Abstract
High tibial osteotomy is a realignment procedure to transfer weight-bearing load to the intact compartment of the knee to alleviate symptoms, slow disease progression, and defer subsequent total knee arthroplasty. To prevent overcorrection or undercorrection, it is not only important to have an exact preoperative calculation of the desired correction angle, but it is also critical to have an accurate intraoperative technique. 85 consecutive patients (90 knees) were enrolled, who were available at 1-year follow-up after a medial opening wedge high tibial osteotomy using a kinematic navigation system or a conventional method, for medial unicompartmental osteoarthritis. On radiographic assessment, the navigation group showed better results than the conventional group in both the mechanical axis and the coordinate of the weight-bearing line on a full-length standing anteroposterior radiograph (3.9° ± 1.0° vs. 2.7° ± 2.2° of valgus, P < 0.01), (62.3 ± 2.9% vs. 58.7 ± 6.6% coordinate at the tibial plateau, P < 0.01). There was no significant difference in the alteration of tibial slope between the two groups. On clinical assessment, the navigation group showed better results in both the mean Hospital for Special Surgery knee score (84 ± 8 vs. 79 ± 7, P < 0.01) and the mean Lysholm knee score (85 ± 6 vs. 83 ± 5, P < 0.05). There was no significant difference in operation times between the two groups. Kinematic navigation-guided high tibial osteotomy is a reproducible and reliable procedure compared to conventional high tibial osteotomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-tibial osteotomy is a realignment procedure to transfer a weight-bearing load from an affected compartment to a relatively intact compartment of the knee. It promotes relief of symptoms, biologic healing of damaged cartilage, and slows down the disease progression in a varus knee [3].
To prevent overcorrection or undercorrection in high tibial osteotomy, the desired correction angle should be calculated exactly in preoperative planning. Even though there are several methods for calculating the correction angle such as the rule of thumb, the trigonometric principle and the weight-bearing line method, there might be errors associated with the surgeon’s experiences as well as radiographic magnifications [13].
Intraoperatively, the corrected angle can be checked by several methods that allow visualization of the mechanical axis such as the cable method, grids with lead-impregnated reference lines, and a radiological measurement of the joint orientation angles [12, 17, 19]. Even though these methods are useful, they have been implicated with several technical mistakes due to only momentary evaluation [5].
In orthopedic surgery, computer-assisted operations have gained popularity as they can improve intraoperative accuracy, precision and reproducibility. However, no clinical study to date has compared the results of conventional and navigation-guided high tibial osteotomies.
The purpose of this article is therefore to compare the results of navigated medial opening wedge high tibial osteotomy with those of conventional high tibial osteotomy, and to present the author’s surgical technique.
Materials and methods
Study population
A retrospective, comparative study of the results of the two different methods (navigated high-tibial osteotomy with allograft vs. conventional high tibial osteotomy with autograft) was approved by the Institutional review board. Between April 2004 and December 2007, 85 patients (90 consecutive knees) who were available at a 1-year follow-up after they underwent a medial open wedge high tibial osteotomy with the conventional method or the navigation system for medial unicompartmental osteoarthritis by a single surgeon, were enrolled. Before November 2005, 43 consecutive knees (40 patients) were assigned to have a conventional medial opening wedge high tibial osteotomy with autogenous tricortical iliac bone graft (conventional group). After November 2005, 47 consecutive knees (45 patients) were assigned to have a navigated medial opening wedge high tibial osteotomy with allogenous chip bone graft (navigation group) (Table 1).
Indications for surgery in both groups were the following: (1) medial unicompartmental osteoarthritis with varus deformity; (2) activity related pain on the medial side of the knee; (3) flexion arc of more than 100° with less than 15° of flexion contracture; (4) less than 12° of varus malalignment. Patients who had concomitant cruciate ligament injury, a history of fracture, or previous open surgery on the affected knee, were excluded from the present study.
Standing anteroposterior, lateral, 30° flexion posteroanterior and skyline views were taken for radiographic assessment. A full-length standing anteroposterior radiograph was also taken to determine the mechanical axis of the femur (from the center of the femoral head to the center of the tibial spines) and the tibia (from the center of the tibial spines to the center of the ankle) as well as the weight-bearing line.
In the conventional group, the expected correction angle was measured by drawing one line from the center of the hip to the 62% coordinate on the tibial plateau and a second line from the 62% coordinate on the tibial plateau to the center of the ankle joint (0% is consistent with the medial border of the tibia and 100% is consistent with the lateral border of the tibia). The angle formed by these two lines intersecting the 62% coordinate reflects the expected correction angle required to realign the weight-bearing line passing through this 62% coordinate [4, 18].
For clinical assessment, the Hospital for Special Surgery (HSS) knee score and the Lysholm knee scoring scale were employed preoperatively and postoperatively [8, 14].
All patients underwent simultaneous arthroscopic surgery to evaluate the status of the articular cartilage, and to treat the eburnated bone lesion with microfracture as well as the torn medial meniscus with an apposite meniscectomy. If the lateral meniscus tear required more than a partial meniscectomy, or more than grade I cartilage lesions on the basis of Outerbridge classification were revealed in the lateral or the patellofemoral compartment, high tibial osteotomy was not performed.
Surgical technique
In both the conventional group and the navigation group, the same technique for medial open wedge high tibial osteotomy was employed except that in the navigation group, the reference markers for determining the mechanical axis were used in the setting of the kinematic navigation system (Orthopilot, Aesculap, Tuttlingen, Germany), and instead of using an autogenous tricortial iliac bone graft, an allogenous chip bone graft was used to reduce overall operation time. Whereas in the conventional group, the cable method was used to determine whether the expected correction was achieved (Fig. 1), and the autogenous tricortical iliac bone graft was used to enhance union.
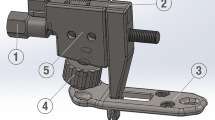
In the navigation group, the first reference marker was fixed at the distal femur, the second reference marker was fixed at the mid-tibia and the third reference marker was wrapped around the foot by a rubber strap (Fig. 2). By moving the hip, knee and ankle through the range of motion for each joint, the centers of the joints were determined, respectively, by the kinematic navigation system (Orthopilot, Aesculap, Tuttlingen, Germany). In addition to determining the centers of each joint using optoelectronic references, the mechanical axis was determined by palpating the patella, the medial and lateral epicondyle of the femur as well as the medial, lateral malleolus and the center of the ankle. This showed a preoperative mechanical axis of the affected lower extremity in degrees. The mechanical axis could be checked on the monitor in real time even after confirmation of the preoperative mechanical axis.
White arrows indicate a reference marker. a Each reference marker for the femur and tibia is secured firmly so that it does not move during the operation. b The third reference marker is for foot and attached with a rubber band. After confirmation of the mechanical axis, the third reference marker is detached
A longitudinal skin incision was made midway between the tibial tuberosity and the posteromedial crest of the tibia over the pes anserius, and was about 4–5 cm long. Along the superior border of the sartorius, the fascia was incised in line with its fiber. Then, the superficial medial collateral ligament and the underlying periosteum were reflected. The distal portion of the medial collateral ligament was raised with a periosteal elevator according to the amount of medial opening.
The starting point for the guide wire was on the medial side of the tibia, placed at the level of tibial tuberosity, approximately 3–4 cm distal to the medial joint line, thus the osteotomy was performed at the proximal part of the patellar tendon insertion. The first guide wire was inserted from medial to lateral direction and oriented obliquely toward the upper portion of fibular head, about 1.5 cm below the joint line under fluoroscopic guidance. At this time, the fluoroscope was tilted caudally about 10°, so the beam would be parallel to the posterior slope of the tibia, as for the tibial plateau view. After placing the first guide wire, the second guide wire was inserted parallel to the first guide wire. Fine tuning was performed till the two guide wires overlapped each other on the fluoroscopic image. At this point, the plane created by the two guide wires was parallel to the posterior slope of the tibia. To facilitate protection of the patellar tendon and to leave the tibial tuberosity at the distal part of the osteotomy site, we usually performed an incomplete oblique vertical osteotomy l cm behind the tibial tuberosity. Along the undersurface of the two guide wires, the oscillating saw was advanced to within 1 cm of the lateral cortex of the tibia under fluoroscopic guidance. The tapered wedge osteotome was inserted into the osteotomy site and the medial opening, hinging on the posterolateral cortex of the tibia, was slowly and carefully produced, until the expected mechanical axis was achieved. The process was monitored on the navigation system in real time.
In the conventional group, the advance of the tapered wedge osteotome as well as the intersection of the cable from the center of the hip to the center of the ankle joint through just lateral to the lateral tibial spine (the 62% coordinate on the tibial plateau) were monitored under the fluoroscope.
The opening at the anteromedial corner of the tibia was about half of that at the posteromedial corner to recreate the inherent posterior slope of the tibia in both groups [15]. As typically accepted, the desired mechanical axis was 3°–5° of valgus [1, 6, 13]. During opening of the osteotomy site, careful attention was paid so as not to break the lateral cortex until the desired alignment was achieved. Once the desired alignment was achieved and confirmed on the navigation system (Fig. 3), the osteotomy site was secured with the appropriate dual open wedge plates (Fig. 4) (Aesculap, Seoul, Korea) after measuring the gap in the navigation group. To replicate the inherent posterior slope of the tibia, the posterior plate was used as measured, and a 2 mm smaller plate was used as the anterior plate in the navigation group. In the navigation group, we put the allogenous bone chips into the osteotomy site after securing the plates with four 6.5 mm cancellous screws.
In the conventional group, two autogenous tricortical iliac bone grafts were trimmed into a wedge shape to insert into both the anterior and posterior portion of the tibia. One was trimmed as measured and inserted into the posterior aspect of the tibia, and the other one was trimmed 2–3 mm lower in height and inserted into the anterior aspect of the tibia to prevent an undesired alteration of the tibial slope. After the insertion of the bone graft, a modified Puddu plate (Fig. 5) (Taesan Sol., Seoul, Korea) was placed on the anteromedial side of the tibia. The plate was secured with three 6.5 mm cancellous screws for the proximal portion and three 4.5 mm cortical screws for the distal portion. Then, it was examined to determine whether the knee extension obtained was comparable to that before surgery. Postoperatively, after splint immobilization for 4 weeks, exercises for range of motion were started with the knee protected by a hinged knee brace for an additional 2 weeks and only toe touch weight-bearing allowed for the first 4 weeks in both groups. After 4 weeks, progressive tolerable weight-bearing was encouraged.
Statistical method
Student’s t-tests were implemented using SPSS software (v.12.0, Chicago, IL, USA) to compare the clinical and radiological results in the navigation and conventional groups with the assumption of homogeneity of variance by Levene’ test as appropriate. A P value < 0.05 was considered statistically significant.
Results
Radiographic results
The preoperative mechanical axis assessed on a full-length standing anteroposterior radiograph was 5.3° ± 1.9° of varus (range from 2.0° to 10.3° of varus) in the conventional group, and 4.7° ± 2.2° of varus (range from 2.2° to 11.3° of varus) in the navigation group (Table 1). The preoperative mechanical axis in the navigation group taken by kinematic navigation and displayed on the monitor was 4.7° ± 2.0° of varus (range from 2° to 10° of varus). At the 1-year postoperative follow-up, the mechanical axis on a full-length standing anteroposterior radiograph was 2.7° ± 2.2° of valgus (range from 0.7° to 8.2° of valgus) in the conventional group, and 3.9° ± 1.0° of valgus (range from 1.8° to 7.3° of valgus) in the navigation group, and this difference was statistically significant (P < 0.01) (Table 2). The weight-bearing line passed through the 58.7 ± 6.6% (50–75%) coordinate at the tibial plateau (0% is consistent with the medial border of tibia and 100% with the lateral border of tibia) in the conventional group, and 62.3 ± 2.9% (56–70%) coordinate in the navigation group, and there was a significant difference (P < 0.01) (Table 2). The preoperative posterior tibial slope (the angle between the medial tibial plateau and posterior tibial cortex) on the lateral radiograph was 10.2° ± 2.3° (range from 6.3° to 15.1°) in the conventional group, and 9.5° ± 2.3° (range from 5.6° to 14.6°) in the navigation group (Table 1). At the 1-year postoperative follow-up, the posterior tibial slope was 10.8° ± 2.2° (range from 7.5° to 16.4°) in the conventional group, and 10.0° ± 2.3° (range from 7.4° to 15.8°) in the navigation group, and there was no significant difference (P > 0.05) (Table 2).
Clinical results
All included knees in both groups had a medial meniscus tear and they underwent apposite meniscectomy according to their tear patterns. Four knees in the navigation group had concomitant lateral meniscus tear and underwent partial meniscectomy and five knees in the conventional group had a partial lateral meniscectomy. All knees showed grade III or IV cartilage lesions on the medial compartment of the femoral and/or the tibial condyle. The Hospital for Special Surgery (HSS) knee score improved from 57 ± 5 (from 49 to 67) to 79 ± 7 (59 to 92) in the conventional group, and from 58 ± 5 (46 to 67) to 84 ± 8 in the navigation group (63 to 95) at their 1-year follow-ups. There was a statistically significant difference in the HSS knee score at the 1-year follow-up between the two groups (P < 0.01) (Tables 1, 2) The Lysholm knee scoring scale improved from 55 ± 5 (from 45 to 68) to 83 ± 5 (74 to 92) in the conventional group, and from 56 ± 6 (45 to 68) to 85 ± 6 (73 to 92) in the navigation group at the 1-year postoperative follow-up. There was a statistically significant difference between the two groups in the Lysholm knee score at the 1-year follow-up (P < 0.05) (Tables 1, 2). The operation time was not significantly different between the two groups (P > 0.05): 73.8 ± 8.5 min in the conventional group and 74.8 ± 6.9 min the navigation group.
Complications
There were two cases with complications in the conventional group, which were delayed union. In the navigation group, there were three cases with complications: two of delayed union, and one of varus collapse. All of these complications were associated with the breakage of the lateral tibial cortex at the osteotomy site during medial opening. In the cases where there was no evidence of callus at the osteotomy site more than 4 weeks postoperatively, we prolonged the postoperative immobilization to 6 weeks and applied a hinged knee brace for another 6 weeks. While four cases of delayed union showed a bony union after 6 months postoperatively without any additional surgical intervention, one case showed a collapse with varus deformity that required a reoperation (varus 7.2°). With the correction of varus deformity, the osteotomy site was fixed securely with dual open wedge plates again and an autoiliac bone block, in addition to allogenous chip bone, was inserted to enhance union.
Discussion
Since Jackson introduced high tibial osteotomy in 1958 [9], it has become one of the best-established surgical options for unicompartmental osteoarthritis with a varus deformity in young and middle-aged patients. The medial opening wedge osteotomy reported by Hernigou et al. [6] has recently gained popularity as it has several advantages over the traditional lateral closing wedge osteotomy. However, in both lateral closing wedge and medial opening wedge osteotomies, undercorrection or overcorrection is a leading cause of failed high tibial osteotomies [6, 16, 21]; this under- or overcorrection results from difficulties in precisely correcting the malalignment intraoperatively.
Recently, computer-assisted surgery system has significantly advanced in orthopedic surgery. It can address inadvertent intraoperative technical errors in conventional surgery and improve reproducibility. In high tibial osteotomies, the computer-assisted surgery system was introduced to compensate for variations in surgeon’s experiences with regard to preoperative planning and intraoperative correction.
In the conventional method, the desired mechanical axis is achieved under a fluoroscope, which is confirmed by the cable method or alignment rod intraoperatively [12]. Several inadvertent errors can be introduced when calculating the desired correction angle preoperatively, as well as when confirming the corrected mechanical axis intraoperatively [10].
In the current study, the desired mechanical axis in the conventional group was determined as the weight-bearing line passed through the 62% coordinate at the tibial plateau, just lateral to the lateral tibial spine, and in the navigation group, the desired mechanical axis was 3°–5° of valgus, as a slight overcorrection that is widely accepted [1, 6, 13]. At the 1-year postoperative follow-up, the navigation group showed better results in the acquired mechanical axis (2.7° ± 2.2° vs. 3.9° ± 1.0°) as well as in the placement of the weight-bearing line at the tibial plateau (58.7 ± 6.6% vs. 62.3 ± 2.9%). In terms of reproducibility, the navigation group produced results with less standard deviation than the conventional group. Saragaglia et al. [11] compared the postoperative mechanical axis between a navigated osteotomy group and a conventional osteotomy group, and found that the navigated osteotomy group showed better reproducibility than the conventional group in achieving a desired mechanical axis. Hankemeier et al. [5] reported a similar result in their study comparing a fluoroscope-based navigation system group and a conventional group, based on measurement of the mechanical axis intersecting the tibial plateau.
With regard to the clinical results of the two groups, even though the present study reflected a 1-year follow-up, the navigation group showed significantly better results in the HSS knee score and the Lysholm knee score. Given the fact that undercorrection or overcorrection has been associated with failed high tibial osteotomies, a precise correction of the mechanical axis is imperative to achieve a satisfactory clinical result [6, 16, 21]. However, a long-term follow-up on navigated high tibial osteotomies is needed, because satisfactory radiographic results do not necessarily equate to satisfactory long-term clinical results.
There was no significant difference in operation time between the two groups. In the navigation group, it took time to determine the center of the hip, knee, and ankle on the kinematic navigation system at the beginning of surgery; however, this was compensated for by using an allogenous chip bone graft, which did not need to harvest and trim into a desired shape as an autogenous tricortical iliac bone graft did. In the conventional group, it took time to obtain a fluoroscopic image to ensure that the cable spanned precisely from the center of the hip to the center of the ankle as well as passing at the 62% coordinate on the tibial plateau.
There was no significant difference in the groups regarding alteration of the posterior tibial slope after surgery. A limitation of the kinematic navigation system used in the current study is the inability to control sagittal plane correction, or the posterior slope of the tibia. To enable the osteotomy to parallel the inherent slope of the tibia in the sagittal plane, we inserted two guide pins to overlap each other on a 10° caudally tilted fluoroscope to simulate the tibial plateau view in both groups. When adjusting the opening wedge, the opening at the posteromedial corner of the tibia should be about two times that at the anteromedial corner to recreate an inherent posterior slope of the tibia, because symmetrical opening would entail an unexpected increase in the posterior slope of the tibia [15]. In the navigation group, the two different sized plates (the anterior plate was usually 2 mm smaller than the posterior plate) were applied to replicate the original slope with the allogenous chip bone graft. In the conventional group, we put two wedge-shaped autogenous tricortical iliac grafts, different in height, into the osteotomy site to replicate an inherent posterior tibial slope with one modified Puddu plate.
In medial opening high tibial osteotomy, an autoiliac bone block is widely used to enhance bone union; however, some authors use bone substitute materials for filling the medial opening gap. Koshino et al. [2] documented good results without any complications for unions of their 21 knees using a porous hydroxyapatite wedge in conjunction with autofibular grafts. Hernigou and Ma used a block of acrylic bone cement and reported a low incidence (1%) of problems with the unions [20].
We used allogenous bone chips instead of the autoiliac bone block in the navigation group not only to avoid donor site morbidity, which has been reported by other authors [7, 20, 22], but also to reduce operational time. There were two cases (4.2% of 47 cases) of delayed union and one case (2.1% of 47 cases) of a varus collapse in the navigation group, and two cases of delayed union (4.6% of 43 cases) in the conventional group. All five of these cases were associated with lateral cortex breakage during the medial opening. While the navigation group had a relatively high incidence (6.3%) of complications related to union including one case of a varus collapse, we are not sure whether this resulted from instability caused by the lateral cortex breakage, or from the biomechanical inferiority of the allogenous chip bone graft. In both groups, rehabilitation protocols such as degree and starting time of weight-bearing and ROM exercise were same.
One limitation of the present study is a relatively short-term follow-up. After the 1-year follow-up, there can be a progressive loss of correction which will undoubtedly have a detrimental effect on clinical results. Thus, a long-term follow-up is necessary to evaluate the benefits of using a kinematic navigation system in high tibial osteotomies. Another limitation of the present study is the fact that we used different types of plates in each of the groups. A modified Puddu plate (Taesan Sol., Seoul, Korea) was employed in the conventional group and dual open wedge plates (Aesculap, Seoul, Korea) were employed in the navigation group. Differences in the biomechanical properties of the plates may have influenced the results as well as complications rates.
Conclusion
The current study showed better clinical and radiological results for navigation-guided high tibial osteotomy when compared with conventional osteotomy. In terms of operation time, there was no significant difference between two groups as the use of allogenic bone graft reduced the operation time in the navigation group. It was shown that navigation-guided high tibial osteotomy is a reproducible and reliable procedure.
References
Amendola A (2003) Unicompartmental osteoarthritis in the active patient: the role of high tibial osteotomy. Arthroscopy 19(Suppl 1):109–116
Brouwer RW, Bierma-zeinstra SMA, van Raaij TM, Verhaar JAN (2006) Osteotomy for medial compartment arthritis of the knee using a closing wedge or an opening wedge controlled by a Puddu plate. A one-year randomized, controlled study. J Bone Joint Surg Br 88:1454–1459
Dowd GSE, Somayaji HS, Uthukuri M (2006) High tibial osteotomy for medial compartment osteoarthritis. Knee 13:87–92
Dugdale TW, Noyes FR, Styer D (1992) Preoperative planning for high tibial osteotomy: the effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res 274:248–264
Hankemeier S, Hufner T, Wang G, Kendoff D, Zeichen J, Zheng G, Krettek C (2006) Navigated open-wedge high tibial osteotomy: advantages and disadvantages compared to the conventional technique in a cadaver study. Knee Surg Sports Traumatol Arthrosc 14:917–921
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity A ten to thirteen-year follow-up study. J Bone Joint Surg Am 69:332–354
Hernigou P, Ma W (2001) Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee 8:103–110
Insall JN, Ranawat CS, Aglietti PA, Shine J (1976) A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am 58:754–765
Jackson JP (1958) Osteotomy for osteoarthritis of the knee: proceedings of the Sheffield Regional Orthopaedic Club. J Bone Joint Surg Br 40:826
Kawakami H, Sugano N, Yonenobu K, Yoshikawa H, Ochi T, Hattori A, Suzuki N (2004) Effects of rotation on measurement of lower limb alignment for knee osteotomy. J Orthop Res 22:1248–1253
Koshino T, Murase T, Saito T (2003) Medial opening-wedge high tibial osteotomy with use of porous hydroxyapatite to treat medial compartment osteoarthritis of the knee. J Bone Joint Surg Am 85:78–85
Krettek Ch, Miclau T, Grun O, Schandelmaier P, Tscherne H (1998) Intraoperative control of axes rotation and length in femoral and tibial fractures Technical note. Injury 29(Suppl 3):29–39
Leone JM, Hassen AD (2006) Osteotomy in the sports knee. In: Insall JN, Scott WN. Surgery of the knee, 4th edn. Churchill Livingstone, New York, pp 1752–1753
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10:150–154
Noyes FR, Goebel SX, West J (2005) Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med 33:378–387
Paley D, Herzenberg JE, Tetsworth K (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 25:425–465
Paley D, Tetsworth K (1992) Mechanical axis deviation of the lower limbs Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res 280:48–64
Rudan JF, Simurda MA (1990) High tibial osteotomy: a prospective clinical and roentgenographic review. Clin Orthop Relat Res 255:251–256
Saleh M, Harriman P, Edwards DJ (1991) A radiological method for producing precise limb alignment. J Bone Joint Surg Br 73:515–516
Saragaglia D, Roberts J (2005) Navigated osteotomies around the knee in 170 patients with osteoarthritis secondary to genu varum. Orthopedics 28(10 Suppl):1269–1274
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis Survival and failure analysis to twenty-two years. J Bone Joint Surg Am 85:469–474
Staubli AE, Simoni CD, Babst R, Lobenhoffer P (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia–early results in 92 cases. Injury 34(Suppl 2):55–62
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, SJ., Koh, YG., Chun, YM. et al. Medial opening wedge high-tibial osteotomy using a kinematic navigation system versus a conventional method: a 1-year retrospective, comparative study. Knee Surg Sports Traumatol Arthrosc 17, 128–134 (2009). https://doi.org/10.1007/s00167-008-0630-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-008-0630-y