Abstract
Press-fit fixation of patellar tendon bone anterior cruciate ligament autografts is an interesting technique because no hardware is necessary to achieve fixation. Up till the present point, there is no biomechanical data available for the tibial press-fit fixation of the hamstring tendons. Hamstring tendons of 21 human cadavers (age: 41.9 ± 13.1 years) were used. A press-fit fixation with looped semitendinosus and gracilis tendons secured by a tape (T) over a bone bridge, or by a baseball-stitched suture (S), was compared with degradable interference screw fixation (I) in 21 porcine tibiae. The constructs were cyclically strained and subsequently loaded to failure. The maximum load to failure, stiffness, and elongation during cyclical loading were measured. The maximum load to failure was highest for the T-fixation at 970 ± 83 N, followed by the I-fixation with 544 ± 109 N, and the S-fixation with 402 ± 78 N (P < 0.03). Stiffness of the constructs averaged 78 ± 13 N/mm for T, 108 ± 18 N/mm for S, and 162 ± 27 N/mm for I (P < 0.03). Elongation during initial cyclical loading was 2.0 ± 0.6 mm for T, 3.3 ± 1.1 mm for S, and 1.4 ± 0.5 mm for I (S inferior to I and T, P<0.05). Elongation between the 20th and 1,500th loading cycle was lower for T (2.2 ± 0.7 mm) compared with I (4.1 ± 2.7 mm) and S (4.8 ± 0.7 mm; P < 0.001). The T-fixation technique exhibited a significantly higher failure load than the S-, and I- techniques. All techniques exhibited larger elongation during initial cyclical loading than is reported in the literature for grafts with bone blocks. Only one technique (T) showed satisfactory elongation behavior during long-term cyclic loading. Interference screw fixation demonstrated significantly higher stiffness. Only one of the investigated techniques (T) seemed to exhibit adequate mechanical properties necessary for early aggressive rehabilitation programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hamstring tendons and bone patellar tendon bone (BPTB) have both been named the “gold standard” for primary anterior cruciate ligament (ACL) replacement [7]. Nonetheless, many different fixation techniques have been investigated [16, 17, 19]. For the hamstring tendons, most surgeons today use hardware for fixation of the graft outside (Endobutton, suture, postscrew, staple) or inside (nonresorbable and resorbable interference screws, cross-pin) the drill holes [25]. The use of most of these implants is compromised by artifacts on postoperative magnetic resonance imaging and the necessity of implant removal in the case of ACL revision surgery [15, 22]. Hardware free press-fit fixation may provide a solution to the drawbacks associated with current techniques [25].
Bone tunnel enlargement is a problem that has been observed following reconstruction of the ACL [4, 14]. The occurrence of bone tunnel enlargement is more frequent, and the magnitude is greater when hamstring grafts are used [28]. Migration of the graft within the tunnel has been suspected of causing this phenomenon [10]. In several meta-analyses, it was demonstrated that hamstring tendon reconstructions are associated with less patellar pain, but the stability of contemporary hamstring tendon reconstructions is inferior to the BPTB technique [5, 6, 32]. Press-fit fixation of the patellar tendon with bone blocks has been shown to provide a good functional outcome in a study with a follow-up of 10 years [8]. In a previous study from our lab, three techniques of press-fitting hamstring tendons in the femoral tunnel were investigated [13]. Two of the three techniques were shown to be mechanically equivalent with the patellar tendon press-fit technique if preconditioned adequately.
We therefore conducted the present study in order to investigate the possibility of using press-fit fixation on the opposite end of the graft, namely in the tibial tunnel. The investigated techniques were also developed using a bone block that presses the graft against the tibial tunnel in close proximity to the joint space. Based on previous experiences, such a technique could foster graft to bone healing [29]. Bone graft integration has been compromised by many of today’s implants [3, 14].
Hence, the purpose of this study was to develop and mechanically characterize a tibial press-fit technique of the hamstring tendons that is free of artificial implants and utilizes a bone block. The fixation strength of this procedure was thus compared with that of a biodegradable interference screw fixation that was well documented [17, 31].
Materials and methods
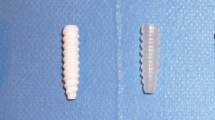
The knees of 21 human cadavers were used for explantation of the hamstring tendons for this study. The age was 41.9 ± 13.1 years (range: 18–60). Explantation was performed on average 2.7 ± 1.3 (0–4) days postmortem. We used the tendons of 14 men and 7 women with a height of 175.7 ± 11.6 (149–190) cm and a weight of 74.9 ± 15.2 (44–100) kg for this investigation. There were no signs of ligament degeneration or local trauma. A bone block was harvested from the tibia medial to the tibial tuberosity (Fig. 1a) in a region where positioning of the tibial tunnel for ACL reconstruction has been recommended [2, 24]. Parts of the block were cortical bone. The block was initially 30 x 11 mm in size and trimmed to be semicircular in shape. The hamstring tendons were looped and had a combined diameter of 7.9 ± 0.6 mm (7–9 mm). For the tibial drill holes, we used the tibiae of 30 German landrace pigs. The pigs were 1-year-old, fully grown, and had a weight between 100 and 120 lbs. All soft tissue was dissected off the bone and the shaft was shortened to 15 cm. The shaft was cemented into an aluminum holder using a polyurethane system (RenCast® FC 53; Huntsman Advanced Materials Ltd., Duxford, Cambridge, England).
A bone block from proximal tibia was harvested in a region where the tibial bone tunnel is usually situated (a). The cortical bone block was trimmed to a conical, semicircular shape. The fixation techniques that were investigated: S/G-grafts were prepared as loops; a retraction tape was passed through the loop (technique T; b). The tape was passed through a 3.2-mm wide hole that created a bone bridge and sutured to this post. The semicircular block was advanced along the medial side of the tibial tunnel until it came to rest close to the tunnel outlet (d). Alternatively, the S/G tendons were sewn together with a modified baseball stitch (technique S; c). The free ends of the sutures were passed through underneath the bone bridge and sutured. The bone block was introduced by analogy with technique T (e). Mechanical tests were conducted with a graft-bone tunnel angle of 0° (d, e). The bone block for the press-fit fixation was inserted from the distal medial side of the tibial tunnel, pressing the graft to the lateral wall of the tunnel (f; A, ACL-footprint; B, bone block; T, transplant)
Graft preparation and fixation
Seven graft constructs were used in each group. The grafts and bone blocks were kept moist during preparation and testing by spraying with a buffered physiologic saline solution, and refrigerated at –20°C before and after preparation until testing.
All bone tunnels were drilled using a drill-press at a flexion angle of the axis of the shaft of the tibia of 30° in the sagittal plane and 15° towards the medial side. This approach was used to imitate the tunnel that is created using a drill guide that allows aiming the tibial tunnel in a direction that facilitates impingement-free positioning and transtibial femoral drilling [12].
Interference screw fixation (I)
The diameter of the tendons was measured and a drill hole of equal diameter was created. A degradable interference screw (Sysorb®; Centerpulse Medical AG, Winterthur, Switzerland) with a screw length of 30 mm and a diameter that exceeded the tunnel width by 1 mm (oversized [31]) was inserted over a guide wire using the instruments and guidelines provided by the manufacturer. The screw was advanced until the proximal outlet of the tunnel.
Press-fit tape fixation (T)
The femoral hamstring press-fit fixation technique described by Paessler [25], leaves a doubled semitendinosus/gracilis loop that can be advanced into the tibial tunnel (Fig. 1b); a 4-mm retraction tape (Mersilene; Ethicon Inc., Somerville, NJ, USA) was passed through this loop and a 10-mm wide bone bridge was created using a 3.2-mm AO drill bit. The diameter of the hamstring tendons was determined, and the size of the bone block was trimmed to a maximum diameter of the tendons diameter plus 2 mm. Then, the diameter of both tendons in combination with the bone plug was determined and the distal cortical end of the tibial tunnel was overdrilled with the diameter of the construct. One end of the tape was introduced through the drill hole and a pretension of 89 N (20 lb) was applied for 5 min. The tape was tied over the bone bridge with five knots. The semicircular bone block was introduced into the distal medial side of the tunnel and advanced with a pusher until it came to rest at the proximal tunnel outlet (Fig. 1d). The bone block was positioned such that its cortical side was facing away from the graft.
Press-fit suture fixation (S)
The second femoral press-fit fixation that has been investigated previously [13], and leaves four separate strands of the graft for tibial fixation (Fig. 1c). Each end of the semitendinosus tendon was sewn to the corresponding end of the gracilis tendon with a modified baseball stitch (Mersilene No. 3 metric, USP 6; Ethicon Inc., Fig. 1c). The size of the tendons and the semicircular bone plug was determined and the distal cortical end of the tibial tunnel was overdrilled to the corresponding diameter. Two of the four suture ends were passed through a bone bridge that was installed by analogy with the first press-fit technique. A pretension of 89 N (20 lb) was applied for 5 min. The sutures were tied with five knots. The bone block was installed by the same means as with the first press-fit technique (Fig. 1e).
Mechanical testing
The constructs were thawed at 4°C for 24 h prior to mechanical testing and kept moist during preparation and testing using buffered physiological saline solution sprayed onto the specimen.
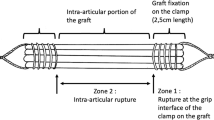
A mechanical testing machine (Mini Bionix 858; MTS Systems Co., MN, USA) was used for the mechanical evaluation of the constructs. The potted tibiae were rigidly fixed in a base platform tilted at 30°, setting the bone tunnel-force direction angle to 0°. This represents a simulation of human ACL reconstructs with a knee flexion angle of 0–30° (Lachman-position [26]; Fig. 1d, e). The distance between the grafts and the clamp was 25 mm, the total length of the free tendons exiting the tunnel was trimmed to 50 mm, leaving 20 mm for fixation in a specially fabricated, s-shaped clamp.
Fixation was performed with the graft centered within the clamp. Then, constructs were pre-tensioned with 50 N for 30 s immediately prior to testing. Subsequently, 1,500 cycles of sinusoidal loading ranging from 50 and 200 N were applied at a repetition rate of 0.5 Hz. The increase in construct length was recorded during cyclical loading. Length changes were reported between first and fifth, fifth and twentieth, twentieth and fiftieth, and fiftieth to 1,500th cycle. After cyclical loading, loading of the specimens was ramped down to 10 N, and after a pause of 30 s the constructs were tested to failure with an actuator speed of 1 mm/s. The maximum failure load, failure mode, and structural stiffness of the constructs were analyzed.
Statistical analysis
All mean values are reported with standard deviations, and ranges. The three groups were compared using a one-way ANOVA. Checks of the normality and equality of variances were conducted. If the normality test failed, a Kruskal-Wallis ANOVA on ranks was executed with a post-hoc Dunn’s Test. If normality test was passed, an ANOVA model with a post-hoc Tukey Test was used. Power tests were used for non-significant findings. All operations were performed using SigmaStat 3.0 (SPSS-company, Chicago, IL 60606, USA). A significance level of 0.05 was used.
Results
Diameter of drill holes
The proximal diameter of the drill hole was 7.75 ± 0.75 mm (range: 7.0–9.0 mm) in group I, 8.43 ± 0.53 mm (range: 8.0–9.0 mm) in group T, and 8.14 ± 0.69 mm (range: 7.0–9.0 mm) in group S with no significant differences being observed (ANOVA, P=0.09). The distal diameter of group I was 8.19 ± 0.65 mm (range: 7.5–9.5 mm), 10.43 ± 0.53 mm (range: 10.0–11.0 mm) in group T, and 9.71 ± 0.57 (range: 8.5–10.0 mm) in group S, which was significantly larger than the I group [(P<0.01); Table 1].
Load to failure
Maximum pull out forces were 970 ± 83 N (range: 853–1,087 N) for the T-fixation, 402 ± 78 N (303–485 N) for the S-fixation, and 544 ± 109 N (440–756 N) for the I-fixation, with all of these values being significantly different (ANOVA, P<0.001; Fig. 2).
Failure mode
None of the fixations failed during cyclic loading. All failures in the T-fixation group were as a result of ruptures of the tape. In one instance, the gracilis tendon and the tape ruptured simultaneously. In the S-fixation group, constructs failed due to rupture of the suture in six cases (86%); and in one test, the tendons were pulled out of the sutures (14%). In the I-fixation group, screw fixation was pulled out of the socket in all instances (100%).
Graft/ fixation stiffness
Stiffness of T-fixation group was lower (78 ± 13 N/mm; range: 59–95 N/mm) than the S-fixation group (108 ± 18 N/mm; 88–145 N/mm). The interference screw fixation demonstrated the highest stiffness (162 ± 27 N/mm; 129–207 N/mm), and all of these differences were significant (P<0.03; Fig. 3).
Length increase during cyclic loading
Cyclical loading elongation determined by the mechanical testing machine in between the first and the fifth loading cycle (Fig. 4) was 2.0 ± 0.6 mm (range: 1.5–3.1 mm) for T-fixation, 3.3 ± 1.1 mm (2.1–5.4 mm) for S-fixation, and 1.4 ± 0.5 mm (0.4–2.6 mm) for I-fixation constructs. Cyclical loading elongation of S-fixation was significantly larger than the other observed techniques (P<0.05). From the fifth to the twentieth loading cycle, length changes were significantly less than over the first five cycles, being reduced to 0.15 ± 0.04 mm (0.08–0.2 mm) for T-fixation, 0.33 ± 0.06 mm (0.27–0.42 mm) for S-fixation, and 0.14 ±0.06 mm (0.06–0.2 mm) for the I-fixation constructs. Elongation of the S-fixation group was still larger than the other groups (P<0.01). In between the twentieth and 1,500th cycle, elongation for T-fixation [2.2 ± 0.07 mm (1.4–3.5 mm)] was significantly smaller than for S-fixation [4.8 ± 0.7 mm (3.7–5.8 mm)] and I-fixation [4.1 ±2.7 mm (2.0–9.9 mm); P<0.001)].
The cyclical loading elongation of the three techniques investigated in this study. Elongation of the S-fixation constructs during the first five cycles and between the fifteenth and twentieth cycles of loading was significantly larger than that of the other fixation techniques (asterisk, ANOVA, Tukey test, P<0.03). Between the 20th and 1,500th cycles, technique T exhibited significantly smaller elongation than T and I (asterisk, ANOVA, Tukey test, P<0.05)
Discussion
The purpose of this study was to investigate the mechanical properties of press-fit tibial fixation of the hamstring tendons in comparison with a well-investigated interference screw fixation.
This study was conducted using human cadavers and young porcine tibiae. Care was taken to explant the tendons shortly postmortem (2.7 ± 1.3 days). The mechanical properties of the tendons of this collective are different from young human tendons; however, most failures were observed as a result of fixation failure rather than tendon rupture.
Recently, there have been concerns about the use of porcine bone for mechanical tests of graft fixations [23]. This study shows that failure loads of interference screw fixations are overestimated in a porcine model compared with the results obtained with human specimens because the spongiosa is more rigid in the porcine bone. It can be assumed that the observed failure loads for the interference screw fixation in this study are higher compared with results that would be obtained using human bone. In our opinion, fixation over a post (as with the T- and S-fixation techniques) are better comparable with results obtained with human specimens, because the cortical bone is similar in both models. Most failures in these groups were a result of suture ruptures. We chose this model so that the results of the present study can be compared with the results of other authors who used a similar set-up [17, 19, 26], and because the specimens were more homogeneous than available human specimens would have been. Our results for failure loads for the interference screw fixation are within the standard deviation of the results of Kousa et al. (612 ± 176 N for BioScrew and 665 ± 201 N for SmartScrew ACL [17]) and Weiler et al. (479 ± 111 N for Arthrex biodegradable screw, 1-mm oversized [30]). The stiffness found for the interference screw fixation was higher than found by Kousa et al. (91 ± 34 N/mm for BioScrew and 115 ± 34 N/mm for Smart Screw ACL [17]). This could be a result of the larger screw diameter in this study. Stiffness of the press-fit fixations of this study were comparable with the results obtained from other postfixations (87 ± 23 N/mm for WasherLoc and 69 ± 14 N/mm for tandem-spiked washers [17]).
Higher strain rates have been used in the investigations of some other authors (30 mm/s [1,18]). The strain rate used in this study (1 mm/s) has been used in most recent investigations [9, 16, 26, 31] and makes the results comparable with our previous investigation [13].
Various different numbers of cycles, recovery periods, and strain magnitudes have been used in order to determine the biomechanical properties of graft fixations [9, 16, 21, 26, 31]. In contrast to our previous investigation [13], we added a long-term test (1,500 cycles) to our protocol. The results suggest that fixation forces are not adequate for both interference screw and suture fixation (4.1 ± 2.7 and 4.8 ± 0.7 mm). However, these results are comparable with the investigation of Kousa et al. [17]. Clinical correlation with long-term knee stability is needed in order to verify these findings.
The present study demonstrates that secure tibial fixation is more difficult to achieve than femoral fixation [13]. There is little angulation of the graft entering the tibial tunnel. Therefore, press-fit techniques add less to the rigidity of the fixation compared with when they are used in the femoral tunnel [21]. However, the T-fixation technique performed well in terms of failure loads and long-term elongation. Graft fixation in 30° of knee flexion has to be recommended to adjust for the initial elongation that is higher than that found for a press-fit BPTB graft (0.7 ± 0.6 mm [13]).
Aggressive rehabilitation protocols have been used successfully in order to rehabilitate ACL-reconstructions using both patellar tendon [27] and hamstring tendon grafts [11]. These protocols repeatedly put loads of more than 200 N on the grafts [20].
To our knowledge, this study is the only investigation that reports data for press-fit hamstring fixation with a bone block for the tibial tunnel. Other authors have analyzed interference screw fixation of hamstring grafts wrapped around a bone block [31]. They found this technique to be of equal quality in terms of mechanical properties compared with a pure tendon fixation. We conclude the same for the T-fixation group of this investigation.
The clinical relevance of a press-fit procedure for the hamstring tendons in the tibial tunnel is the potential of less bone tunnel widening compared with currently used techniques [3, 28]. A further benefit is the possibility to perform MRIs without metal artifacts.
This study demonstrates that a press-fit technique with the hamstring tendons and and autologous bone block demonstrates higher maximum pull out forces when compared with an isolated interference screw fixation. The constructs need to be pretensioned before final fixation. Further clinical studies are necessary to follow up on the healing process of a tibial press-fit fixation. Such studies should include a careful analysis of bone tunnel enlargement.
References
Aune AK, Ekeland A, Cawley PW (1998) Interference screw fixation of hamstring vs patellar tendon grafts for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:99–102
Boszotta H (1997) Arthroscopic anterior cruciate ligament reconstruction using a patellar tendon graft in press-fit technique: surgical technique and follow-up. Arthroscopy 13:332–339
Clatworthy MG, Annear P, Bulow JU, Bartlett RJ (1999) Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc 7:138–145
Fink C, Zapp M, Benedetto KP, Hackl W, Hoser C, Rieger M (2001) Tibial tunnel enlargement following anterior cruciate ligament reconstruction with patellar tendon autograft. Arthroscopy 17:138–143
Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr (2003) Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 31:2–11
Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC (2005) Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy 21:791–803
Herrington L, Wrapson C, Matthews M, Matthews H (2005) Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. Knee 12:41–50
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13:248–255
Hoffmann RF, Peine R, Bail HJ, Sudkamp NP, Weiler A (1999) Initial fixation strength of modified patellar tendon grafts for anatomic fixation in anterior cruciate ligament reconstruction. Arthroscopy 15:392–399
Hoher J, Moller HD, Fu FH (1998) Bone tunnel enlargement after anterior cruciate ligament reconstruction: fact or fiction? Knee Surg Sports Traumatol Arthrosc 6:231–240
Howell SM, Deutsch ML (1999) Comparison of endoscopic and two-incision techniques for reconstructing a torn anterior cruciate ligament using hamstring tendons. Arthroscopy 15:594–606
Howell SM, Lawhorn KW (2004) Gravity reduces the tibia when using a tibial guide that targets the intercondylar roof. Am J Sports Med 32:1702–1710
Jagodzinski M, Behfar V, Hurschler C, Albrecht K, Krettek C, Bosch U (2004) Femoral press-fit fixation of the hamstring tendons for anterior cruciate ligament reconstruction. Am J Sports Med 32:1723–1730
Jansson KA, Harilainen A, Sandelin J, Karjalainen PT, Aronen HJ, Tallroth K (1999) Bone tunnel enlargement after anterior cruciate ligament reconstruction with the hamstring autograft and endobutton fixation technique. A clinical, radiographic and magnetic resonance imaging study with 2 years follow-up. Knee Surg Sports Traumatol Arthrosc 7:290–295
Kohn D, Busche T, Carls J (1998) Drill hole position in endoscopic anterior cruciate ligament reconstruction. Results of an advanced arthroscopy course. Knee Surg Sports Traumatol Arthrosc 6(Suppl 1):S13–S15
Kousa P, Jarvinen TL, Vihavainen M, Kannus P, Jarvinen M (2003) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med 31:174–181
Kousa P, Jarvinen TL, Vihavainen M, Kannus P, Jarvinen M (2003) The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part II: tibial site. Am J Sports Med 31:182–188
Kurosaka M, Yoshiya S, Andrish JT (1987) A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 15:225–229
Magen HE, Howell SM, Hull ML (1999) Structural properties of six tibial fixation methods for anterior cruciate ligament soft tissue grafts. Am J Sports Med 27:35–43
Markolf KL, Gorek JF, Kabo JM, Shapiro MS (1990) Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg [Am] 72:557–567
Musahl V, Abramowitch SD, Gabriel MT, Debski RE, Hertel P, Fu FH, Woo SL (2003) Tensile properties of an anterior cruciate ligament graft after bone-patellar tendon-bone press-fit fixation. Knee Surg Sports Traumatol Arthrosc 11:68–74
Noyes FR, Barber-Westin SD (2001) Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am 83A:1131–1143
Nurmi JT, Sievanen H, Kannus P, Jarvinen M, Jarvinen TL (2004) Porcine tibia is a poor substitute for human cadaver tibia for evaluating interference screw fixation. Am J Sports Med 32:765–771
Odensten M, Gillquist J (1986) A modified technique for anterior cruciate ligament (ACL) surgery using a new drill guide for isometric positioning of the ACL. Clin Orthop 154–158
Paessler HH, Mastrokalos DS (2003) Anterior cruciate ligament reconstruction using semitendinosus and gracilis tendons, bone patellar tendon, or quadriceps tendon-graft with press-fit fixation without hardware. A new and innovative procedure. Orthop Clin North Am 34:49–64
Seil R, Rupp S, Krauss PW, Benz A, Kohn DM (1998) Comparison of initial fixation strength between biodegradable and metallic interference screws and a press-fit fixation technique in a porcine model. Am J Sports Med 26:815–819
Shelbourne KD, Nitz P (1990) Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med 18:292–299
Webster KE, Feller JA, Hameister KA (2001) Bone tunnel enlargement following anterior cruciate ligament reconstruction: a randomised comparison of hamstring and patellar tendon grafts with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 9:86–91
Weiler A, Hoffmann RF, Bail HJ, Rehm O, Sudkamp NP (2002) Tendon healing in a bone tunnel. Part II: Histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy 18:124–135
Weiler A, Hoffmann RF, Siepe CJ, Kolbeck SF, Sudkamp NP (2000) The influence of screw geometry on hamstring tendon interference fit fixation. Am J Sports Med 28:356–359
Weiler A, Hoffmann RF, Stahelin AC, Bail HJ, Siepe CJ, Sudkamp NP (1998) Hamstring tendon fixation using interference screws: a biomechanical study in calf tibial bone. Arthroscopy 14:29–37
Yunes M, Richmond JC, Engels EA, Pinczewski LA (2001) Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: a meta-analysis. Arthroscopy 17:248–257
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jagodzinski, M., Scheunemann, K., Knobloch, K. et al. Tibial press-fit fixation of the hamstring tendons for ACL-reconstruction. Knee Surg Sports Traumatol Arthrosc 14, 1281–1287 (2006). https://doi.org/10.1007/s00167-006-0105-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0105-y