Abstract
During decennia the treatment of radial head fractures has been controversial. For Mason type II fractures, more recent studies agree that open reduction and internal fixation is the treatment of choice. It restores biomechanical properties, allows an early mobilisation of motion and results in better functional outcome compared with other treatments. In this study, we present the mid-to-long-term results of an arthroscopic technique for reduction and percutaneous fixation. Fourteen patients were available for follow-up with a final assessment performed at an average of 5 years 6 months (range 1 year to 11 years 3 months). Patients were evaluated for pain, motion and radiological findings. The average elbow score (Broberg and Morrey in J Bone Joint Surg Am 68:669–674, 1986) was 97.6 points (range 86–100), corresponding with 3 good and 11 excellent results. Two of the patients with only good results had associated cartilage lesions of the capitellum. Our results show that arthroscopically assisted reduction and internal fixation of type II radial head fractures is a valid technique with consistently good outcome. Although the technique is technically demanding, it allows more precise articular fracture reduction control, as well as better evaluation of associated lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of radial head fractures is still controversial. Options include non-surgical management, open reduction with internal fixation, radial head excision and prosthetic replacement. For the Mason type II fractures, more recent studies agree that open reduction and internal stable fixation is the treatment of choice [11, 13, 14, 24–26, 29]. It restores the biomechanical properties, allows range of motion exercises and results in better functional outcome compared with other treatments.
In this study, we present an arthroscopic technique for reduction and percutaneous fixation. The purpose of this study is to evaluate the long-term results of 14 patients treated with an arthroscopic technique for reduction and percutaneous fixation.
Materials and methods
Sixteen patients with a Mason type-II radial head fracture were managed by arthroscopic reduction and percutaneous fixation between 1992 and 2005. Of the 16 patients treated, 2 were lost to follow-up. Fourteen patients were reviewed and a final assessment was performed.
Study population
Follow-up averaged 5 years 6 months (range from 1 year to 11 years 3 months). The mean age at time of operation was 37.5 years (range from 19 to 57 years) (Table 1). Our patients contained five men and nine women. Eight injuries were the result of a fall from standing height; one, a fall from a greater height; two, a fall during sports activity; two, a bicycle accident and one a motorcycle accident. In nine patients, the dominant arm was affected.
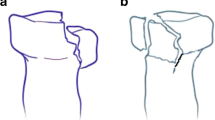
The fracture type was classified according to the Mason classification, as modified by Hotchkiss [11] (Table 2). Only type II fractures were included in this study (Fig. 1). If there was any doubt about the fracture type or displacement, a CT-scan was performed (Fig. 2). In this retrospective study, all patients had at least 2 mm fragment displacement. All fractures were closed without neurovascular injuries. Two patients had a cartilage lesion of the capitellum. No elbow dislocation or other associated lesions were present.
Arthroscopic treatment
Elbow arthroscopy was performed using a standardized technique. The patient is placed in prone position under general anesthesia. The arm is hung over a padded arm board with the elbow flexed at 90° and the forearm hanging free.
The elbow is initially insufflated with a saline solution through the soft spot. The first midlateral portal is used for viewing. An anterolateral portal is used for instrumentation (Fig. 3). The hemarthrosis and debris are washed out. The joint is inspected and associated lesions are searched for.
Pronation and supination allow a more extended view of the radial head and fracture fragments.
After assessment of the fracture pattern, reduction is performed by manipulation with a probe and a K-wire (Fig. 4). This percutaneously placed K-wire is also used to maintain fracture reduction.
Through a small stab incision, a headless screw with a differential thread is inserted. Throughout the study period, two different brands of headless screws were used: non-cannulated herbert screws for 12 patients and cannulated bold screws for the other four patients. In case of a cannulated screw, the K-wire used for temporary fracture fixation is overdrilled and the screw is inserted over the K-wire. After fixation the reduction is evaluated with a probe. In case of a large free fracture fragment and the impression of fragment instability after insertion of the first screw, a second screw is placed according to the same technique. In case of doubt, the screw length was verified with the image intensifier. Postoperatively patients received a sling and early range of motion exercises while full rotation is promoted.
In the two patients with a cartilage lesion of the capitellum, the lesion was debrided and loose cartilage fragments were removed.
Evaluation
The final clinical and radiographic evaluation was done by the junior author (FM). All the patients had at least 1 year follow-up. In the follow-up assessment, the Elbow evaluation score described by Broberg and Morrey [2] (Table 3) and the American shoulder and elbow surgeons elbow assessment (ASES) form were used. These include pain, motion, strength, stability, satisfaction and function as outcome variables.
Radiographic signs of osteoarthritis were assessed according to the criteria of Broberg and Morrey [2].
Results
Pain
Twelve of the 14 patients had no elbow pain or only an occasional ache with heavy use.
Visual-analogue-scale scores in the ASES form were used to compare the patients’ perception of pain, with 25 points representing the best possible score. The average score was 23.8 points (range 20.5–25 points). Table 4 lists the level of difficulty in performing various activities.
Motion
Average flexion was 142.2° (range 122–150), and the mean flexion deformity was 2.8° (range 0°–10°). The range of pronation and supination was symmetrical.
No patients had clinical evidence of instability.
Strength
All patients demonstrated normal power of elbow flexion, extension, pronation and supination. In all cases the grip strength of the affected arm was within 10% of the grip strength of the unaffected arm.
Satisfaction
Satisfaction was assessed using the 10-point ordinal scale in the ASES score, anchored at 0 for low and 10 for high satisfaction. Patients were generally satisfied with scores ranging from 8 to 10 points (mean 9.5).
Radiographic assessment
Radiographic evaluation confirmed good reduction and fracture healing (Fig. 5). Traumatic degenerative changes were absent in 11 elbows, mild in two and moderate in one. No elbow showed severe degenerative changes.
Functional Assessment
The Broberg and Morrey functional rating score averaged 97.6 points (range 86–100), corresponding with 3 good and 11 excellent results. Two patients with only good results had associated cartilage lesions of the capitellum.
All patients returned to preoperative professional and sports activities such as high-level basketball (1), tennis (3), volleyball (1) and rock climbing (2). Another patient changed his job to one with heavier manual work.
Complications
None of the patients required a second operation. No hardware needed to be removed.
No infections, nerve injuries or vascular injuries have developed after arthroscopy in this series.
Discussion
Treatment of Mason type II fractures is still controversial. Options include non-surgical management, excision and open reduction and internal fixation. This study evaluates the long-term results of an arthroscopic technique in the treatment of those fractures.
At present, open reduction and internal fixation has become the most accepted treatment for those fractures, as it restores the biomechanical properties and offers a better functional outcome [1, 11, 13, 14, 24–26, 29].
The reports of radial head excision are controversial, with some authors judging it to be satisfactory [5, 8, 21] and others reporting an unfavourable outcome [12, 18, 19, 27]. In other studies no difference was found between primary or delayed radial head excision [2, 10]. Probably, radial head excision should be reserved as a primary procedure in patients with low demand or as a salvage procedure when symptoms persist. We suggest that radial head excision only should be used in low demand patients with an inadequate range of motion, or in patients with persisting residual symptoms after initial treatment.
The technique of arthroscopically assisted reduction and percutaneous fixation is an alternative for open reconstruction of the radial head. After an initial feasibility series in the early 1990, the senior author decided to reserve the arthroscopic approach for Mason type II fractures in a younger active population. This obviously limited the number of included patients. In our department, a very conservative attitude was adopted towards other fracture types as well as in elderly patients. In addition, only a few patients (less than 10) underwent ORIF or arthroplasty with radial head prosthesis during the same time interval. Unfortunately, it is impossible to retrospectively determine the exact number of patients with radial head fractures cared for at our hospital in the given period as no database for conservatively managed fractures exists.
The good and excellent results in this study are very similar to other studies that used open reduction and internal fixation as treatment for Mason type II fractures. Ring et al. [24] published an average score of 92 points using the same score. They also found a significant association between an unsatisfactory result and a complex injury pattern. Esser et al. [7] reported similar results. Khalfayan et al. [14] concluded that displaced radial head fractures treated conservatively had more pain and loss of strength and were less mobile than fractures treated by a stable osteosynthesis.
The technique of arthroscopically assisted reduction and internal fixation has been described once before. Rolla et al. report six patients treated with a similar technique. The fractures were not further classified, the follow-up was limited to an average of 12 months and they reported a satisfactory functional outcome [25]. Treatment of a radial neck fracture by arthroscopic reduction and percutaneous fixation has been described [6].
Open reduction can be performed by plate and screws or by merely using screws. Several studies report good results with the use of Herbert screws [3, 16, 23, 24]. Such a headless screw can be buried beneath the articular surface of the radial head which avoids impingement. Due to the differential thread, the screw causes compression across the fracture. In our more recently treated patients, we were able to use a cannulated type of headless screw, which obviously made the technique much easier. Since the stability was controlled per-operatively using fluoroscopy as well as arthroscopy, a second screw was deemed necessary in only few cases. It is our feeling that the minimal invasive approach maintains the capsular structures, which may have an additional stabilizing effect. This may limit the need for an additional screw, while the capsular dissection required in an open technique may sufficiently add to fracture fragment instability requiring the placement of an additional screw.
If the fracture fixation with one screw during open surgery would appear as stable, we would not tend to add a second screw either. However, in the study period, no type II fractures were primarily treated by open surgery. In three patients, arthroscopic surgery had to be converted to open surgery because the screw could not be inserted percutaneously. In two patients, fracture fixation was not possible because the fragments appeared too small during arthroscopic evaluation. In these cases, the fragments were reduced with a probe but not fixed. Finally, an arthroscopic reduction of a die punch fragment in the radial head was done in two patients, again without fragment fixation because the reduction was already stable without a screw. All these patients were excluded from the presented series.
In this study, we used the Mason classification, as modified by Hotchkiss [11]. Mason’s original classification was only based on radiological findings, the degree of displacement is not determined and associated lesions are not considered [1, 15, 30]. The classification developed by Hotchkiss is based on radiological appearance, features of the clinical examination and an assessment of associated lesions, which makes it more practical and treatment directed [29]. Hotchkiss also recommended a CT scan for additional information on the size and displacement of the fracture fragments [11]. A minimally displaced fracture (displacement less than 2 mm) without mechanical block requires no operative treatment. If the displacement is less than 2 mm, it is classified by Hotchkiss as a type I fracture. A repairable fracture (not severely comminuted or three-part) is classified as a type II fracture. A not reconstructable fracture (severely comminuted) is classified as a type III fracture. In this study only type II fractures were included. We do not recommend managing severely comminuted fractures by arthroscopically assisted reduction and internal fixation.
The possibility of assessing and treating intra-articular pathology arthroscopically offers significant advantages over open procedures [17].
The most important advantage of arthroscopy is that it offers a good view of the articular surface, which leads to a better understanding of the morphology of the fracture lines and fragments. This facilitates a more precise fracture reduction control [6, 25].
Another important advantage is a better evaluation of associated lesions compared with other techniques [6, 9, 25]. Resection of loose bodies or osteophytes and debridement of cartilage lesions is also possible. Little additional tissue damage with early mobilisation as well as the removal of haemarthrosis and articular debris decrease the risk of adherences and create the circumstances that allow a better functional outcome [9, 25]. A better cosmetic result is another benefit.
In this study we had no complications as neurovascular damage or infection.
Treatment of radial head fractures may be complicated because of the presence of associated lesions. Recently, capitellum lesions were noted by van Riet et al. [30] in 2% of patients for a total of 39% of associated lesions. The less good results in the patients with lesions of the capitellum can be explained by the disturbance of the radiocapitellar contact surface. This part of the joint is extremely important, as 60% of the axial load at the elbow is transmitted through the radiocapitellar joint [20].
There are few reports of combined capitellum and radial head fractures. Ward and Nunley [31] report a series of seven concomitant fractures of the capitellum and radial head. They found an incidence of 1% capitellum fractures in all radial head fractures. This incidence even reached 24% in radial head fractures that required surgical treatment. They recommend an open anatomic reduction and secure fixation of large displaced fractures and excision of small fracture fragments. They also stress the importance of a complete removal of loose intraarticular fragments. In the present study, we found an incidence of 14% capitellar cartilage lesions (only type II fractures were included), they were associated with a less good outcome.
Hardy et al. [9] report a screw fixation of type I capitellum fracture under arthroscopic control. Caputo et al. [4] report ten cases of articular cartilage injuries of the capitellum interposed in radial head fractures. This injury pattern was identified in no case on preoperative imaging, including computed tomography in two cases.
Neurovascular damage is the most feared complication of elbow arthroscopy. The radial and posterior interosseous nerves are at risk of being damaged by any surgical procedure on the anterolateral and inferior capsule of the elbow. Therefore, careful attention to the regional anatomy and technical considerations of elbow arthroscopy is essential to prevent direct injury to the neurovascular structures of the elbow [22, 28].
We used midlateral as a viewing portal and an anterolateral portal as a working portal. This allows a good view of the radial head, the capitellum and the radioulnar joint [28]. Rolla et al. [25] used four portals, the proximal anteromedial portal and posterolateral portal for viewing and the anterolateral and midlateral portal for instrumentation.
We must emphasize that arthroscopic radial fracture reduction and fixation is a technically demanding procedure and requires the skill of an experienced arthroscopist.
In conclusion, our results show that arthroscopically assisted reduction and internal fixation of type II radial head fractures is a valid option with consistently good outcome. Although this less invasive technique is technically demanding, it allows more precise articular fracture reduction control, as well as better evaluation of associated lesions.
Associated cartilage lesions of the capitellum were associated with a less good outcome.
References
Bennett J (1993) Radial head fractures: diagnosis and management. J Shoulder Elbow Surg 2:264–273
Broberg M, Morrey B (1986) Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am 68:669–674
Bunker T, Newman J (1985) The Herbert differential pitch bone screw in displaced radial head fractures. Injury 16:621–624
Caputo A, Burton K, Cohen M, King J (2006) Articular cartilage injuries of the capitellum interposed in radial head fractures: a report of ten cases. J Shoulder Elbow Surg 15:716–720
Coleman D, Blair W, Shurr (1987) Resection of the radial head for fracture of the radial head.Long term follow-up of seventeen cases. J Bone Joint Surg Am 69:385–392
Dawson F, Inostroza F (2004) Arthroscopic reduction and percutaneous fixation of a radial neck fracture in a child. Arthroscopy 20:90–93
Esser RD, Davis S, Taavao T (1995) Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma 9:318–323
Goldberg I, Pelan J, Yosiovitch Z (1986) Late results of excision of the radial head for an isolated closed fracture. J Bone Joint Surg Am 68:675–679
Hardy P, Menguy F, Guillot S (2002) Arthroscopic treatment of capitellum fracture of the humerus. Arthroscopy 18:422–426
Herbertsson P, Josefsson P, Hasserius R, Besjakov J, Nyqvist F, Karlsson (2004) Fractures of the radial head treated with radial head excision. J Bone Joint Surg Am 86:1925–1930
Hotchkiss R (1997) Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg 5:1–10
Ikeda M, Oka Y (2000) Function after early head resection for fracture: a retrospective evaluation of 15 patients followed 3–18 years. Acta Orthop Scand 71:191–194
Ikeda M, Sugyama K, Kang C, Takagaki T, Oka Y (2005) Comminuted fractures of the radial head Comparison of resection and internal fixation. J Bone Joint Surg Am 87:76–84
Khalfayan E, Culp R, Alexander A (1992) Mason type II radial head fractures: operative versus nonoperative treatment. J Orthopaedic Trauma 6:283–289
Mason M (1954) Some observations on fractures of he head of the radius with a review of one hundred cases. Br J Surg 42:123–132
McArthur R (1987) Herbert screw fixation of fracture of the head of the radius. Clin Orth 224:79–87
Menth-Chiari W, Poehling G, Ruch D (1999) Arthroscopic resection of the radial head. Arthroscopy 15:226–230
Mikic Z, Vukadinovic S (1983) Late results in fractures of the radial head treated by excision. Clin Orthop 181:220–228
Morrey B (1995) Current concepts in the treatment of fractures of the radial head, the olecranon, and coronoid. J Bone Joint Surg Am 77:316–327
Morrey B, An K, Stormont T (1988) Force transmission through the radial head. J Bone Joint Surg Am 70:250–256
Morrey B, Chao E, Hui F (1979) Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am 61:63–68
O’Driscoll S, Morrey B (1992) Arthroscopy of the elbow. J Bone Joint Surg Am 74:84–94
Pearce M, Gallannaugh S (1996) Mason type II radial head fractures fixed with Herbert bone screws. J R Soc Med 89:340–344
Ring D, Quintero J, Jupiter J (2002) Open reduction and internal fixation of fractures of the Radial Head. J Bone Joint Surg Am 84:1811–1815
Rolla P, Surace M, Bini A, Pilato G (2006) Arthroscopic treatment of fractures of the radial head. Arthroscopy 22:233e1–233e6
Sanders R, French H (1986) Open reduction and internal fixation of comminuted radial head fractures. Am J Sports Med 14:130–135
Sowa D, Hotchkiss R, Weiland A (1995) Symptomatic proximal translation of the radius following radial head resection. Clin Orthop 317:106–113
Stothers K, Day B, Regan W (1995) Arthroscopy of the elbow: anatomy, portal sites and a description of the lateral portal. Arthroscopy 4:449–457
Van Glabbeek F, van Riet R, Verstreken J (2001) Current concepts in the treatment of radial head fractures in the adult: a clinical and biomechanical approach. Acta Orthop Belg 67:430–441
van Riet R, Morrey B, O’Driscoll S, Van Glabbeek F (2005) Associated injuries complicating radial head fractures. Clin Orthop 441:351–355
Ward WG, Nunley JA (1988) Concomitant fractures of the capitellum and radial head. J Orthop Trauma 2:110–116
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Michels, F., Pouliart, N. & Handelberg, F. Arthroscopic management of Mason type 2 radial head fractures. Knee Surg Sports Traumatol Arthr 15, 1244–1250 (2007). https://doi.org/10.1007/s00167-007-0378-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0378-9