patients had 35-mm long interference screw graft fixation in the tibia with the screw being 1 mm oversized compared to the drilled bone tunnel (drill diameter 8–10 mm). The screw was placed just inside the tibial cortex for optimal graft compression and fixation in the tibial tunnel. The femoral fixation was Rigidfix (Depuy Mitek, Raynham, MA).
All patients followed the same accelerated rehabilitation protocol. The rehabilitation allowed full weight bearing from first postoperative day and focused on early restoration of full extension and quadriceps function.
CT-scans were performed 2 weeks and 1 year postoperatively. The patients were placed in a supine position in a multi-slice CT scanner (Brilliance 64-slice, Philips Medical Systems, Cleveland, OH). Axial slices were made starting from the joint-space level to 1 cm distal from the cap of the screw. The scans were performed in high resolution with collimating on 64 × 0.625 mm, slice thickness 0.9 mm. Reformatting was performed a with C-filter resulting in a slice thickness of 5.0 and 1.0 mm spacing.
CT-evaluations were performed using the scanner-supplied software (Philips Medical Systems, Cleveland, OH). A reconstructed slice through the original drill hole canal along the direction of the screw was made. This direction was assessed on the 2-week postoperative images due to the possible lack of screw appearance 1 year after surgery. A tick was placed in the middle of the canal in the longitudinal direction of the screw and for every 5.0 mm a line was drawn on the square angle on the tick (Fig. 1). Curved reconstruction slices perpendicular to the direction of the drill hole canal were made. The diameter in the canal was measured in the horizontal and the vertical plane on these curved reconstruction slices between the osseous edges of the drill hole canal (Fig. 2).
The cross-sectional areas in the canal were calculated using the mean diameter between the horizontal and vertical measurement and the assumption of a circular formed canal. Tibial canal volume was calculated as stacked truncated cones using the six central cross-sectional areas, to measure the five central trunculated cones in the canal. Thus, we also bypassed the possible confounding irregularities in both ends of the canal. All bone canal volumes at 1-year follow-up were normalized to the volume of the drilled canal peroperatively based on drill diameter, due to the fact that different screw diameters were used. This is expressed as percentage of tunnel widening.
Postoperative control data included data from consultations in order to report the functional level of the patients as well as other unexpected occurrences.
CT data is presented as mean with 95% CI. For comparison, two-tailed paired T test were used between the two time points in the and a two-tailed Student’s t test to compare the two groups at 1-year follow-up. P values less than 0.05 were considered significant.
Results
All patients were available for CT scanning at the 1-year follow-up. The results of the CT scanning were not known to the doctors in the outpatient clinic at any of the consultations in the follow-up period. At the 1-year follow-up seven of the ten patients were able to exercise through running on a regular basis, but none of these had returned to contact sports. One patient had a small extension defect, one had problems with continuing the job as an archeologist, and one was scheduled for reoperation due to graft rupture. One had a lowered functional level with persistent medial joint pain and was diagnosed with pre-arthritic changes in the medial part of the knee joint with subchondral involvement.
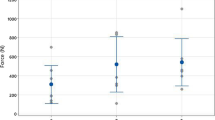
One year postoperative the screw was only visible in two out of ten cases. No unexpected granulomas or cysts were observed. Fourteen days postoperatively a mean tunnel widening of 78% [52%; 110%] was observed, which was a significant increase (P < 0.01). At the 1 year follow-up, the mean tunnel widening was 128% [84%; 180%] which was significantly higher than at baseline (P < 0.001) and 14 days postoperatively (P < 0.001) (Figs. 3, 4).
Discussion
The most important finding of this study was the rather disappointing observations of tibial tunnel widening after ALC reconstruction using this PCL interference screw. Clearly the findings on CT oppose the aim of this new interference screw to demonstrate ability to be remodeled into bone tissue in humans at 1 year follow-up. Several studies have described tunnel widening after ACL reconstruction and although the exact etiology is not known and might be multi-factorial, several important factors have been investigated. This has previously been discussed by Wilson et al. [37].
We found that majority of tunnel expansion after ACL reconstruction takes place during surgery when the tendons are compacted into the cancellous bone by oversized interference screw. In our study, the 14 days postoperative scannings demonstrated a 78% increase in tunnel volume due to the initial graft fixation method. This phenomenon has been demonstrated in previous studies [6, 25] and is not considered to be device related.
The search for explanations of these results is very important in understanding the mechanisms that should be taken into consideration when new materials for interference screws are being developed. Two issues need to be addressed in this context. First, why was the bioresorbable PLC screw not replaced by bone, at least partially replaced, since an experimental ovine study delivered promising results regarding this issue. Second, which circumstances lead to a subsequent or concurrent tunnel enlargement? There might be several explanations for this. It is a common fact that degradation of PLGA polymers leads to an acidification of the environment [10, 30]. This is an issue that has been addressed in several papers and although the acidification is a theoretical and experimental fact, the clinical importance can still be debated. Addition of calcium carbonate might contribute as a buffer to this, and thus manage to provide a pH neutral local environment, which has earlier been shown with the use of divalent cations [9, 39].
When results like ours needs to be explained, we have to turn to the previous works on this material. Using animal models is an essential part of developing compounds and products in tissue engineering. Even though several precautions are taken into consideration when testing an animal model for its clinical relevance, explanations of diverging results in relation to human trials can often be found in the inaccuracy of using animal models. The ovine study conducted by Walsh et al. [33] reports a partially replacement of bone in the bone canals already after 26 weeks postoperatively and complete substitution of the screw with bone after 1 year. Their study was well conducted but the authors only briefly discuss the limitations of their model for clinical use.
It is important to speculate on the limitations of the animal model to explain the unexpected findings in this present study. An editorial in Arthroscopy discusses this subject [19]. It is likely to presume that the biological breakdown of the PLC material does not vary between ovine and humans. The distinct important variable parameter between these two species is the osteogenetic rate. The osteogenetic capacity of 18-month-old sheep would indisputably be higher than in human subjects with a mean age of almost 32 years, which is also commented by Walsh et al. Skeletal maturity is not reached before the age of 36 month in ovines [22]. The bone remodeling at this age would then still only be considered moderately similar to humans [27]. Several studies describe large differences in bone composition between these two species [1, 8]. The hypothesis that would explain the undesirable events in our study is that fast degradation of the PLC interference screw which was not immediately replaced by bone, due to a slower bone metabolic activity in humans lead to an unstable situation with an increase in micro-motions of the tendons, that would further impair the environment for bone formation as seen around implants [11]. Early joint activation is a normal part of accelerated rehabilitation. Fibrous tissue formation and a tunnel enlargement were the subsequent result of this problem. In addition, the bone marrow tibia in young sheep consists of haemopoietic tissue with bone marrow-derived mesenchymal stem cells (MSC), and compared to humans the tibial bone marrow will be more inactive at the adult age. The bone density in the tibia is lower than in femur and therefore an implant as in this study that has adverse effect on tunnel widening should exert this effect more pronounced in the tibia.
Early rehabilitation has also been mentioned as a course of tunnel enlargement [12, 28]. Early rehabilitation might be responsible for a part of the tunnel widening occurring between surgery and the 14 days follow-up, but since tunnel widening was not described in the ovine study, also exposed to some extent of early rehabilitation, we find this explanation unlikely as a single factor. Both due to the above mentioned and due to the very distinct and consistent observation of tunnel widening in this study.
One reason for the withdrawal of the Calaxo screw was cases of aseptic cystic formation or granulomas in the proximal tibia. These cases were rare and are reported in less than 1% of all cases, which is why our small case series could have avoided this complication. Also the company emphasized that the screw should be fully embedded in bone to avoid soft tissue inflammation outside the tibial cortex. This issue indicated that the fast resorbing composite material of the Calaxo screw did have some adverse inflammatory effects [25].
One of the limitations in this study is the relatively low number of patients included, which disables this study from determining the clinical outcome of these patients. Although the tendency of the tunnel widening seems to be clear, it should be underlined that the conclusions in this study are based on a limited number of patients. The use of CT for evaluating the tibial bone canal is also limited by the fact that small isles of bone or osteogenetic foci of woven bone might not be detected, and hence there is a possibility that the osteoconductive properties of the screw and osteoinductive events in the canal could be underestimated. Due to the fact, that this was not even slightly evident on any of the scans, we find this highly unlikely. When assuming that early rehabilitation is responsible for the early observed tunnel widening, it should be taken into consideration that the tunnel size at baseline is not measured from CT. The limitations discussed above does not conflict with the observed results in the present study.
Conclusion
The use of PLC interference screws in humans did not result in bone formation in the tibial bone canal although the screw was degraded. One patient is scheduled for revision surgery due to graft failure, which could not be explained by the use of the PLC screw. We observed a significant tunnel enlargement during the 1-year follow-up, and can therefore conclude that tunnel enlargement is not only an issue with other resorbable polymer screws and metallic interference screws. In conclusion, the findings in this study clearly demonstrate that designing a resorbable screw that is replaced by bone tissue after ACL reconstructions is a huge challenge, and as clinician one must always be aware of possible side effects using biodegradable materials. Also, important limitations of preclinical biological data translating into clinical biology is clearly demonstrated.
References
Aerssens J, Boonen S, Lowet G, Dequeker J (1998) Interspecies differences in bone composition, density, and quality: potential implications for in vivo bone research. Endocrinology 139:663–670
Ahlstrom M, Pekkinen M, Riehle U, Lamberg-Allardt C (2008) Extracellular calcium regulates parathyroid hormone-related peptide expression in osteoblasts and osteoblast progenitor cells. Bone 42:483–490
Barber FA (2005) Poly-d, l-lactide interference screws for anterior cruciate ligament reconstruction. Arthroscopy 21:804–808
Barber FA, Dockery WD (2008) Long-term absorption of beta-tricalcium phosphate poly-l-lactic acid interference screws. Arthroscopy 24:441–447
Brand JC Jr, Nyland J, Caborn DN, Johnson DL (2005) Soft-tissue interference fixation: bioabsorbable screw versus metal screw. Arthroscopy 21:911–916
Buck DC, Simonian PT, Larson RV, Borrow J, Nathanson DA (2004) Timeline of tibial tunnel expansion after single-incision hamstring anterior cruciate ligament reconstruction. Arthroscopy 20:34–36
Dujardin J, Vandenneucker H, Bellemans J (2008) Tibial cyst and intra-articular granuloma formation after anterior cruciate ligament reconstruction using polylactide carbonate osteoconductive interference screws. Arthroscopy 24:238–242
Field RA, Riley ML, Mello FC, Corbridge MH, Kotula AW (1974) Bone composition in cattle, pigs, sheep and poultry. J Anim Sci 39:493–499
Fredenberg S, Reslow M, Axelsson A (2007) Effect of divalent cations on pore formation and degradation of poly(d, l-lactide-co-glycolide). Pharm Dev Technol 12:563–572
Fu K, Pack DW, Klibanov AM, Langer R (2000) Visual evidence of acidic environment within degrading poly(lactic-co-glycolic acid) (PLGA) microspheres. Pharm Res 17:100–106
Goodman SB (1994) The effects of micromotion and particulate materials on tissue differentiation. Bone chamber studies in rabbits. Acta Orthop Scand Suppl 258:1–43
Hantes ME, Mastrokalos DS, Yu J, Paessler HH (2004) The effect of early motion on tibial tunnel widening after anterior cruciate ligament replacement using hamstring tendon grafts. Arthroscopy 20:572–580
Honda Y, Anada T, Kamakura S, Nakamura M, Sugawara S, Suzuki O (2006) Elevated extracellular calcium stimulates secretion of bone morphogenetic protein 2 by a macrophage cell line. Biochem Biophys Res Commun 345:1155–1160
Honda Y, Fitzsimmons RJ, Baylink DJ, Mohan S (1995) Effects of extracellular calcium on insulin-like growth factor II in human bone cells. J Bone Miner Res 10:1660–1665
Kaeding C, Farr J, Kavanaugh T, Pedroza A (2005) A prospective randomized comparison of bioabsorbable and titanium anterior cruciate ligament interference screws. Arthroscopy 21:147–151
Kwak JH, Sim JA, Kim SH, Lee KC, Lee BK (2008) Delayed intra-articular inflammatory reaction due to poly-L-lactide bioabsorbable interference screw used in anterior cruciate ligament reconstruction. Arthroscopy 24:243–246
Lajtai G, Schmiedhuber G, Unger F, Aitzetmuller G, Klein M, Noszian I, Orthner E (2001) Bone tunnel remodeling at the site of biodegradable interference screws used for anterior cruciate ligament reconstruction: 5-year follow-up. Arthroscopy 17:597–602
Lembeck B, Wulker N (2005) Severe cartilage damage by broken poly-l-lactic acid (PLLA) interference screw after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 13:283–286
Lubowitz JH, Poehling GG (2008) Don’t know much biology: redux. Arthroscopy 24:127–129
Ma CB, Francis K, Towers J, Irrgang J, Fu FH, Harner CH (2004) Hamstring anterior cruciate ligament reconstruction: a comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy 20:122–128
Martinek V, Seil R, Lattermann C, Watkins SC, Fu FH (2001) The fate of the poly-l-lactic acid interference screw after anterior cruciate ligament reconstruction. Arthroscopy 17:73–76
Martini L, Fini M, Giavaresi G, Giardino R (2001) Sheep model in orthopedic research: a literature review. Comp Med 51:292–299
Mastrokalos DS, Paessler HH (2008) Allergic reaction to biodegradable interference poly-l-lactic acid screws after anterior cruciate ligament reconstruction with bone–patellar tendon–bone graft. Arthroscopy 24:732–733
McGuire DA, Barber FA, Elrod BF, Paulos LE (1999) Bioabsorbable interference screws for graft fixation in anterior cruciate ligament reconstruction. Arthroscopy 15:463–473
Myers P, Logan M, Stokes A, Boyd K, Watts M (2008) Bioabsorbable versus titanium interference screws with hamstring autograft in anterior cruciate ligament reconstruction: a prospective randomized trial with 2-year follow-up. Arthroscopy 24:817–823
Nakade O, Takahashi K, Takuma T, Aoki T, Kaku T (2001) Effect of extracellular calcium on the gene expression of bone morphogenetic protein-2 and -4 of normal human bone cells. J Bone Miner Metab 19:13–19
Reinwald S, Burr D (2008) Review of nonprimate, large animal models for osteoporosis research. J Bone Miner Res 23:1353–1368
Rodeo SA, Kawamura S, Kim HJ, Dynybil C, Ying L (2006) Tendon healing in a bone tunnel differs at the tunnel entrance versus the tunnel exit: an effect of graft–tunnel motion? Am J Sports Med 34:1790–1800
Segawa H, Omori G, Tomita S, Koga Y (2001) Bone tunnel enlargement after anterior cruciate ligament reconstruction using hamstring tendons. Knee Surg Sports Traumatol Arthrosc 9:206–210
Shenderova A, Burke TG, Schwendeman SP (1999) The acidic microclimate in poly(lactide-co-glycolide) microspheres stabilizes camptothecins. Pharm Res 16:241–248
Vuola J, Goransson H, Bohling T, Asko-Seljavaara S (1996) Bone marrow induced osteogenesis in hydroxyapatite and calcium carbonate implants. Biomaterials 17:1761–1766
Vuola J, Taurio R, Goransson H, Asko-Seljavaara S (1998) Compressive strength of calcium carbonate and hydroxyapatite implants after bone-marrow-induced osteogenesis. Biomaterials 19:223–227
Walsh WR, Cotton NJ, Stephens P, Brunelle JE, Langdown A, Auld J, Vizesi F, Bruce W (2007) Comparison of poly-l-lactide and polylactide carbonate interference screws in an ovine anterior cruciate ligament reconstruction model. Arthroscopy 23:757–765
Warden WH, Chooljian D, Jackson DW (2008) Ten-year magnetic resonance imaging follow-up of bioabsorbable poly-l-lactic acid interference screws after anterior cruciate ligament reconstruction. Arthroscopy 24(370):e371–e373
Warden WH, Friedman R, Teresi LM, Jackson DW (1999) Magnetic resonance imaging of bioabsorbable polylactic acid interference screws during the first 2 years after anterior cruciate ligament reconstruction. Arthroscopy 15:474–480
Weiler A, Hoffmann RF, Stahelin AC, Helling HJ, Sudkamp NP (2000) Biodegradable implants in sports medicine: the biological base. Arthroscopy 16:305–321
Wilson TC, Kantaras A, Atay A, Johnson DL (2004) Tunnel enlargement after anterior cruciate ligament surgery. Am J Sports Med 32:543–549
Zantop T, Weimann A, Schmidtko R, Herbort M, Raschke MJ, Petersen W (2006) Graft laceration and pullout strength of soft-tissue anterior cruciate ligament reconstruction: in vitro study comparing titanium, poly-d,l-lactide, and poly-d,l-lactide-tricalcium phosphate screws. Arthroscopy 22:1204–1210
Zhu G, Mallery SR, Schwendeman SP (2000) Stabilization of proteins encapsulated in injectable poly (lactide-co-glycolide). Nat Biotechnol 18:52–57
Acknowledgment
This study was financially supported by Smith and Nephew, Denmark.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Foldager, C., Jakobsen, B.W., Lund, B. et al. Tibial tunnel widening after bioresorbable poly-lactide calcium carbonate interference screw usage in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 18, 79–84 (2010). https://doi.org/10.1007/s00167-009-0865-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0865-2