Abstract
Patient activity level may be an important prognostic variable relating to outcome in patients with shoulder disorders. The purpose of this cross-sectional study was to test the hypothesis that a shoulder activity scale will detect differences in shoulder activity based on the patient diagnosis and age. A total of 157 patients of four academic orthopedic surgeons with a diagnosis of rotator cuff disease (86), glenohumeral instability (31) or osteoarthritis (40) were asked to fill out a previously validated shoulder activity scale and the ASES shoulder questionnaire. The patient’s diagnosis, gender and age were recorded. The activity level was significantly higher in patients with instability than in patients with rotator cuff disease or osteoarthritis. Patients with rotator cuff disease were significantly more active than patients with osteoarthritis. Linear regression of activity level on patient age and diagnosis demonstrated a statistically significant relationship between activity level and both independent variables. Diagnosis influenced activity level independent of age. This is the first study to document diagnosis-based differences in the shoulder activity level of patients with different shoulder disorders. Shoulder activity level should be evaluated as a prognostic variable in studies of patients with shoulder disorders that may predict outcome and guide treatment in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past two decades measurement tools for evaluating patient function have become more common in orthopedics [23]. Most tools are designed to quantify patient symptoms and/or functional disability because other traditional measures (such as strength or range of motion) used by physicians do not capture this data. Although symptoms and function relate to patient activity level, these measures do not specifically capture the patient’s activity level. Function typically reflects how well a patient performs certain tasks, while activity level measures how much a patient does.
The use of activity scales in orthopedics is growing, and a variety of activity rating scales are available for disorders of the knee [3, 13, 16, 19, 24] and ankle [6]. There is a need for a validated questionnaire evaluating patient activity for the shoulder [4], particularly since activity level may be an important confounding factor in clinical studies. In any study comparing two or more groups of patients, the activity level of the groups should be similar to avoid a biased comparison [13]. These scales are important not only to differentiate highly active athletes from sedentary arthritis patients, but also to make distinctions within subgroups, such as highly active post-arthroplasty patients from household ambulators, or adult recreational competitors versus elite professional athletes, each of which may warrant separate analysis.
Two patients with different levels of activity may have similar levels of pain (symptoms) and limitations of function after an identical injury. However, their postoperative outcome could be different based on their level of activity for several reasons. Patient level of activity may influence healing after surgery. For example, an overhead painter will stress a rotator cuff repair more heavily than a sedentary retiree. Although symptoms and function relate, activity level may also influence patient perception of treatment success. If treatment relieves night pain for a low activity patient, they may be satisfied with the outcome. However, a more active patient may expect restoration of previous activity level to reach a similar level of satisfaction. Thus, patient activity level could be an important prognostic variable relating to outcome.
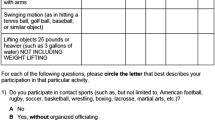
A scale for measuring the level of shoulder activity (Fig. 1) has been validated in a healthy population [2]. Our hypothesis was that this shoulder activity scale would detect differences in shoulder activity between patient cohorts with different shoulder disorders based on the age and diagnosis. The purpose of this study was to use this scale in a population of patients with shoulder disorders to compare the activity level of patients with different disorders.
Materials and methods
Approval from the Institutional Review Board at both study sites was obtained for this investigation. The diagnoses included in this study were isolated shoulder instability, osteoarthritis and rotator cuff disease (diagnosed clinically as impingement, partial thickness cuff tear or full thickness cuff tear), diagnosed in the office by the participating orthopedic surgeons based on the history, physical examination and imaging studies. Patients with findings suggestive of other concomitant shoulder pathology such as acromioclavicular joint osteoarthritis or biceps tendonitis were excluded. Patients with a history of previous shoulder surgery were excluded. Patients of four orthopedic surgeons from two separate orthopedic institutions were asked if they would be willing to participate in this study. If they agreed to participate, informed consent was obtained and the patients completed the ASES [17] and shoulder activity scale [2]. The patient’s diagnosis, gender and age were recorded.
Summary statistics were recorded for patient age and activity level by diagnosis. The variance of the activity level was tested for homogeneity and an ANOVA was performed. Post hoc Tukey t tests were used to compare the activity level between different diagnoses. The percent of patients involved in contact and overhead sports was calculated by diagnosis and compared across diagnoses using the chi-square test. A linear regression model was calculated with activity level as the dependent variable, with age and diagnosis as the independent variables. The statistical analysis was performed using SPSS 14.0 (Chicago, Ill).
Results
A total of 157 patients (95 males, 62 females), including 86 with rotator cuff disease (47 male, 39 female), 40 with osteoarthritis (26 males, 14 female) and 31 with instability (22 male, 9 female), enrolled in the study. Overall, the median age of study participants was 55.2 ± 18.6 years (range 16–88). On diagnosis, the median age of patients with rotator cuff disease was 52.5 ± 13.7 years (range 26–80) compared with 70.2 ± 9.5 (range 45–88) for osteoarthritis patients and 24.8 ± 11.1 (range 16–58) for instability patients. The mean ASES scores were 38.2 ± 23.4 for patients with rotator cuff disease, 48.3 ± 19.4 for the osteoarthritis cohort and 67.9 ± 22.1 for instability patients.
Linear regression of activity level on patient age and diagnosis demonstrated a statistically significant relationship between activity level and both independent variables (P < 0.001). Among patients <30 years of age, the median activity level was 14 ± 4.0 (activity scores on this scale range from 0 to 20). This decreased to 10 ± 5.2 in patients age 30–50, 9 ± 4.9 for patients in the age range of 50–70 and 6.5 ± 5.5 in patients over 70 years of age. Although 29% of patients under 30 and 21% of patients age 30–50 had a high level of shoulder activity (>15), approximately 10% of patients over the age of 50 maintained a high level of shoulder activity (Fig. 2). No patients under the age of 30 had a low level of shoulder activity (<5) compared with almost 40% of patients over 70.
The activity level was significantly higher in patients with instability (14 ± 5.2, range 1–20) than in patients with rotator cuff disease (10 ± 5.1, range 0–20) (P = 0.027) or osteoarthritis (7 ± 4.7, range 0–18) (P < 0.001). Patients with rotator cuff disease were significantly more active than patients with osteoarthritis (P < 0.01). Thirty-two percent of patients with instability had a high level of activity of 16–20, compared with 16% of patients with rotator cuff disease and <3% of patients with osteoarthritis (Fig. 3). Conversely, 35% of patients with osteoarthritis had a low activity level of 0–5, compared with 21% of rotator cuff patients, and <11% of instability patients.
Patients with instability were more likely to play contact sports (50%) than patients with rotator cuff disease (6%) or osteoarthritis (0%) (P < 0.001). They were also more likely to participate in sports involving overhead activity such as throwing or swimming (instability 60%, rotator cuff disease 26%, osteoarthritis 3%) (P < 0.001).
Discussion
The shoulder activity scale studied herein detected significant differences in activity level based on the shoulder disorder and patient age. This is the first study to compare the activity level of patients with different shoulder disorders. Our hypothesis that the shoulder activity scale would detect differences in shoulder activity between patient cohorts with different shoulder disorders was confirmed. As might be expected, instability patients tend to be the most active patients, whereas osteoarthritis patients are the least active patients. Activity level also varied by age in a sensible pattern, as younger patients had a higher activity level and older patients tended to be less active. Even with a strong correlation between diagnosis and patient age, the type of shoulder disorder had an effect on shoulder activity independent of age. These findings further validate this shoulder activity scale as an appropriate tool for assessing patients with shoulder disorders. Although these findings may appear intuitive, this is the first study to document quantitative differences in shoulder activity level by age and diagnosis in patients with shoulder disorders.
Furthermore, the distribution of activity level by diagnosis is a significant finding because this variability suggests that activity level should be studied for potential prognostic value. Shoulder activity level may have predictive value in patients with a given shoulder disorder, since there was variability among patients with each of the three diagnoses studied. A sizable percentage of patients with rotator cuff disease and instability demonstrated a relatively low level of shoulder activity (<5). Numerous rotator cuff patients and even a few osteoarthritis patients demonstrated a relatively high level of shoulder activity (>15). This wide distribution of activity level across patients with the same diagnosis suggests that activity level should be investigated as a possible prognostic factor. Within a given study of outcome for a treatment, such as total shoulder arthroplasty, the activity of the patients and therefore their expectations and outcomes may vary widely. By documenting their activity prior to treatment, i.e. surgery, the effect of treatment can be interpreted in the appropriate context. Activity level can also be used to assess outcome, by comparing a patient’s postoperative activity to their preoperative activity level.
Activity level was correlated with age as might be expected, yet there was variability among patients at different age levels, just as there was for each diagnosis. Patients under 30 were definitely more active than older patients, as no one under 30 had an activity level <5 and 72% of those under 30 had an activity level >10 compared with 49% of those 30–50, 41% of those 50–70 and 36% of those over 70. However, 10% of those 50–70 and 12% of those over 70 exhibited a relatively high activity level (>15). This distribution of activity level across patients of similar ages, even for older patients, suggests that activity level adds important descriptive information to cohorts of patients with shoulder disorders.
Although our patients were selected on the basis of clinical diagnosis by the investigators, the mean ASES scores suggest that the degree of disease pathology was consistent with that previously described in the literature. For example, the mean ASES score of 43.3 ± 23.4 for rotator cuff disease in our study population was similar to the mean preoperative rotator cuff scores from Kocher et al. [8] (51.3 ± 18.6), Baysal et al. [1] (53.3 ± 20.6) and Skutek et al. [22] (33.9 ± 15.9). Similarly, the mean ASES score of 68.0 ± 22.1 in our instability patients was similar to the mean instability scores from Kocher et al. [8] (64.0 ± 22.7). Our osteoarthritis scores (41.1 ± 19.4) were between previously published values of Lo et al. [11] (hemiarthroplasty 31.1 ± 16.6; total shoulder arthroplasty 30.7 ± 19.5) and Kocher et al. [8] (56.5 ± 19.3).
Studies have found that activity level can be an important prognostic variable for patients with disorders of the knee [12]. For example, the Marx knee activity rating scale has been shown to be useful in helping to determine which patients have a better chance of returning to preinjury activity levels after ACL reconstruction [5]. This may also be true in the shoulder. A recent prospective study of traumatic anterior shoulder instability by Sachs et al. [18] reported a strong trend towards higher recurrence rates in patients with occupational use of the arm at or above shoulder level and participation in collision/contact sports. More active patients may face a higher risk of recurrent instability, persistent rotator cuff or arthritis symptoms.
The level of activity may also be an important variable with regards to arthroplasty. In the knee, activity has been shown to correlate with increased implant wear [9, 10], which may influence implant durability [20, 21]. In the shoulder, the preoperative level of activity may be relevant to postoperative activity level and patient satisfaction, as well as the survivorship of the prosthesis. Patients have been shown to remain active after shoulder arthroplasty [14].
As mentioned previously, activity level can also be used to help assess patient outcome. For example, in the knee, the Marx activity scale has been shown to improve significantly after microfracture [15]. Activity is very important to patients after total knee arthroplasty [7, 25, 26], and activity levels have been shown to increase significantly within 6 months of revision total knee arthroplasty as well [19].
A limitation of this study is the lack of strict criteria for the severity of pathology in enrolled patients (i.e. rotator cuff tendonitis versus partial thickness or full thickness rotator cuff tear). However, the purpose of this study was not to precisely define diagnostic subgroups, but rather to assess the range of shoulder activity in patients across diagnostic categories. As mentioned previously, the distribution of ASES scores in our diagnostic cohorts is consistent with previously published results. Further investigation of shoulder activity level within well-defined patient cohorts may be warranted to investigate these issues further.
Conclusion
In conclusion, the shoulder activity scale studied herein [2] demonstrates diagnosis and age-related differences in activity level. Younger patients have a higher activity level than older patients when controlled for diagnosis. Osteoarthritis patients are the least active, and rotator cuff patients are less active than instability patients. Although diagnosis was correlated with age, diagnosis had an effect on activity level that was independent of patient age. This is the first study to document these expected relationships of shoulder activity to patient age and diagnosis. Another significant finding was the sufficient variance in the activity level, even within age- and diagnosis-matched cohorts, to suggest that shoulder activity level may be useful as a prognostic variable for the evaluation of patients with shoulder disorders. Future studies should investigate whether shoulder activity level can be used to predict outcome and guide treatment in patients with shoulder disorders.
References
Baysal D, Balyk R, Otto D, Luciak-Corea C, Beaupre L (2005) Functional outcome and health-related quality of life after surgical repair of full-thickness rotator cuff tear using a mini-open technique. Am J Sports Med 33:1346–1355. doi:10.1177/0363546505275130
Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG (2005) Measurement of shoulder activity level. Clin Orthop Relat Res 439:101–108. doi:10.1097/01.blo.0000173255.85016.1f
Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR (1994) Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med 22:632–644. doi:10.1177/036354659402200511
Dorey FJ, Amstutz HC (2001) The need to account for patient activity when evaluating the results of total hip arthroplasty with survivorship analysis. J Bone Joint Surg Am 84:709–710
Gobbi A, Francisco R (2006) Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc 14:1021–1028. doi:10.1007/s00167-006-0050-9
Halasi T, Kynsburg A, Tallay A, Berkes I (2004) Development of a new activity score for the evaluation of ankle instability. Am J Sports Med 32:899–908. doi:10.1177/0363546503262181
Healy WL, Iorio R, Lemos MJ (2000) Athletic activity after total knee arthroplasty. Clin Orthop Relat Res 380:65–71. doi:10.1097/00003086-200011000-00009
Kocher MS, Horan MP, Briggs KK, Richardson TR, O’Holleran J, Hawkins RJ (2005) Reliability, validity, and responsiveness of the American Shoulder and Elbow Surgeons subjective shoulder scale in patients with shoulder instability, rotator cuff disease, and glenohumeral arthritis. J Bone Joint Surg Am 87:2006–2011. doi:10.2106/JBJS.C.01624
Kuster MS, Stachowiak GW (2002) Factors affecting polyethylene wear in total knee arthroplasty. Orthopedics 25:s235–s242
Lavernia CJ, Sierra RJ, Hungerford DS, Krackow K (2001) Activity level and wear in total knee arthroplasty: a study of autopsy retrieved specimens. J Arthroplasty 16:446–453. doi:10.1054/arth.2001.23509
Lo IK, Litchfield RB, Griffin S, Faber K, Patterson SK, Kirkley A (2005) Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis. A prospective, randomized trial. J Bone Joint Surg Am 87:2178–2185. doi:10.2106/JBJS.D.02198
Marx RG (2003) Knee rating scales. Arthroscopy 19:1103–1108. doi:10.1016/j.arthro.2003.10.029
Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF (2001) Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med 29:213–218
McCarty EC, Marx RG, Maerz D, Altchek D, Warren RF (2008) Sports participation following shoulder replacement surgery. Am J Sports Med 36:1577–1581. doi:10.1177/0363546508317126
Mithoefer K, Williams RJ 3rd, Warren RF, Wickiewicz TL, Marx RG (2006) High-impact athletics after knee articular cartilage repair: a prospective evaluation of the microfracture technique. Am J Sports Med 34:1413–1418. doi:10.1177/0363546506288240
Noyes FR, Barber SD, Mooar LA (1989) A rationale for assessing sports activity levels and limitations in knee disorders. Clin Orthop Relat Res 246:238–249
Richards RR, An KN, Bigliani LU et al (1994) A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg 3:347–352. doi:10.1016/S1058-2746(09)80019-0
Sachs RA, Lin D, Stone ML, Paxton E, Kuney M (2007) Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am 89:1665–1674. doi:10.2106/JBJS.F.00261
Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buvea CM, Krackow KA (2005) Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am 87:1985–1994. doi:10.2106/JBJS.D.02564
Schmalzried TP, Shepherd EF, Dorey FJ et al (2000) Wear is a function of use, not time. Clin Orthop Relat Res 381:36–46. doi:10.1097/00003086-200012000-00005
Schmalzried TP, Szuszczewicz ES, Northfield MR et al (1998) Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am 80:54–59. doi:10.1302/0301-620X.80B1.7739
Skutek M, Fremerey RW, Zeichen J, Bosch U (2000) Outcome analysis following open rotator cuff repair. Early effectiveness validated using four different shoulder assessment scales. Arch Orthop Trauma Surg 120:432–436. doi:10.1007/s004020000133
Swiontkowski MF, Buckwalter JA, Keller RB, Haralson R (1999) The outcomes movement in orthopaedic surgery: where we are and where we should go. J Bone Joint Surg Am 81:732–740. doi:10.1302/0301-620X.81B6.9794
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Weiss JM, Noble PC, Conditt MA et al (2002) What functional activities are important to patients with knee replacements? Clin Orthop Relat Res 404:172–188. doi:10.1097/00003086-200211000-00030
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC (1998) Assessing activity in joint replacement patients. J Arthroplasty 13:890–895. doi:10.1016/S0883-5403(98)90195-4
Acknowledgments
The authors of this paper have no financial relationship with any organization relating to this study. We have full control of all primary data and agree to allow the journal to review this data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brophy, R.H., Levy, B., Chu, S. et al. Shoulder activity level varies by diagnosis. Knee Surg Sports Traumatol Arthrosc 17, 1516–1521 (2009). https://doi.org/10.1007/s00167-009-0820-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-009-0820-2