Abstract
According to literature, knee arthroscopy is a minimal invasive surgery performed for minor surgical trauma, reduced morbidity and shortens the hospitalization period. Therefore, this type of surgery before total knee arthroplasty (TKA) could be considered a minor procedure with minimum postoperative complication. A retrospective and cohort series of 1,474 primary TKA was performed with re-assessment after a minimum follow-up period of 2 years: 1,119 primary TKA had no previous surgery (group A) and 60 primary TKA had arthroscopic debridement (group B). All the patients underwent a clinical and radiological evaluation as well as IKS scores. Statistical analysis of postoperative complications revealed that group B had a higher postoperative complication rate (P < 0.01). In this group, 30% of local complications were re-operated and 8.3% of these cases underwent revision TKA (P < 0.01). The mean interval between arthroscopy and primary TKA was 53 months. However, statistical analysis did not reveal a direct correlation between arthroscopy/primary TKA interval and postoperative complications/failures (P = 0.55). The Kaplan–Meier survival curves showed a survival rate of 98.1 and 86.8% at 10 years follow-up for groups A and B, respectively. Our data allow us to conclude that previous knee arthroscopy should be considered a factor related to postoperative primary TKA outcomes as demonstrated by the higher rate of postoperative complications and failures (P < 0.001) as well as a worse survival curve than group A.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroscopy is a valuable tool for treating mechanical symptoms related to early stages of knee arthritis with satisfactory postoperative clinical results. According to Pagnano et al. [14], Miller et al. [11] and McGinley et al. [10], arthroscopic procedures can improve clinical symptoms and delay total knee arthroplasty (TKA) intervention, even in middle-aged and geriatric populations [21].
At later stages of arthritis, total knee arthroplasty is presented as a predictable and reproducible surgical procedure having an estimated mean implant life of 10 years in 92% of the cases. World literature cites the clinical efficacy of this surgical intervention in improving adverse symptoms of arthritis with even total elimination of pain and better range of motion, promoting independence and improved quality of life [2, 5, 20].
However, it must be underscored that previous knee surgery is associated with surgical difficulties and postoperative complications in the case of primary TKA on the same knee [4]. Previous surgeries such as tibial or femoral osteotomy, distal patellar–femoral re-alignment, osteosynthesis of tibial plateau or distal femoral fractures could result in poor postoperative clinical scores in primary TKA as compared to cases without previous knee surgery.
In the literature, the role of arthroscopy as a previous surgical procedure in primary TKA has not yet been established. Arthroscopy is a minimal invasive surgery performed for minor surgical trauma, reduced morbidity and shortens hospitalization period when compared with other surgical interventions. Hence, this type of surgery before TKA could be considered a minor surgical procedure with minimum postoperative complications.
Therefore, is previous knee arthroscopy related to worse results in primary TKA?
Materials and methods
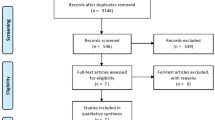
From March 1988 to August 2005, 1,474 primary TKA were performed in our department. The posterior-stabilized tricompartmental TKA with one-third medial condyle (Tornier®, Saint Ismier, France) was used.
A retrospective and cohort study analyzed two distinct groups of patients. In one group of 1,119 primary TKA (1,035 patients) (group A) had no previous knee surgery, while 60 primary TKA (60 patients) (group B) had undergone previous arthroscopy. Tables 1, 2, 3 present the percentage distribution of patients according to age, sex, side, and body mass index (BMI), the etiological diagnosis and type of knee arthritis in groups A and B, respectively. The interval between arthroscopy surgery and primary TKA was variable, ranged from a minimum interval period of 4 months and a maximum of 120 months (mean interval of 53 months).
All the patients underwent a prior systematic assessment that included a clinical examination, radiographs [bipodal hip–knee–ankle film (pangonogram) [12], anteroposterior knee view with monopodal support, posteroanterior view at 45° knee flexion, lateral view at 30° knee flexion, patellar axial at 30° knee flexion, stress valgus and varus X-ray using a Telos® system] and International Knee Society (IKS) knee and functional scores [7]. Blackburne–Peel index (BPI) [3] was used as radiological measure for determining pre and postoperative patellar height. Pre and postoperative patella position in the radiographic axial view at 30° knee flexion were evaluated.
In our series of cases, the clinical and radiological data for each patient were obtained at the latest follow-up before any revision TKA.
In group A, the medial approach was used in 974 cases (87%) involving 10 cases of tibial tubercle osteotomy, the lateral approach in 134 cases (12%) involving 64 cases of tibial tubercle osteotomy and anterolateral approach was used in 11 cases (1%).
However, in group B, the medial approach was used in 53 cases (88.3%) involving 1 case of tibial tubercle osteotomy, the lateral approach was used in 7 cases (11.7%) involving 4 cases of tibial tubercle osteotomy.
The mean duration of surgery was 86.19 and 105.38 min for groups A and B, respectively. No difference was found for both study groups (P = 0.34).
Statistical analysis
In our primary TKA series, the statistical analysis of certain variables showed that these two study groups of patients were similar (regarding some characteristics), and the ANOVA confirmed that these groups could be comparable (no statistical difference for height, weight, BMI and sex distribution). The data obtained underwent statistical analysis with Minitab® Statistical Software Package (Minitab Ltd. State, Brandon Court, Unit E1, State College, Pennsylvania). In this statistical analysis, the limit of significance considered was 5%.
Results
During the postoperative follow-up, 86 patients (8%) were lost from the original group A and 949 patients (992 primary TKA) were re-assessed regularly. In group B one patient (2%) was lost and 59 cases (98%) re-assessed. The mean follow-up period was 43.2 months (24–193) and 46.6 months (24–140), respectively for groups A and B.
Knee range of motion
When comparing groups A and B, the preoperative mean knee range of motion data for hyperextension, lag of extension and hyperflexion were respectively, 0.4°/4°/116° and 0.5°/5°/115° (P = 0.76, P = 0.4 and P = 0.47, respectively). Likewise, in the postoperative evaluation, the mean knee range of motion was statistically similar for both study groups: 0.7°/0.5°/118° and 0.9°/0.2°/117° respectively, in the groups A and B (P = 0.5, P = 0.5 and P = 0.5, respectively).
IKS knee and functional scores
The pre and postoperative IKS knee score did not differ for both A and B study groups (P = 0.6 and P = 0.23, respectively). In the same way, pre and postoperative IKS functional score showed no difference between both study groups (P = 0.11 and P = 0.10, respectively). The mean IKS knee and functional scores are presented in Table 4.
Level of pain
The statistical analysis of preoperative evaluation of both study groups showed no difference. However, the postoperative evaluation of both study groups showed that the distribution of patients classified as no pain and severe level of pain differed (P < 0.03 and P < 0.003, respectively) (Table 5).
Radiological evaluation
In group A, arthritis was radiologically classified according to Ahlbäck’s classification [1], in 1% of the cases as stage 1, 24%—stage 2, 47%—stage 3 and 28% of the cases as stage 4. In group B, the cases were classified as stages 1–4 in 6.5, 33, 54 and 6.5%, respectively.
Statistical analysis showed a difference in distribution of cases classified as stages 1 and 4 in groups A and B (P = 0.01 and P = 0.01, respectively). On the other hand, there was no difference between cases classified as stages 2 and 3 in both study groups.
The pangonogram radiograph measured knee malalignment and the percentage values were grouped under four intervals: 0°–3°; 4°–6°; 7°–9° and above 9° are presented in Table 6.
Patella position in the radiographic axial view
The percentage values of pre and postoperative of patella position in the radiographic axial view at 30° knee flexion and statistical analysis are presented in Table 7.
Patella height
The pre and postoperative mean values of patella height measured by Blackburne–Peel index [3] in the lateral radiographic at 30° knee flexion were respectively 0.76 and 0.60 for group A; 0.75 and 0.59 for group B. Statistical analysis showed no difference in both study groups in the pre and postoperative values (P = 0.5 and P = 0.48, respectively).
Intraoperative complications
Tibial plateau or femur fissures (minor and non-displaced fracture) and collateral ligaments damage (partial tear, never a complete disruption) were the most frequent intraoperative complications in primary TKA surgery. Intraoperative complications were reported in 44 cases of group A (4%) and 4 cases of group B (7%). However, statistical analysis showed no difference between both study groups (P = 0.3).
Postoperative complications
At the mean postoperative follow-up of 43.2 months, we identified 103 complications in group A (10% of the cases in this group). A second surgical intervention was performed in 80 cases (79%) and prosthetic component replacement was performed in 33 cases (41% of these cases).
At the mean postoperative follow-up of 46.6 months, we registered 18 complications in group B (30% of the cases in this group). 100% of these cases underwent another surgical intervention and in 39% of these cases (7 cases), the prosthetic components were replaced.
Regarding the same type of postoperative complications (Table 8), we observed that group B had a higher rate of postoperative complications and percentage of prosthetic components replacement when compared to group A (P < 0.001 and P < 0.001).
Survival rates
At 120 months follow-up, the Kaplan–Meier curve showed a 98.1% survival rate (95% confidence interval, 99.1–97.1%) for group A, while group B had 86.8% survival rate (95% confidence interval, 99.5–74.1%).
Discussion
Scher et al. [17] and Jerosch et al. [8] emphasize that arthroscopic management is an effective method proposed for the treatment of some postoperative TKA complications, such as knee stiffness, painful TKA (patellar clunk syndrome and painful patellofemoral crepitus), intraarticular loose body and pseudomeniscus. Similarly, Klinger et al. [9] states that arthroscopy could be useful in relieving pain, improving knee function and even, in elucidating undiagnosed cases of painful knee arthroplasty.
Although knee arthroscopy is considered a minimal invasive surgery on a native knee, it is not free from postoperative complications. Sherman et al. [19] in a retrospective review of 2,640 patients reported 8.2% postoperative complications, of which 58% were classified as major complications such as infections, hemarthrosis, adhesions, instrument breakage, cardiovascular and neurological problems.
On the other hand, previous knee surgery seems to be related to inferior clinical and functional postoperative results as well as postoperative primary TKA complications. Nelson et al. [13] concluded that TKA after varus osteotomy of the distal femur is a technically demanding procedure and associated with inferior clinical results when compared with those of primary TKA without previous osteotomy. Similarly, Parvizi et al. [16] reported that primary TKA after high tibial osteotomy presented a high rate of radiographic evidence of TKA loosening. Analyzing primary TKA in patients with previous distal femoral fracture, Papadopoulos et al. [15] observed that these cases resulted in restricted range of motion and intraoperative complications.
But in fact, the influence of arthroscopy as previous surgery in the outcome of primary TKA has not been reported.
In our work, the groups A and B presented no different characteristics regarding sex, side, BMI and type of knee arthritis (Tables 1, 3). Similarly, in both study groups, the main etiological diagnoses were arthritis, followed by inflammatory rheumatism. Moreover, preoperative evaluation IKS knee and functional scores and knee range of motion did not differ. The mean age of group B was 3 years less than group A (P < 0.001). In relation to the stage of arthritis, 75% of cases in group A and 60% of group B were classified as stages 3 and 4. Statistical analysis showed a prevalence of stage 4 cases in group A.
In our series, 52 and 57% of cases presented knee malalignment superior to 7º in groups A and B, respectively (P = 0.35). However, postoperative evaluation showed that surgery improved the knee alignment and no difference was found in both groups (Table 6).
As shown by some authors [6, 18], intraoperative complications during primary TKA (tibia or femur fracture, disruption of collateral ligament or even patellar tendon disruption) could influence postoperative outcome. However, in our series of cases, this occurrence was not identified in group B (P = 0.3).
Improved preoperative of IKS knee and functional scores were 107 and 43% for group A and 96 and 45% for group B. The statistical analysis showed no difference in improved IKS knee and functional scores (P = 0.2 and P = 0.4, respectively).
Despite the fact that there was no statistical difference in IKS knee and functional scores in our series, group B presented a higher rate of postoperative complications when compared to group A (P < 0.001) (Table 8 presents patella baja, patella fracture, anterior tibial tubercle fracture, TKA loosening and stiffness as postoperative complications in group B). This was demonstrated by the fact that 30% of the cases were re-operated in group B and 8.3% of these cases were submitted to revision TKA, while only 4% of cases in group A were re-operated and 1.4% underwent surgical revision (P < 0.001 and P < 0.001, respectively). These results are also confirmed by the Kaplan–Meier survival curves, with a survival rate of 98.1 and 86.8% at 10 years follow-up for groups A and B, respectively.
In group B, the mean interval between arthroscopy and primary TKA was 53 months. In this group, we observed that in 57% of the cases the mean interval was 25.6 months. However, in this study, statistical analysis did not demonstrate a direct correlation between arthroscopy and primary TKA interval and postoperative complications and failures (P = 0.55). Although the mechanism involved remains to be clarified, we hypothesized that knees with more inflammatory soft tissue (group B) could be related to higher postoperative complications and failure rates.
Even though, our results did not identify the mechanism by which previous knee arthroscopy influences primary TKA outcome, these data have motivated us to follow-up this study and conduct further extensive studies on patients who have undergone primary TKA after other knee surgeries on the same knee.
Conclusion
Our data allow us to conclude that previous knee arthroscopy should be considered a factor related to postoperative primary TKA outcomes as demonstrated by the higher rate of postoperative complications and failures (P < 0.001) as well as a worse survival curve than group A.
References
Ahlbäck S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) Suppl 277:7–72
Archibeck MJ, White RE Jr (2004) What’s new in adult reconstructive knee surgery. J Bone Joint Surg Am 86:1839–1849
Blackburne JS, Peel TE (1977) A new method of measuring patellar height. J Bone Joint Surg Br 59:241–242
Burki H, von Knoch M, Heiss C, Drobny T, Munzinger U (1999) Lateral approach with osteotomy of the tibial tubercle in primary total knee arthroplasty. Clin Orthop Relat Res 362:156–161
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 86:963–974
Gandhi R, Beer DEJ, Leone J, Petruccelli D, Winemaker M, Adili A (2006) Predictive risk factors for stiff knees in total knee arthroplasty. J Arthroplasty 21:46–52
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Jerosch J, Aldawoudy AM (2007) Arthroscopic treatment of patients with moderate arthrofibrosis after total knee replacement. Knee Surg Traumatol Arthrosc 15:71–77
Klinger HM, Baums MH, Spahn G, Ernstberger T (2005) A study of effectiveness of knee arthroplasty after arthroplasty. Arthroplasty 21:731–738
McGinley BJ, Cushner FD, Scott WN (1999) Debridement arthroscopy. 10 year follow-up. Clin Orthop Relat Res 367:190–194
Miller BS, Steadman JR, Briggs KK, Rodrigo JJ, Rodkey WG (2004) Patient satisfaction and outcome after of the degenerative knee. J Knee Surg 17:13–17
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone and Joint Surgery Am 69:745–749
Nelson CL, Saleh KJ, Kassim RA, Windsor R, Haas S, Laskin R, Sculco T (2003) Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg Am 85:1062–1065
Pagnano MW, Clarke HD, Jacofsky DJ, Amendola A, Repici JA (2005) Surgical treatment of the middle-aged patient with arthritic knees. Instr Course Lect 54:251–259
Papadopoulos EC, Parvizi J, Lai CH, Lewallen DG (2002) Total knee arthroplasty following prior distal femoral fracture. Knee 9:267–274
Parvizi J, Hansen AD, Spangehl MJ (2004) Total knee arthroplasty following proximal tibial osteotomy: risk factors for failure. J Bone Joint Surg Am 86:474–479
Scher DM, Paumier JC, Di Cesare PE (1997) Pseudomeniscus following total knee arthroplasty as a cause of persistent knee pain. J Arthroplasty 12:114–118
Schoderbek RJ Jr, Brown TE, Mulhall KJ, Mounasamy V, Iorio R, Krackow KA, Macaulay W, Saleh KJ (2006) Extensor mechanism disruption after total knee arthroplasty. Clin Orthop Relat Res 446:176–185
Sherman OH, Fox JM, Snyder SJ, Del Pizzo W, Friedman MJ, Ferkel RD, Lawley MJ (1986) Arthroscopy—“no problem surgery”. An analysis of complications in two thousand six hundred and forty cases. J Bone Joint Surg Am 86:256–265
Weir DJ, Moran CG, Pinder IM (1996) Kinematic condylar total knee arthroplasty.14-year survivorship analysis of 208 consecutive cases. J Bone Joint Surg Br 78:907–911
Yang SS, Nisonson B (1995) Arthroscopy surgery of the knee in the geriatric patient. Clin Orthop Relat Res 316:50–58
Acknowledgment
Sérgio Rocha Piedade was supported by the Post Doctorate Scholarship by CNPq, National Council for Scientific and Technological Development, Brazil.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Piedade, S.R., Pinaroli, A., Servien, E. et al. Is previous knee arthroscopy related to worse results in primary total knee arthroplasty?. Knee Surg Sports Traumatol Arthrosc 17, 328–333 (2009). https://doi.org/10.1007/s00167-008-0669-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0669-9