Abstract
Female athletes incur anterior cruciate ligament ruptures at a rate at least twice that of male athletes. Hypothesized factors for the increased injury risk in females include biomechanical, neuromuscular, and hormonal differences between genders. A wealth of literature exists examining these potential predispositions individually, but the interactions between these factors have not been examined extensively. Our purpose was to investigate changes in neuromuscular control and laxity at the knee across the menstrual cycle of healthy females. Fourteen female collegiate athletes with normal, documented ovulatory menstrual cycles, confirmed ovulation, and no history of serious knee injury participated. The presence and timing of ovulation was determined during a screening cycle with ovulation detection kits and during an experimental cycle with collection of daily urine samples and subsequent analysis of urinary estrone-3-glucuronide (E3G) and pregnanediol-3-glucoronide (PdG), which correlate with circulating estrogen and progesterone. Each subject had measures of knee neuromuscular performance and laxity once during the mid-follicular, ovulatory, and mid-luteal stages of her menstrual cycle. The test battery included assessments of knee flexion and extension peak torque, passive knee joint position sense, and postural control in single leg stance. Knee joint laxity was measured with an arthrometer. Analyses of variance revealed that E3G and PdG levels were significantly different across the three testing sessions, but there were no significant differences in the measures of strength, joint position sense, postural control, or laxity. No significant correlations were found between changes in E3G or PdG levels and changes in the performance and laxity measures between sessions. These results suggest that neuromuscular control and knee joint laxity do not change substantially across the menstrual cycle of females despite varying estrogen and progesterone levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Female athletes tear their anterior cruciate ligaments (ACL) at rates between two and eight times more often than their male counterparts [1, 2]. Numerous factors have been hypothesized to influence this increased injury risk including gender differences related to anatomical structure, neuromuscular function, joint laxity, and hormonal fluctuations [12]. While several studies have examined these factors in isolation, few have examined the interrelationships between these hypothesized risk factors.
The role of increased circulating estrogen and progesterone on ACL injury risk has been studied in a variety of paradigms. Some researchers have reported that females are at greater risk of tearing their ACL during the ovulatory phase of their menstrual cycle when there is a surge is circulating estrogen [27, 28], while others have reported that there is greater risk in the week preceding the onset of menstruation (luteal phase) when there is a sustained increase in progesterone relative to the early follicular phase [19, 21]. A limitation of these studies, however, is that menstrual cycle phase has been determined by patient self-report and without hormone confirmation. Ovulation is preceded by a large surge in estrogen, while there is also a somewhat elevated level of estrogen in the follicular phase although not to the extent of that seen just prior to ovulation. Estrogen has been shown to have deleterious effects on the collagen structure of the ACL in vitro [17, 26, 29, 30]. Similarly, some evidence suggests that increases in estrogen in vivo are associated with increased knee laxity as assessed with an instrumented arthrometer [5, 11]. However, there is no concrete evidence associating increased knee laxity with increased injury risk.
Gender differences related to neuromuscular differences at the knee have also been suggested as a potential cause of ACL injury risk in female athletes. Females have been postulated to utilize a dynamic protective strategy to perturbation at the knee which is more quadriceps dominant than that of males [13]. The reliance of males on a more hamstring dominant strategy may be more protective of the ACL because the hamstrings and ACL have agonist functions in preventing anterior displacement of the tibia on the femur. Additionally, females have been shown to have impaired proprioception assessing knee motion into extension than males [24]. This delayed recognition of joint position coupled with a quadriceps dominant dynamic defense mechanism to knee perturbation may place females at greater ACL injury risk. There is also mounting evidence that estrogen influences electrical activity of neurons both centrally and peripherally [16, 23, 24].
To date, there have only been a few studies that have examined fluctuations in multiple measures of lower extremity neuromuscular performance across the menstrual cycle of healthy, physically active females [7–10]. Friden et al. [7] found no significant changes in peak torque and muscular endurance of the knee extensors and performance on a single leg-hopping task across three phases of the menstrual cycle. In a follow-up study, they found that knee joint kinesthesia was significantly impaired in the premenstrual phase and hopping performance was improved in the ovulation phase [10]. Friden et al. [8, 9] have also demonstrated postural control impairments in females with premenstrual symptoms in the mid-luteal phase. These findings support the hypothesis that lower extremity neuromuscular performance may be influenced by circulating sex hormones. Our purpose was to assess measures of hamstring and quadriceps strength, knee joint position sense, postural control, and knee joint laxity at three points across the menstrual cycle of healthy female athletes.
Materials and methods
Subjects
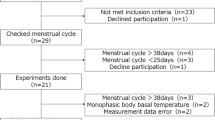
Fourteen healthy female collegiate athletes (age=19.3±1.3 years, height=163.6±8.5 cm, mass=59.4±6.8 kg) who were experiencing normal menstrual cycles (28–35 day cycles) with confirmed ovulation and who were not taking oral contraceptive pills completed all aspects of the study. Subjects participated in either competitive soccer or stunt cheerleading and were free of previous knee injuries and had no history of menstrual disorders. Before participating in the study, all subjects read and signed an informed consent form approved by the Pennsylvania State University Institutional Review Board.
Estimation of circulating hormones
During month 1 of the study, potential subjects monitored the length of their menstrual cycle and confirmed that they ovulated using commercially available ovulation detection kits (First Response®, Church and Dwight Inc., Princeton, NJ, USA). While we initially enrolled 20 females in the study, 6 potential subjects who did not ovulate during month 1 or had a menstrual cycle that did not last between 28 and 35 days were excluded from participation in the rest of the study.
During month 2, subjects collected daily morning urine samples throughout the length of their cycles. Subsequent analysis of urinary estrone-3-glucuronide (E3G) and pregnanediol-3-glucoronide (PdG), which correlate with circulating estrogen and progesterone, were used to verify that subjects had normal cycles that included ovulation using methods previously reported by McConnell et al. [18]. These methods have been previously validated [20]. A pair of endocrinologists who reviewed the hormone measurements assessed the presence or absence of ovulation for each subject.
Testing schedule
Subjects underwent the neuromuscular performance and laxity testing battery on three occasions: mid-follicular phase (4–7 days before predicted ovulation), ovulatory (±2 days of predicted ovulation), and mid-luteal (7–10 days after predicted ovulation). The day of predicted ovulation was based on the day of ovulation and the length of the cycle in month 1. On the first day of testing, subjects were familiarized with all testing procedures prior to data collection.
Strength testing
Quadriceps and hamstring strength were quantified using an isokinetic dynamometer (Biodex Corp., Shirley, NY, USA) to test concentric force production in knee extension and flexion. Subjects performed 10 repetitions of maximum flexion and extension at a speed of 120°/s. Dependent variables included hamstring and quadriceps peak torque and the ratio of hamstring to quadriceps peak torque. All peak torque values were normalized to subjects body mass.
Joint position sense
Passive joint position sense was assessed using an isokinetic dynamometer (Biodex Corp., Shirley, NY, USA). Subjects performed two trials of passive joint position sense testing on each limb with the target positions being 15° and 30° of knee flexion. Subjects sat in dynamometer chair with the test limb beginning at 90° of knee flexion. The limb was passively moved by the dynamometer at 2°/s until it reached the target position. The limb was then held at the target position for 5 s and then passively returned to the start position. The limb was again moved passively toward the target position and the subject was instructed to hit a switch when she felt the limb had reached the target angle. Absolute degrees of error from the target angle served as the dependent variable.
Postural control
Postural control was assessed with an AMTI Accusway (AMTI Inc, Watertown, MA, USA) force platform. Subjects completed three 10-second trials while standing on the right and left legs in unilateral stance. Subjects stood with their eyes open and their arms folded across their chest and were instructed to stand as still as possible for the duration of the trial. Data were collected at a rate of 50 Hz. Velocity of center of pressure (COP) excursions served as the dependent variable for postural control.
Knee laxity
Knee joint laxity was assessed by quantifying anterior tibial translation using a KT-1000 knee arthrometer (Medmetric Corp., San Diego, CA USA). During each testing session, three trials of laxity measures for each limb were taken with 133 N of force applied to the arthrometer. The mean of the three trials was calculated and served as the dependent variable for knee joint laxity.
Statistical analysis
Data from the neuromuscular performance and laxity measures from the right and left limbs were averaged together and used for analyses. For each dependent variable, a repeated measure ANOVA was run to determine the differences within the testing sessions.
Additionally for each dependent variable, change scores between the mid-luteal and ovulatory measures, and mid-luteal and mid-follicular measures, were calculated. Pearson product moment correlations were then calculated between changes in the neuromuscular performance and laxity measures and E3G and PdG levels, respectively. The level of significance was set a priori at p<0.05 for all analyses.
Results
Repeated measures ANOVA revealed that E3G and PdG levels were significantly different across the three testing sessions (p<0.05). The highest E3G levels were found on the ovulatory test day and peak PdG levels were found in the mid-luteal phase. There were not, however, any significant differences identified in knee extension or flexion peak torque, hamstring:quadriceps ratio, passive knee joint position sense at 15° or 30°, postural control, or knee joint laxity across the three testing sessions. All but one (joint position sense at 15°) of the neuromuscular control and laxity measures had post hoc power (1-ß) values greater than or equal to 0.75 indicating that our non-significant findings are unlikely due to an inadequate sample size. Means, standard deviations, p-values, and power calculations for all dependent variables are shown in Table 1.
There were no significant bivariate correlations between changes in the E3G or PdG levels and changes in any of the neuromuscular performance and laxity measures (Tables 2, 3).
Discussion
Our aim was to simultaneously examine potential alterations in several potential risk factors of ACL injuries across the menstrual cycle of female athletes while also measuring sex hormone levels. Our findings appear to demonstrate that there are no substantial fluctuations in hamstring and quadriceps muscle strength, knee joint position sense, postural control, and knee joint laxity across the course of a normal menstrual cycle in female athletes.
Previous authors report conflicting results regarding changes in knee laxity across the menstrual cycle. Karageanes et al. [15] found no increase in knee laxity across the menstrual cycle of high school athletes. Our results also revealed no significant changes in laxity across the menstrual cycle. Conversely, Heitz et al. [11] found an increase in knee laxity in the ovulatory and luteal phases compared to the follicular phase, but there was no direct correlation between increased laxity and increased serum estrogen levels. Likewise, Deie et al. [5] found increases in anterior knee laxity in the luteal and ovulatory phases compared to the follicular phase in females. No differences were seen across testing sessions in males. There may not be direct correlations between estrogen levels and joint laxity measures because changes in the viscoelastic properties of the ACL in response to increased circulating estrogen may not be immediate. Further research in this area is warranted.
We did not identify substantial quadriceps and hamstring strength deficits across the menstrual cycle. These findings are consistent with previous studies that did not find alterations in knee strength at different points in the menstrual cycle [6, 7, 14]. Conversely, Sarwar et al. [25] found that quadriceps and grip strength were both weakened in the mid-follicular and mid-luteal phases compared to the ovulatory phase; while Davies et al. [3] found grip strength and standing long jump performance to be superior during the menstrual phase with respect to the follicular and luteal phases.
We did not demonstrate changes in passive knee joint position sense or postural control during single leg stance across the menstrual cycle. These are common measures of proprioception and neuromuscular control, respectively. If increased estrogen did have a deleterious effect on sensorimotor function, we thought that one or both of these measures would be altered. Our findings are in contrast to the findings of Friden et al. who have reported impairments in knee joint kinesthesia during the premenstrual phase [10] and postural control in the mid-luteal phase [8, 9]. Interestingly, these deficits were greater in women complaining of premenstrual symptoms compared to those not reporting such symptoms. The interactions between sex hormones, proprioception and neuromuscular control, premenstrual symptoms, and ACL injury risk require further study.
The findings of our study are strengthened by the lack of significant correlations between changes in E3G and PdG and changes in the performance and laxity measures between testing days. One would expect that if estrogen or progesterone were either adversely or positively affecting neuromuscular performance or laxity, there would be strong correlations in the change scores of these measures.
While 14 subjects completed our entire study, we were forced to exclude 6 potential subjects because they ovulated in month 1, but did not ovulate in month 2 of our study. DeSouza et al. [4] studied the characteristics of three consecutive menstrual cycles in groups of moderately exercising and sedentary young adult females who were menstruating normally. They reported that only 45% of menstrual cycles were ovulatory in the exercising group, while the sedentary group had ovulatory cycles 90% of the time. Additionally, no sedentary women (0%) had inconsistent menstrual cycle classifications from cycle to cycle, but 46% of the exercising women were inconsistent. Estrogen and progesterone do not fluctuate as greatly in anovulatory cycles as they do in ovulatory cycles. It is possible that physically active females who have inconsistent ovulation across repetitive menstrual cycles may be at an increased risk of ACL injuries because of inconsistent estrogen and progesterone surges between cycles. In other words, the ACL of a female who undergoes ovulatory cycles on a consistent basis may respond in a predictable fashion to repetitive increases in circulating estrogen and progesterone. Conversely, the ACL of a female who undergoes ovulatory cycles on an inconsistent basis may respond in an unpredictable fashion to an occasional increase in circulating estrogen or progesterone. Exploration of this hypothesis is warranted.
Our study was not without limitations. Our “ovulatory” testing session did not always correspond with the day of ovulation of our subjects. Due to logistic constraints, our testing schedule was based on the day of the cycle on which ovulation occurred in month 1. Variations were seen in the day of ovulation between the consecutive cycles, however, we did measure hormone levels where previous researchers have relied on patient self-reports of menstrual cycle phase. Secondly, our assessments of neuromuscular performance at the knee did not involve neuromuscular responses to knee joint perturbations during weight bearing such as is the typical mechanism of non-contact ACL rupture seen in female athletes. It is possible that our testing battery was not specific enough to assess the dynamic defense mechanism that protects the ACL during sporting activities. Lastly, we chose to have all subjects have their first testing day be in the follicular phase rather than randomizing the phase in which they were first tested. It is possible that systematic learning effects may have occurred due to our study design. It is our recommendation that future research examine joint laxity and neuromuscular function on a more regular basis, such as every 3 days throughout the length of the cycle, or perhaps daily across those days closest to expected ovulation and onset of menstruation to gain a more concrete representation of changes that may occur with regard to fluctuations in circulating estrogen and progesterone.
In conclusion, we did not identify substantial changes in hamstring or quadriceps strength, passive knee joint position sense, postural control in single leg stance, or knee joint laxity across the menstrual cycle of female athletes. Further research is needed to further examine the interrelationships between different potential risk factors for ACL injuries in female athletes.
References
Arendt EA, Dick R (1995) Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med 23:694–701
Arendt EA, Agel J, Dick R (1999) Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Training 34:86–92
Davies BN, Elford JC, Jamieson KF (1991) Variations in performance in simple muscle tests at different phases of the menstrual cycle. J Sports Med Phys Fitness 31:532–537
De Souza MJ, Miller BE, Loucks AB, Luciano AA, Pescatello LS, Campbell CG, Lasley BL (1998) High frequency of luteal phase deficiency and anovulation in recreational women runners: blunted elevation in follicle-stimulating hormone observed during luteal-follicular transition. J Clin Endocrinol Metab 83:4220–4232
Deie M, Sakamaki Y, Sumen Y, Urabe Y, Ikuta Y (2002) Anterior knee laxity in young women varies with their menstrual cycle. Int Orthop 26:154–156
DiBrezzo R, Fort IL, Brown B (1991) Relationships among strength, endurance, weight and body fat during three phases of the menstrual cycle. J Sports Med Phys Fitness 31:89–94
Friden C, Hirschberg AL, Saartok T (2003) Muscle strength and endurance do not significantly vary across 3 phases of the menstrual cycle in moderately active premenopausal women. Clin J Sport Med 13:238–241
Friden C, Hirschberg AL, Saartok T, Backstrom T, Leanderson J, Renstrom P (2003) The influence of premenstrual symptoms on postural balance and kinesthesia during the menstrual cycle. Gynecol Endocrinol 17:433–439
Friden C, Ramsey DK, Backstrom T, Benoit DL, Saartok T, Linden Hirschberg A. (2005) Altered postural control during the luteal phase in women with premenstrual symptoms. Neuroendocrinology 81:150–157
Friden C, Hirschberg AL, Saartok T, Renstrom P (2005) Knee joint kinaesthesia and neuromuscular coordination during three phases of the menstrual cycle in moderately active women. Knee Surg Sports Traumatol Arthrosc [Epub ahead of print]
Heitz NA, Eisenman PA, Beck CL, Walker JA (1999) Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athletic Training 34:144–149
Huston LJ, Greenfield ML, Wojtys EM (2000) Anterior cruciate ligament injuries in the female athlete: potential risk factors. Clin Orthop 372:50–63
Huston LJ, Wojtys EM (1996) Neuromuscular performance characteristics in elite female athletes. Am J Sports Med 24:427–436
Janse de Jonge XA, Boot CR, Thom JM, Ruell PA, Thompson MW (2001) The influence of menstrual cycle phase on skeletal muscle contractile characteristics in humans. J Physiol 530:161–166
Karageanes SJ, Blackburn K, Vangelos ZA (2000) The association of the menstrual cycle with the laxity of the anterior cruciate ligament in adolescent female athletes. Clin J Sport Med 10:162–168
Lee DY, Chai YG, Lee EB, Kim KW, Nah SY, Oh TH, Rhim H (2002) 17 Beta-estradiol inhibits high-voltage-activated calcium channel currents in rat sensory neurons via a non-genomic mechanism. Life Sci 70:2047–2059
Liu SH, Al-Shaikh RA, Panossian V, Finerman GA, Lane JM (1997) Estrogen affects the cellular metabolism of the anterior cruciate ligament. A potential explanation for female athletic injury. Am J Sports Med 25:704–709
McConnell HJ, O’Connor KA, Brindle E, Williams NI (2002) Validity of methods for analyzing urinary steroid data to detect ovulation in athletes. Med Sci Sports Exerc 34:1836–1844
Moller-Nielsen J, Hammar M (1989) Women’s soccer injuries in relation to the menstrual cycle and oral contraceptive use. Med Sci Sports Exerc 21:126–129
Munro CJ, Stabenfeldt GH, Cragun JR, Addiego LA, Overstreet JW, Lasley BL (1991) Relationship of serum estradiol and progesterone concentrations to the excretion profiles of their major urinary metabolites as measured by enzyme immunoassay and radioimmunoassay. Clin Chem 37:838–844
Myklebust G, Maehlum S, Holm I, Bahr R (1998) A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports 8:149–53
Papka RE, Srinivasan B, Miller KE, Hayashi S (1997) Localization of estrogen receptor protein and estrogen receptor mRNA in peripheral autonomic and sensory neurons. Neuroscience 79:1153–1163
Papka RE, Storey-Workley M, Shughrue PJ, Merchenthaler I, Collins JJ, Usip S, Saunders PTK, Shupnik M (2001) Estrogen receptor-ά and -В-immunoreactivity and mRNA in neurons of sensory and autonomic ganglia and spinal cord. Cell Tissue Res 304:193–214
Rozzi SL, Lephart SM, Gear WS, Fu FH (1999) Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J SportsMed 27:312–319
Sarwar R, Niclos BB, Rutherford OM (1996) Changes in muscle strength, relaxation rate and fatigability during the human menstrual cycle. J Physiol 493:267–272
Slauterbeck J, Clevenger C, Lundberg W, Burchfield DM (1999) Estrogen level alters the failure load of the rabbit anterior cruciate ligament. J Orthop Res 17:405–408
Wojtys EM, Huston LJ, Lindenfeld TN, Hewett TE, Greenfield ML (1998) Association between the menstrual cycle and anterior cruciate ligament injuries in female athletes. Am J Sports Med 26:614–619
Wojtys EM, Huston LJ, Boynton MD, Spindler KP, Lindenfeld TN (2002) The effect of the menstrual cycle on anterior cruciate ligament injuries in women as determined by hormone levels. Am J Sports Med 30:182–188
Yu WD, Liu SH, Hatch JD, Panossian V, Finerman GA (1999) Effect of estrogen on cellular metabolism of the human anterior cruciate ligament. Clin Orthop 366:229–238
Yu WD, Panossian V, Hatch JD, Liu SH, Finerman GA (2001) Combined effects of estrogen and progesterone on the anterior cruciate ligament. Clin Orthop 383:268–281
Acknowledgements
This project was funded in part by grants from the Women’s Sports Foundation and the Pennsylvania State University College of Health & Human Development Interdisciplinary Seed Grant Program. The research was carried out in compliance with all laws and regulations governing research involving human subjects in the USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hertel, J., Williams, N.I., Olmsted-Kramer, L.C. et al. Neuromuscular performance and knee laxity do not change across the menstrual cycle in female athletes. Knee Surg Sports Traumatol Arthr 14, 817–822 (2006). https://doi.org/10.1007/s00167-006-0047-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0047-4