Abstract
This study compared hamstring (HS) and patellar tendon (PT) anterior cruciate ligament (ACL) reconstruction in females. Sixty-five patients (43 HS, 22 PT) were evaluated at a mean 3.8-year postoperatively. Evaluation included IKDC 2000, SF-36, Cincinnati sports activity scores, anterior knee pain (AKP), kneeling pain, range of motion and anterior knee laxity. One PT patient sustained a traumatic graft rupture. There were no differences between the two grafts in terms of anterior knee laxity or IKDC scores. The HS group had higher sports activity scores and higher scores on the Physical Functioning and General Health subscales of the SF-36. Despite no difference in AKP, there was greater kneeling pain in the PT patients, who also had greater extension deficits. Both HS and PT are satisfactory ACL grafts in females, but HS grafts were associated with less morbidity, greater return to preinjury level of activity and higher quality of life scores.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most frequently used autografts for anterior cruciate ligament (ACL) reconstruction are the central third bone-patellar tendon-bone graft and the hamstring (HS) tendon graft, usually combined semitendinosus and gracilis tendons. Randomised clinical trials have shown satisfactory and similar functional outcomes for both graft types [3, 5, 7–10, 14, 19, 23]. However, some of these studies have demonstrated less morbidity with HS grafts than with patellar tendon (PT) grafts, particularly with regard to pain on kneeling and extension deficit [5, 8–10].
None of these studies has focused specifically on the outcome in females. Study populations have included both males and females, with most studies having a majority of males. In contrast to the general trend of the results of the randomised trials, in a study of only female subjects Barrett et al. [6] reported a higher failure rate for HS grafts (23%) than for PT grafts (8%). In addition, the authors reported a reduced rate of return to preinjury activity levels and increased pain with HS grafts compared to PT grafts. A more recent study by Gobbi et al. [12] also found significantly increased anterior knee laxity at 3 years in females with HS grafts compared to males with HS grafts and females with PT grafts.
In this study, we examined a cohort of female subjects who had undergone ACL reconstruction by one surgeon with either a PT or HS tendon autograft between 2 and 6 years previously.
Patients and methods
From March 1998 to February 2001, 131 skeletally mature female patients underwent primary ACL reconstruction by one experienced knee surgeon, using either autogenous HS or PT grafts. During the 3-year period in which the procedures were performed the grounds for deciding on a particular graft for an individual varied, reflecting the lack of evidence to clearly support one graft at that time. In the community in which the surgeries were performed there was a high level of awareness about ACL reconstruction because of extensive media coverage in relation to professional sporting injuries. As a result, patients with an ACL rupture frequently had preconceived ideas about graft selection prior to attending an orthopaedic surgeon for consultation regarding their injury. In such situations it was the treating surgeon’s policy to use the graft that the patient had preselected.
There were however two consistent indications for PT grafts; chronic ACL insufficiency and ACL reconstruction in combination with a collateral ligament repair or reconstruction. Therefore, patients who underwent ACL reconstruction more than 12 months after injury and patients with collateral ligament injuries of greater than grade II severity were excluded from the present study. In addition, we excluded patients with marked ACL insufficiency as defined by a 3+ Lachman test or a gross pivot-shift test on examination under anaesthesia at the commencement of their surgery. Patients with radiographic evidence of osteoarthritis or arthroscopic evidence of cartilage disruption of greater than Noyes grade IIA or Noyes IIA greater than 1 cm in diameter [18] were also excluded. Finally, we excluded patients who were pregnant at the time of the study.
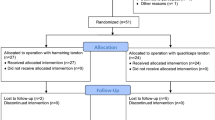
After applying these criteria, 94 females (61 HS, 33 PT) were potentially available for inclusion and were invited to attend for review. Twenty were lost to follow-up, six were overseas, and three were too busy to participate. One HS patient was unhappy with her outcome and declined to take part. Sixty five patients agreed to participate (43 HS, 22 PT). One PT patient had ruptured the graft 20 months after surgery whilst playing netball. She had been playing without problems for 13 months prior to re-injury. As this patient had subsequently undergone revision ACL reconstruction with a good outcome and a successful return to sport, she was not reviewed. Subjects were informed about the study before consenting to participate.
Characteristics of the study sample are shown in Tables 1 and 2. All ACL injuries occurred during sporting activity and, preoperatively, the PT and HS groups were similar in terms of age, preinjury Cincinnati sports activity score [17], time from injury to surgery, and examination findings at operation. The follow-up was a mean of 3.6 years in the HS group and of 3.9 years in the PT group. There were no significant differences between the two groups. On this basis, it was felt that it was reasonable to proceed with a comparative analysis.
Surgical technique
All patients had undergone an arthroscopically assisted single-incision ACL reconstruction. In the HS group, the gracilis and semitendinosus tendons were harvested through an oblique 3–4 cm incision. In the PT group, a central third bone-tendon-bone graft was harvested through a 5–7 cm longitudinal incision. The femoral tunnel was drilled using a trans-tibial technique. All grafts were statically pretensioned at 20 lb (89 N) for 5 min prior to insertion. Graft fixation was the same in both groups. Femoral fixation was by means of an EndoButton (Smith and Nephew Endoscopy, Mansfield, MA, USA) attached to the graft with a doubled loop of 3-mm polyester tape. On the tibial side all grafts were fixed with a 7 × 25 mm absorbable PLLA interference screw (Phantom Interference Screw, DePuy Orthopaedic Technology Inc., Warsaw, IN, USA). In the PT group, the PT defect was loosely closed with interrupted absorbable sutures. Although, the donor sites on the patella and tibial tubercle were not formally bone grafted, bone fragments from trimming of the graft were placed in the tibial tubercle defect. Patients were discharged from hospital on the first postoperative day.
Associated pathology
In the HS group there were seven (16%) medial meniscal tears; two were stable and not treated, one was repaired using an inside to out technique and the remaining four were treated by partial meniscectomy. There were 12 (28%) lateral meniscal tears; five were stable and the remaining seven underwent partial meniscectomy. One medial femoral condyle lesion was also debrided. In the PT group there were five (23%) medial meniscal tears; one was repaired using an inside to out technique and the remaining four underwent partial meniscectomy. There were seven (33%) lateral meniscal tears; three were stable and the remaining four underwent partial meniscectomy.
Postoperative management
Postoperatively all patients used the same rehabilitation protocol. The protocol emphasised early restoration of full extension and quadriceps function and allowed weight bearing on an as tolerated basis from the first postoperative day. No braces or splints were used. Progression was on an as tolerated basis, being guided by the presence and degree of pain and swelling. Apart from isometric exercises with the knee in full extension, quadriceps-strengthening exercises were restricted to closed kinetic chain exercises during the first 3 months. Patients were allowed to ride an exercise bicycle from 2 weeks postoperatively and were allowed to start gymnasium exercises (leg press, half squats, step ups and HS curls) from 6 weeks. Running was allowed from 10 weeks and sports-specific drills from 3 months. Patients were allowed to return to competitive sport from 8 months, provided there was no effusion, a normal range of motion, satisfactory stability and good quadriceps function.
Evaluation
All patients completed a questionnaire, which included the IKDC 2000 subjective knee evaluation form [13], the SF-36 [25] and the Cincinnati Sports Activity Scale [17]. The following two questions were added to the subjective knee form: “Do you have pain at the front of your knee?” and “Do you have pain when you kneel?” The response format for these additional questions was identical to that of the subjective knee form (zero = no pain, ten = worst pain imaginable).
Patients were then examined by a single orthopaedic surgeon who was not involved in the patients’ care and who completed the IKDC 2000 knee examination form. The examiner was not blinded to graft type as they were the only person involved in reviewing the patients. The treating surgeon was unaware of the results until all data collection had been completed. The passive ranges of extension and flexion of both knees were recorded using a goniometer with the subject supine. The deficit of the operated limb relative to the non-operated limb was recorded. KT-1000 arthrometer (MEDmetric, San Diego, CA, USA) measurements of side-to-side differences in anterior tibial displacement were recorded at 134 N (30 lb). The Lachman test was recorded and graded as normal, 1+, 2+ or 3+. The pivot-shift test was also performed on both knees and graded as normal, glide, clunk or gross. One PT patient and three HS patients did not complete the examination component of the review.
Statistical analysis
Data were analysed using independent samples t-tests, the Mann–Whitney U-test and contingency tables to compare HS and PT groups. The significance level was set at P < 0.05.
Results
Pain and IKDC subjective knee evaluation
Data for the recorded pain variables is shown in Table 3. There were no significant differences in the incidence or the severity of anterior knee pain (AKP) between the two groups. In contrast, the incidence (P < 0.01) and severity (P < 0.01) of pain on kneeling were significantly greater in the PT group. IKDC subjective knee evaluation scores were not significantly different between the two groups (HS mean 89.5, ranges 59–100; PT mean 86.5, ranges 61–99).
SF-36
The HS group scored significantly higher on the physical functioning (P = 0.02) and general health subscales (P = 0.03) of the SF-36 (Fig. 1). There was no difference between the groups for the other subscales.
Cincinnati Sports Activity Scale
Sports activity scores were significantly higher in the HS group (P = 0.04). The median score was 85 (ranges 55–100) compared to 80 (ranges 40–100) in the PT group. A greater number of HS patients had also returned to their preinjury score (HS 60%; PT 33%, P = 0.04).
IKDC knee evaluation form
There was no difference in the distribution of IKDC categories between the two groups. Overall, 24 (40%) patients were graded normal (38% HS, 45%PT) and 35 (59%) as nearly normal (60% HS, 55% PT). There was one patient who rated abnormal in the HS group. No patients rated severely abnormal.
Ligament examination
The mean KT-1000 side-to-side difference in anterior tibial displacement at 134 N was 1.7 mm (ranges −1 to 4) in the HS group and did not differ from the mean of 1.8 mm (ranges 0–5) in the PT group. All patients had 5 mm or less side-to-side difference and the majority in both groups (HS: 70%, PT: 75%) had a side-to-side difference of 2 mm or less. The Lachman grades reflected the KT-1000 measurements with 44 (73%) patients having a normal test and the remainder having 1+ laxity.
In the HS group 29 (72.5%) patients had a normal pivot-shift test, 10 (25%) had a pivot glide and one (2.5%) had a pivot clunk. In the PT group there were 15 (75%) patients with a normal pivot-shift test, and 5 (25%) with a pivot glide.
Range of motion
Although small in magnitude, extension deficits were significantly greater in the PT group (HS mean 1.0°, ranges −2 to 5°; PT mean 1.9°, ranges 0 to 5°, P = 0.04). Flexion deficits were not significantly different between the groups (HS mean 1.4°, ranges −4 to 12°; PT mean 0.5°, ranges −3 to 4°).
Complications
There were no immediate postoperative complications that required re-operation or readmission. Three patients in the HS group required a subsequent procedure within 12 months. Two underwent arthroscopy for notch impingement and one had a manipulation under anaesthesia for a restricted range of flexion. There were no subsequent procedures within 12 months in the PT group.
Discussion
This mid term follow up of ACL reconstruction in athletically active females showed no significant differences between HS and PT grafts in terms of knee laxity and rate of graft rupture but did show differences in favour of HS grafts in terms of morbidity, return to activity and quality of life.
The laxity findings contrast with those of Barrett et al. [6] who reported a higher failure rate with HS grafts based on the presence of a 1+ or more pivot-shift test, a KT-1000 difference of more than 5 mm, a 2+ or more Lachman test or revision surgery. The use of a 1+ pivot shift as an indicator of failure is more rigorous than the IKDC, which classifies such a pivot shift as nearly normal. If the IKDC criteria are applied to Barrett’s data and only categories abnormal and severely abnormal are regarded as failures, the failure rate for HS grafts is 13% compared to 8% for PT grafts. This is more in keeping with our observations and may be more appropriate given that there is a subjective element in the assessment of the pivot-shift test.
Our findings are also in contrast with those of Gobbi et al. [12] who reported that at an average of 3 years, females who had undergone ACL reconstruction with a HS graft had significantly more anterior laxity (1.7 mm) than females who had undergone ACL reconstruction with a PT graft (1.0 mm). However, it is worth noting that unlike the present study, Gobbi et al. did not use the same fixation methods for both graft types. The HS grafts had suspensory fixation at both ends, which may have contributed to increased laxity compared to the PT grafts, which had aperture fixation on the femoral side and suspensory fixation on the tibial side. In our study, both grafts had suspensory fixation on the femoral side and interference screw fixation on the tibial side.
Similar to previous studies that have compared HS and PT grafts, we did observe a small but significant extension deficit in the PT group compared to HS group [1, 2, 9, 10]. This is probably of little clinical relevance. One might have expected that due to increased ligamentous laxity compared to males, extension deficits would be minimized in a study population consisting entirely of females. However, our results are in fact consistent with previous studies, which had a preponderance of male subjects [9, 10]. This increased extension deficit associated with PT grafts has previously been attributed to donor site morbidity [20–22].
Assessment of pain on kneeling revealed possibly the most clinically significant difference between the two graft types. The incidence and severity of pain on kneeling were greater in the PT group. Once again this reflects the findings of randomised controlled trials, which have used this outcome measure in mixed gender populations [4, 5, 8–10]. Increased pain on kneeling seems to be related to the harvest site for PT grafts [11]. It has previously been reported that tenderness over the inferior pole of the patella occurs particularly if the patellar bone defect is grafted rather than left open [15]. Although we placed bone chips from shaping of the bone blocks in the tibial tubercle defect no bone graft was applied to the patellar defects in the patients in this study.
Quantitative assessment of activity can be difficult because scores need to take into account both the frequency and the type of exercise. The scale we chose to use, the Cincinnati Sports Activity Scale, does both. Although the median scores of 85 in the HS group and 80 in the PT group reflect a similar frequency of participation (1–3 days/weeks), there is a difference in the type of exercise reflected by these scores. A score of 85 indicates participation in sports that involve jumping, hard pivoting and cutting, whereas 80 indicates participation in sports that do not involve these manoeuvres.
It has been suggested that there is a role for generic health outcome measures in evaluating surgical procedures [16]. We therefore used the SF-36, which showed differences with the HS group scoring significantly higher on the Physical Functioning and General Health subscales. This is in fact consistent with the greater number of HS subjects (60%) who had returned to their preinjury activity level compared to the 33% of PT subjects.
Although this study was not a randomised comparison, we used strict inclusion criteria to reduce the number of potentially confounding variables and to maximize the strength of the study. Only patients with a relatively isolated ACL rupture were included. Patients who had chronic ACL insufficiency (greater than 1 year from injury to surgery) were excluded, as were patients with marked laxity preoperatively. A single surgeon performed all procedures and one investigator, who was not involved in the patients’ care, examined all patients. Apart from graft harvest, the surgical technique, including fixation technique, was identical for both groups. The effectiveness of the inclusion and exclusion criteria is demonstrated by the similarity of the characteristics of the two groups.
We recognise that due to non-randomisation of graft type there was a potential for selection bias. The period in which these patients underwent surgery coincided with the time when many of the recent randomised controlled trials comparing the two grafts were being conducted and analysed. As a result there was less information than is available today to enable surgeons to make an evidence-based decision regarding graft selection. Therefore, we feel that the potential for selection bias was at least partially mitigated by the treating surgeon’s uncertainty about the indications for each graft type during the period of the study. Furthermore, where consistent indications were used, steps were taken to exclude the relevant patients. In addition, accepting a patient’s preconceived preference for a particular graft type added further inconsistency (and therefore less potential for selection bias) to the graft allocation process.
Our overall follow up rate was 69%, just below the generally recommended rate of 70% being regarded as acceptable [24]. Importantly the rate of follow up for both grafts types was essentially the same (70% HS; 67% PT). As a result we do not believe that transfer bias is likely to have had a significant impact on this study.
Given that the two subject groups were comparable and that our findings are in accordance with those reported from randomised studies in mixed gender populations, we believe that the results of this study indicate that HS tendon grafts are a satisfactory alternative to PT grafts for females undergoing ACL reconstruction.
References
Aglietti P, Buzzi R, D’Andria S, Zaccherotti G (1993) Patellofemoral problems after intra-articular anterior cruciate ligament reconstruction. Clin Orthop 288:195–204
Aglietti P, Buzzi R, Zaccherotti G, De Biase P (1994) Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med 22:211–217
Anderson AF, Snyder RB, Lipscomb AB Jr (2001) Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am J Sports Med 29:272–279
Aune AK, Ekeland A, Cawley PW (1998) Interference screw fixation of hamstring vs patellar tendon grafts for anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 6:99–102
Aune AK, Holm I, Risberg MA, Jensen HK, Steen H (2001) Four-strand hamstring tendon autograft compared with patellar tendon- bone autograft for anterior cruciate ligament reconstruction: a randomized study with two-year follow-up. Am J Sports Med 29:722–728
Barrett G, Noojin F, Hartzog C, Nash C (2002) Reconstruction of the anterior cruciate ligament in females: a comparison of hamstring versus patellar tendon autograft. Arthroscopy 18:46–54
Beynnon B, Johnson R, Fleming B, Kannus P, Kaplan M, Samani J, Renstrom P (2002) Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am 84:1503–1513
Ejerhed L, Kartus J, Sernert N, Kohler K, Karlsson J (2003) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med 31:19–25
Eriksson K, Anderberg P, Hamberg P, Lofgren A, Bredenberg M, Westman I, Wredmark T (2001) A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br 83:348–354
Feller JA, Webster KE (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31:564–573
Feller JA, Webster KE, Gavin B (2001) Early post-operative morbidity following anterior cruciate ligament reconstruction: patellar tendon versus hamstring graft. Knee Surg Sports Traumatol Arthrosc 9:260–266
Gobbi A, Domzalski M, Pascual J (2004) Comparison of anterior cruciate ligament reconstruction in male and female athletes using the patellar tendon and hamstring autografts. Knee Surg Sports Traumatol Arthrosc 12:534–539
Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelbourne KD (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29:600–613
Jansson K, Linko E, Sandelin J, Harilainen A (2003) A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 31:12–18
Kohn D, Sander Beuermann A (1994) Donor-site morbidity after harvest of a bone-tendon-bone patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc 2:219–223
Mohtadi NGH (1993) Quality of life assessment as an outcome in anterior cruciate ligament reconstructive surgery. In: Jackson DW (ed) The anterior cruciate ligament: current and future concepts. Raven Press Ltd., New York, pp 439–444
Noyes FR, Barber SD, Mooar LA (1989) A rationale for assessing sports activity levels and limitations in knee disorders. Clin Orthop 246:238–249
Noyes FR, Stabler CL (1989) A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med 17:505–513
O’Neill DB (1996) Arthroscopically assisted reconstruction of the anterior cruciate ligament. A prospective randomized analysis of three techniques. J Bone Joint Surg Am 78:803–813
Rosenberg TD, Franklin JL, Baldwin GN, Nelson KA (1992) Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Am J Sports Med 20:519–525
Rubinstein RA Jr, Shelbourne KD, VanMeter CD, McCarroll JC, Rettig AC (1994) Isolated autogenous bone-patellar tendon-bone graft site morbidity. Am J Sports Med 22:324–327
Sachs RA, Daniel DM, Stone ML, Garfein RF (1989) Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med 17:760–765
Shaieb M, Kan D, Chang S, Marumoto J, Richardson A (2002) A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med 30:214–220
Spindler KP Reading the literature to change your clinical practice. ISAKOS: Current Concepts: Graft choice for ACL reconstruction. http://www.isakos.com/innovations/spindler.html
Ware JJ, Sherbourne C (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siebold, R., Webster, K.E., Feller, J.A. et al. Anterior cruciate ligament reconstruction in females: a comparison of hamstring tendon and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc 14, 1070–1076 (2006). https://doi.org/10.1007/s00167-006-0100-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0100-3